Meta-Research: A comprehensive review of randomized clinical trials in three medical journals reveals 396 medical reversals
Figures
Figure 1
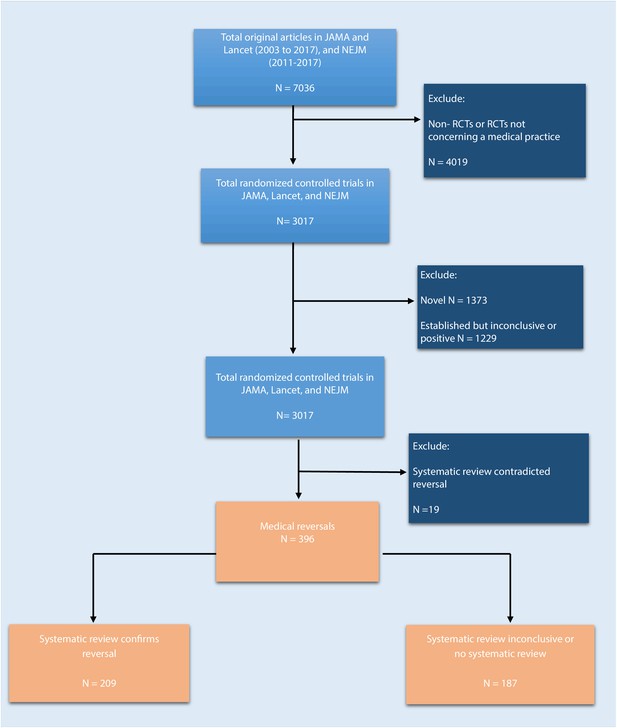
Flowchart of selection process to identify included randomized trials.
https://doi.org/10.7554/eLife.45183.002
Figure 2
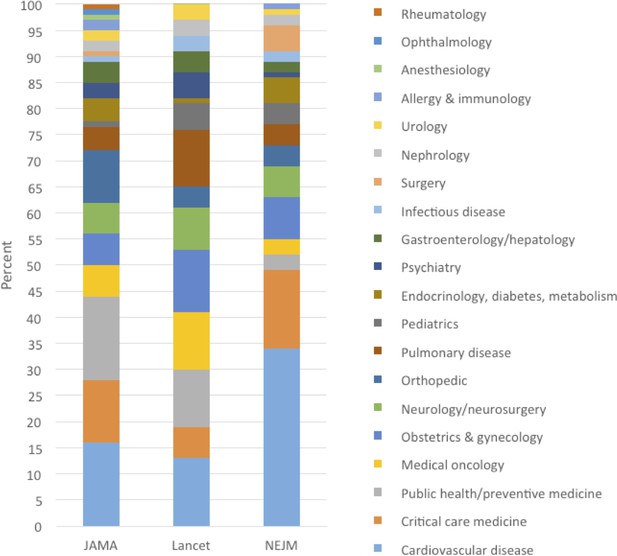
Percent of medical reversals in each medical specialty, by journal: JAMA (2003–2017), Lancet (2003–2017), NEJM (2011–2017).
https://doi.org/10.7554/eLife.45183.004Tables
Table 1
Characteristics of the included reversal studies from JAMA (2003–2017), Lancet (2003–2017), NEJM (2011–2017).
https://doi.org/10.7554/eLife.45183.003| JAMA (n = 154) | Lancet (n = 113) | NEJM (n = 129) | Total (N = 396) | |
|---|---|---|---|---|
| Economic status of studied population | ||||
| High-income | 152 (99%) | 93 (82%) | 121 (94%) | 366 (92%) |
| Low- and middle-income | 2 (1%) | 20 (18%) | 8 (6%) | 30 (8%) |
| Intervention type | ||||
| Medication | 49 (32%) | 36 (32%) | 44 (34%) | 129 (33%) |
| Procedure | 22 (14%) | 22 (19%) | 37 (29%) | 81 (20%) |
| Vitamins/supplements/food | 34 (22%) | 11 (11%) | 8 (6%) | 53 (13%) |
| Device | 15 (10%) | 12 (11%) | 8 (6%) | 35 (9%) |
| System intervention | 13 (8%) | 12 (11%) | 5 (4%) | 30 (8%) |
| Optimize | 5 (3%) | 5 (4%) | 13 (10%) | 23 (6%) |
| Behavioral therapy | 6 (4%) | 4 (4%) | 2 (2%) | 12 (3%) |
| Screening test | 3 (2%) | 4 (4%) | 2 (2%) | 9 (2%) |
| Treatment algorithm | 1 (1%) | 3 (3%) | 5 (4%) | 9 (2%) |
| Diagnostic instrument | 2 (1%) | 2 (1%) | 2 (2%) | 6 (2%) |
| Radiation | 2 (1%) | 1 (1%) | 2 (2%) | 5 (1%) |
| Over-the-counter medication | 2 (1%) | 1 (1%) | 1 (1%) | 4 (1%) |
| Medical Discipline | ||||
| Cardiovascular disease | 21 (14%) | 15 (13%) | 44 (34%) | 80 (20%) |
| Public health/preventive medicine | 32 (20%) | 13 (12%) | 3 (2%) | 48 (12%) |
| Critical care medicine | 18 (12%) | 6 (5%) | 21 (16%) | 45 (11%) |
| Obstetrics and gynecology | 13 (8%) | 13 (12%) | 10 (8%) | 36 (9%) |
| Neurology/neurosurgery | 7 (5%) | 10 (9%) | 8 (6%) | 25 (6%) |
| Oncology | 7 (5%) | 12 (11%) | 4 (3%) | 23 (6%) |
| Orthopedic | 15 (10%) | 5 (4%) | 3 (2%) | 23 (6%) |
| Pulmonary disease | 6 (4%) | 11 (10%) | 5 (4%) | 22 (6%) |
| Pediatrics | 2 (1%) | 6 (5%) | 7 (5%) | 15 (4%) |
| Gastroenterology/hepatology | 6 (4%) | 3 (4%) | 4 (3%) | 13 (3%) |
| Endocrinology, diabetes, metabolism | 7 (5%) | 0 (0%) | 5 (4%) | 12 (3%) |
| Psychiatry | 4 (3%) | 5 (4%) | 1 (1%) | 10 (3%) |
| Nephrology | 4 (3%) | 4 (4%) | 2 (2%) | 10 (3%) |
| Infectious disease | 2 (1%) | 3 (3%) | 3 (2%) | 8 (2%) |
| Surgery | 2 (1%) | 2 (2%) | 4 (3%) | 8 (2%) |
| Urology | 3 (2%) | 3 (3%) | 1 (1%) | 7 (2%) |
| Allergy and immunology | 1 (1%) | 0 (0%) | 2 (2%) | 3 (1%) |
| Anesthesiology | 1 (1%) | 2 (2%) | 1 (1%) | 4 (1%) |
| Rheumatology | 2 (1%) | 0 (0%) | 1 (1%) | 3 (1%) |
| Ophthalmology | 1 (1%) | 0 (0%) | 0 (0%) | 1 (<1%) |
-
Column percentage may not add up to 100% because of rounding.
Table 2
Selected reversal summaries from JAMA (2003–2017), Lancet (2003–2017), NEJM (2011–2017).
https://doi.org/10.7554/eLife.45183.005| RCT and medical discipline | Reversal summary | Systematic review conclusion |
|---|---|---|
| Morris et al. 2016. Immediate delivery compared with expectant management after preterm pre-labour rupture of the membranes close to term (PPROMT trial): a randomized controlled trial. The Lancet 387:444–452. (1/30/2016) [Obstetrics and gynecology] | Both the American College of Obstetricians and Gynecologists and Royal College of Obstetrics and Gynaecology support and/or recommend immediate delivery for women with ruptured membranes who are 34 weeks or greater (Morris et al., 2016). Neonatal infection is a major concern in when there has been a ruptured membrane, especially in premature infants (Merenstein and Weisman, 1996). In this trial, participants assigned to the expectant management group did not have any worse outcomes regarding the primary outcomes of neonatal sepsis (2%; n = 924 in the immediate birth arm vs. 3%; n = 915 in the expectant management arm; RR = 0.8; 95% CI = 0.5–1.3; p=0.37) or neonatal morbidity and mortality (8% vs. 7%; p=0.32) than those assigned to immediate delivery, and had less respiratory distress (p=0.008) and need for mechanical ventilation (p=0.02). This is a reversal of the practice of immediate delivery in women with preterm, pre-labor rupture of the membranes, as it does not lead to less neonatal sepsis. | 2017. Cochrane review. “We found no clinically important difference in the incidence of neonatal sepsis between women who birth immediately and those managed expectantly in PPROM prior to 37 weeks' gestation. Early planned birth was associated with an increase in the incidence of neonatal RDS, need for ventilation, neonatal mortality, endometritis, admission to neonatal intensive care, and the likelihood of birth by caesarean section, but a decreased incidence of chorioamnionitis.” (Bond et al., 2017) |
| Edmond et al. 2015. Effect of early neonatal vitamin A supplementation on mortality during infancy in Ghana (Neovita): a randomised, double-blind, placebo-controlled trial. The Lancet 385:1315–1323. (4/4/2015) [Pediatrics] | Vitamin A deficiency is a public health issue in low-income countries. While multiple trials, including a Cochrane review, have been performed on the effectiveness of vitamin A supplementation in infants in low-income countries, the WHO stated that there was insufficient evidence to make a recommendation on its usage (Gogia and Sachdev, 2011; Imdad et al., 2016). The International Vitamin A Consultative Group (IVACG) supports the use of 50,000 IUs for infants < 6 months of age (Ross, 2002). In this trial based in Ghana, vitamin A supplementation did not lead to a lower mortality rate compared to placebo (24.5/1,000 [n = 11,474] vs. 21.8/1,000 [n = 11,481] supplemented infants; RR1.12; 95% CI = 0.95–1.33; p=0.18), in newborn infants. This is a reversal of the practice of vitamin A supplementation during the early neonatal period in Africa, as it does not improve mortality. | 2017. Cochrane review. “Evidence provided in this review does not indicate a potential beneficial effect of vitamin A supplementation among neonates at birth in reducing mortality during the first six months or 12 months of life.” (Haider and Bhutta, 2017) |
| Conjee et al. 2011. Sertraline or mirtazapine for depression in dementia (HTA-SADD): a randomised, multicentre, double-blind, placebo-controlled trial. The Lancet 378:403–411. (7/30/2011) [Psychiatry] | Sertraline and mirtazapine are commonly prescribed for depression in older adults, and mirtazapine is recommended as a first-line treatment for depression in clinical guidelines, regardless of age (Nelson et al., 2008; Doody et al., 2001; Eccles et al., 1998; National Collaborating Centre for Mental Health, 2007). The results from this trial show that neither sertraline (n = 107; mean difference = 1.17; 95% CI = −0.23 to 2.58; p=0.10) nor mirtazapine (n = 108; mean difference = 0.01; 95% CI = −1.37 to 1.38; p=0.99) improved rates of depression over placebo (n = 111) in those with Alzheimer's disease. This is a reversal of the practice of using traditional treatments for depression, such as sertraline or mirtazapine, in patients with Alzheimer’s, as depression in this population may have different mechanisms than that of the general population. | 2017. “We found no significant drug-placebo difference for depressive symptoms. Overall quality of the evidence was moderate because of methodological limitations in studies and the small number of trials.” (Orgeta et al., 2017) |
| Dennis et al. 2009. Effectiveness of thigh-length graduated compression stockings to reduce the risk of deep vein thrombosis after stroke (CLOTS trial 1): a multicentre, randomised controlled trial. The Lancet 373:1958–1965. (6/9/2009) [Cardiovascular] | Compression therapy was first used by German physicians in the late 19th century when they noticed that superficial vein thromboses disappeared after the use of compression bandages (Galanaud et al., 2013). Compression stockings were used as early as the 1930 s but became widely used after the results of a trial were published in 2000 (Galanaud et al., 2013). National stroke guidelines recommend use of graduated compression stockings (GCS) to reduce risk of deep vein thrombosis (DVT) and pulmonary embolism (Adams et al., 2007) although there is a lack of clinical trials investigating its use in an acute stroke population. This study compared routine care plus GCS (n = 1265) with routine care plus avoidance of GCS (n = 1262) in patients within 1 week of an acute stroke. The study found that there was no difference in occurrence of symptomatic or asymptomatic DVT between groups (126 [10%] in the GCS group vs 133 [10.5%] in the control group) and more adverse events (64 [5%] vs 16 [1%]) in the GCS group. This is a reversal of the use of thigh-length graduated compression stockings to reduce the risk of deep vein thrombosis after stroke. | 2010. Cochrane review. ‘Evidence from randomised trials does not support the routine use of GCS to reduce the risk of DVT after acute stroke.” (Naccarato et al., 2010) However, this RCT was not included in the review. |
| Moss et al. 2006. Effect of mammographic screening from age 40 years on breast cancer mortality at 10 years' follow-up: a randomized controlled trial. The Lancet 368:2053–2060. (12/9/2006) [Public health and general preventive medicine] | In the past, the American Cancer Society recommended that women between the ages of 40 and 49 get mammograms every 1–2 years (American Cancer Society, 2018). However, the benefit of mammograms for women under the age of 50 has not been established. 160 921 women aged 39–41 years old were randomly assigned in the ratio of 1:2 to an intervention group of annual mammography to age 48 or to a control group of usual medical care. At a mean follow-up of 10.7 years, there was no significant difference in breast cancer mortality between the intervention and control groups (relative risk 0.83 [95% CI 0.66–1.04], p=0.11). This is a reversal of the recommendation of mammographic screening every 1–2 years for women ages 40–49. | 2013. Cochrane review. “The chance that a woman will benefit from attending screening is small at best, and - if based on the randomised trials - ten times smaller than the risk that she may experience serious harm in terms of overdiagnosis.” (Gøtzsche and Jørgensen, 2013) |
| Kerr et al. 2003. Intrahepatic arterial versus intravenous fluorouracil and folinic acid for colorectal cancer liver metastases: a multicentre randomised trial. The Lancet 361:368–373. (2/1/2003) [Oncology] | Colon cancer, one of the most common types of cancer, has a relapse rate, after surgery, of about 50%, with the liver being a common site for metastasis (Midgley and Kerr, 1999). Intrahepatic arterial infusion has been used as a method of delivering chemotherapy because it is thought that there would be a higher dose of chemotherapy to cancer cells, while lessoning the side-effects of chemotherapy (Ansfield et al., 1971; Fortner et al., 1984). This trial randomly allocated 290 patients from 16 centers to receive either intravenous chemotherapy (folinic acid 200 mg/m2, fluorouracil bolus 400 mg2 and 22 hr infusion 600 mg/m2, day 1 and 2, repeated every 14 days) or IHA chemotherapy designed to be equitoxic (folinic acid 200 mg/m2, fluorouracil 400 mg/m2 over 15 mins and 22 hr infusion 1600 mg/m2, day 1 and 2, repeated every 14 days). Median survival in the IHA group was 14.7 months and was 14.8 months in the intravenous group (hazard ratio 1.04 [95% CI 0.80–1.33]). This is a reversal of the use of IHA for patients with colorectal cancer liver metastases. | 2011. Cochrane review. “Currently available evidence does not support the clinical or investigational use of fluoropyrimidine-based HAI alone f or the treatment of patients with unresectable CRC liver metastases: in fact, the greater tumor response rate obtained with this HAI regimen does not translate into a survival advantage over fluoropyrimidine alone SCT.” (Mocellin et al., 2009) |
| MUST trial group. 2017. Association Between Long-Lasting Intravitreous Fluocinolone Acetonide Implant vs Systemic Anti-inflammatory Therapy and Visual Acuity at 7 Years Among Patients With Intermediate, Posterior, or Panuveitis. JAMA 317:1993–2005. (5/16/2017) [Ophthalmology] | Noninfectious intraocular inflammation, or uveitis, can lead to visual impairment. Currently, there are two treatments commonly used for uveitis; the first approach is through systemic corticosteroids and corticosteroid-sparing immunosuppressive drugs (Jabs et al., 2005). The other, more recent approach was approved by the FDA in 2005 and involves surgically implanting fluocinolone acetonide implants (Callanan et al., 2008). When systemic therapy (n = 126) and intravitreous implants (n = 129) approaches were compared with one another in a randomized control trial, it was found that after seven years of follow up, those that were randomized to receive implants had poorer visual acuity than the group who were treated with systemic therapy. Change in mean visual acuity from baseline through 7 years was 1.15 in the systemic therapy group and −5.96 in the implant group (between-group difference, −7.12; 95% CI, −12.4 to −2.14; p=0.006). This is a reversal of intravitreous fluocinolone acetonide implants for uveitis. | None found |
| Jakicic et al. 2016. Effect of Wearable Technology Combined With a Lifestyle Intervention on Long-term Weight Loss The IDEA Randomized Clinical Trial. JAMA 316:1161–1171. (9/20/2016) [Public health and general preventive medicine] | Wearable technologies have become increasingly popular as tools to assist in weight loss since they can help track physical activity and estimate calorie burn (Piwek et al., 2016). This clinical trial randomized adults who were participating in a weight-loss program (including a low-calorie diet, increases in physical activity, group counseling sessions, telephone counseling sessions, text message prompts, and access to study materials on a website) to use a wearable device and accompanying web interface (enhanced intervention group, n = 237) or to a self-monitoring website (standard intervention group, n = 233). The study found that the standard intervention group experienced significantly more weight loss than the enhanced intervention group after 24 months (5.9 kg vs 3.5 kg; difference 2.4 kg; 95% CI, 1.0–3.7; p=0.002). This is a reversal of wearable technology for long-term weight loss. | 2017. While this review concluded that wearable technology reduces sedentary behavior, there were no SR/MA on whether these devices reduce weight (Stephenson et al., 2017). This review did not include the RCT. |
| Manson et al. 2013. Menopausal Hormone Therapy and Health Outcomes During the Intervention and Extended Poststopping Phases of the Women’s Health Initiative Randomized Trials JAMA 310:1353–1368. (10/2/2013) [Obstetrics and gynecology] | Postmenopausal hormone replacement therapy (HRT) was initially used in the 1940 s as a way to delay age-related health outcomes, but in the 1970’s studies began to emerge showing that the use of HRT, specifically unopposed estrogen, was associated with endometrial cancer. Progesterone was thought to oppose the effects of estrogen and mitigate the excess risk of cancer, so women began to take them again. By the 1990s, HRTs were the most commonly prescribed medications (Brett and Madans, 1997). The Women’s Health Initiative investigated the effects of HRT in postmenopausal women compared to placebo. This paper is an overview of the many health effects of HRT and found that there is a complex pattern of risks and benefits. The authors concluded that HRT is not an appropriate or recommended intervention for the prevention of chronic disease in postmenopausal women. | 2015. “The current evidence suggests that MHT [menopausal hormone therapy] does not affect the risk of death from all causes, cardiac death and death from stroke or cancer.” (Benkhadra et al., 2015) Another SR/MA (2016) did not find any cardiovascular benefit to hormone therapy (Mahmoodi et al., 2017). |
Siversten et al. 2006. Cognitive Behavioral Therapy vs Zopiclone for Treatment of Chronic Primary Insomnia in Older Adults A Randomized Controlled Trial. JAMA 295:2851–2858. (6/28/2006) [Public health and general preventive medicine] | Insomnia is a common complaint among individuals age 55 years and older and is associated with reduced quality of life, affective disorders, and increased health service utilization (Simon and VonKorff, 1997). Pharmacological interventions are common treatments prescribed by primary care physicians, yet sleep medication has shown to have a small effect size and clinical benefit, and long-term use of the drugs can cause dependency and increased tolerance (Glass et al., 2005). Zopiclone, a non-benzodiazepine sleeping pill, is also associated with next-day sleepiness and traffic collisions (Allain et al., 1991; Montplaisir et al., 2003). Cognitive behavioral therapy (CBT) is the most widely used psychological intervention for insomnia but has limited studies proving its efficacy. This study was the first RCT to compare the effects of nonbenzodiazepine sleep medications with nonpharmacological treatment. The study found that, at 6 months, CBT improved sleep efficiency from 81.4% to 90.1% compared to the zopiclone group, which saw a decrease in efficiency from 82.3% to 81.9%. CBT (n = 18) improved short and long-term sleep outcomes compared to zopiclone and that in most outcomes, zopiclone (n = 16) was no more effective than placebo (n = 12). Zopiclone was no better than placebo in improving symptoms for patients with insomnia. This is a reversal of zopiclone for improving insomnia symptoms. | 2012. “There is moderate grade evidence suggesting CBT-I is superior to the non-benzodiazepines zopiclone and zolpidem for improving sleep measures in the short term.” (Mitchell et al., 2012) |
| Hallstrom et al. 2006. Manual Chest Compression vs Use of an Automated Chest Compression Device During Resuscitation Following Out-of-Hospital Cardiac Arrest: A Randomized Trial. JAMA 295:2620–2628. (6/14/2006) [Cardiovascular] | Out-of-hospital cardiac arrest is generally treated by cardiopulmonary resuscitation (CPR) and the quality and order of resuscitation intervention may have an effect on cardiac and neurological outcomes (Steen et al., 2003). Consistent compressions in CPR is difficult while maintaining quality, and paramedics have been shown to provide shallower, slower compressions over time (Ochoa et al., 1998). Manual chest compression devices were designed to provide ideal chest compressions. The AutoPulse Resuscitation System is a load-distributing band circumferential chest compression device (LDB-CPR) that received marketing clearance by the FDA in 2002 (Food and Drug Administration, 2019). This study compared the use of an LDB-CPR device with manual CPR in EMS care for patients with cardiac arrest that was presumed to be of cardiac origin and that had occurred prior to the arrival of EMS personnel. Automated LDB-CPR devices (n = 394) were associated with worse neurological outcomes and showed a trend toward worse survival compared to manual CPR (n = 373). Comparing LDB-CPR to manual CPR, survival to hospital discharge was 5.8% vs 9.9% (p=0.06). The two best cerebral performance categories at hospital discharge were recorded in 3.1% of LDB-CPR patients compared to 7.5% of manual CPR patients (p=0.006). This is a reversal on the use of automated chest compression devices for resuscitation following out-of-hospital cardiac arrest. | 2014. Cochrane review. “Widespread use of mechanical devices for chest compressions during cardiac events is not supported by this review. More RCTs that measure and account for the CPR process in both arms are needed to clarify the potential benefit to be derived from this intervention.” (Brooks et al., 2011) |
Harris et al. 2013. Universal Glove and Gown Use and Acquisition of Antibiotic-Resistant Bacteria in the ICU A Randomized Trial. JAMA 310:1571–1580. (10/16/2013) [Critical care] | The emergence of antibiotic-resistant bacteria has become a serious public health issue. To help prevent the spread of these organisms, policies recommending contact precautions (e.g. gloves and gowns) were made by the Centers for Disease Control and Prevention (Manian and Ponzillo, 2007). In this trial, intensive care units (ICUs) were randomized to usual care of ICUs (N = 10) or a protocol where all health care workers are required to wear gloves and gowns for all patient contact (intervention ICUs; N = 10). There was no difference in the acquisition of methicillin-resistant Staphylococcus aureus or vancomycin-resistant Enterococcus between ICUs that had universal glove and gown use and those that did not (difference, −1.71 acquisitions per 1000 person-days, 95% CI, −6.15 to 2.73; p=0.57). This is a reversal of requiring that all health care workers in ICUs wear gloves and gowns for all patient contact and when entering a patient room. | 2014. ‘Contact precautions did not significantly reduce the VRE acquisition rate.” (De Angelis et al., 2014) This review did not include the RCT. |
| Binanay et al. 2005. Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness: The ESCAPE Trial. JAMA 294:1625–1633. (10/5/2005) [Cardiovascular] | Pulmonary artery catheterization (PAC) was introduced in the 1970 s and was adopted nationwide in the ICU and perioperative settings for congestive heart failure (Gore et al., 1987). Although therapies have improved over the years, patients with heart failure still have up to 35–40% one-year mortality rates (Lee et al., 2003). PAC has been questioned for its safety and efficacy. This study investigated the survival rate of patients after PAC (n = 206) or clinical assessment alone (n = 207). They found that PAC increased adverse events (21.9% PAC vs 11.5% clinical assessment; p=0.04) and had no effect on days alive out of the hospital during the first 6 months (133 vs 135 days; HR, 1.00; 95% CI, 0.82–1.21; p=0.99), overall mortality (10% vs 9%; OR, 1.26; 95% CI, 0.78–2.03; p=0.35), and number of days hospitalized (8.7 vs 8.3; HR, 1.04; 95% CI, 0.86–1.27; p=0.67). This is a reversal of PAC for patients with congestive heart failure. | 2013. Cochrane review. “PAC is a diagnostic and haemodynamic monitoring tool but not a therapeutic intervention. Our review concluded that use of a PAC did not alter the mortality, general ICU or hospital LOS, or cost for adult patients in intensive care.” (Rajaram et al., 2013) |
| Schoor et al. 2003. Prevention of Hip Fractures by External Hip Protectors A Randomized Controlled Trial. JAMA 289:1957–1962. (4/16/2003) [Orthopedic] | Hip fractures affect millions of people annually and external hip protectors were designed to absorb the impact of a fall to prevent fractures. There were a number of RCTs investigating external hip protectors and hip fracture prevention showing with mixed results, (Chan et al., 2000; Lauritzen et al., 1993; Parker et al., 2005) yet protectors were still regularly prescribed in practices (van Schoor et al., 2002). This study found that prescribing a hip protector was not effective in preventing hip fractures in elderly persons aged 70 years and older compared to risk and bone health information. There were 18 fractures in the intervention group (n = 276) compared to 20 fractures in the control group (n = 285; p=0.86). This is a reversal of external hip protectors for preventing fractures in elderly persons in institutional homes. | 2014. Cochrane review. After excluding studies with high risk of bias, this Cochrane systematic review found that hip protectors did not have a significant effect on risk of hip fractures in institutional settings (Santesso et al., 2014). |
| Coleman et al. 2012. A Randomized Trial of Nicotine-Replacement Therapy Patches in Pregnancy. NEJM 366:808–818. (3/1/2012) [Obstetrics and gynecology] | Cigarette smoking during pregnancy increases the risks of pregnancy complications, as well as the chance of delivering a low-birth-weight or preterm baby. Despite these risks, approximately 6% to 22% of pregnant women in high-income countries smoke, making cigarette smoking one of the leading causes of adverse pregnancy outcomes (Cnattingius, 2004). Behavioral counseling is recommended for pregnant smokers, (Lumley et al., 2009) as is nicotine-replacement therapy, which is recommended by several guidelines (Coleman et al., 2012a). In the SNAP trial (N = 1050), pregnant smokers receive behavioral counseling and were randomly assigned to either a standard course of nicotine patches or placebo. In this trial, it was found that a nicotine patch was no more effective than placebo in helping pregnant women to quit smoking(9.4% and 7.6%, respectively; unadjusted odds ratio with nicotine-replacement therapy, 1.26; 95% confidence interval, 0.82 to 1.96). This is a reversal on nicotine replacement therapy patches in pregnancy. | 2015. Cochrane review. "NRT [Nicotine Replacement Therapy] used in pregnancy for smoking cessation increases smoking cessation rates measured in late pregnancy by approximately 40%. There is evidence, suggesting that when potentially-biased, non-placebo RCTs are excluded from analyses, NRT is no more effective than placebo. There is no evidence that NRT used for smoking cessation in pregnancy has either positive or negative impacts on birth outcomes (Coleman et al., 2012b). |
| Nicolaides et al. 2016. A Randomized Trial of a Cervical Pessary to Prevent Preterm Singleton Birth. NEJM 374:1044–1052. (3/17/2016) [Obstetrics and gynecology] | The transvaginal placement of a silicone pessary is often recommended for pregnant women with a short cervix given their increased risk of spontaneous delivery prior to 34 weeks of gestation. It is believed that this device reduces direct pressure on the cervix and prolongs pregnancy (Arabin et al., 2003). This randomized trial compared spontaneous preterm births among women with pessaries with those who underwent expectant management and found that the pessary had no significant effect on the rate of preterm delivery (12.0% and 10.8%, respectively; odds ratio in the pessary group, 1.12; 95% confidence interval, 0.75 to 1.69; p=0.57). This is a reversal on a cervical pessary to prevent preterm singleton birth of women 16 years or older with a cervical length of 25 mm or less. | 2017. “In singleton pregnancies with a [transvaginal ultrasound cervical length] TVU CL ≤ 25 mm at 200–246 weeks, the Arabin pessary does not reduce the rate of spontaneous preterm delivery or improve perinatal outcome.” Saccone et al., 2017 |
| Shroyer et al. 2017. Five-Year Outcomes after On-Pump and Off-Pump Coronary-Artery Bypass NEJM 377:623–632. (8/17/2017) [Cardiovascular] | Observational studies in the 1990s showed an association between off-pump coronary-artery bypass and better early clinical outcomes compared to on-pump, and the practice of performing coronary-artery bypass surgery on a beating heart repopularized (Cleveland et al., 2001). Yet randomized controlled trials have not been able to show efficacy in off-pump surgeries and suggested that incomplete revascularization was more frequent with off-pump surgery (Hattler et al., 2012). This follow-up study (n = 2203) found that 5 year outcomes of death from any cause (relative risk, 1.28; 95% confidence interval [CI], 1.03–1.58; p=0.02) and any major adverse cardiovascular events (relative risk, 1.14; 95% CI, 1.00–1.30; p=0.046) were worse for patients who underwent coronary-artery bypass surgery off-pump compared to on-pump. This is a reversal of off-pump coronary-artery bypass. | 2018. “This meta-analysis represents a comprehensive summary of RCTs comparing OPCABG to ONCABG. Our results showed that OPCABG was associated with no reduction in operative risk, an excess mortality at follow-up ≥3 years, and a trend toward higher risk of repeated revascularization.’ (Gaudino et al., 2018) |
| Friedly et al. 2014. A Randomized Trial of Epidural Glucocorticoid Injections for Spinal Stenosis. NEJM 374:11–21. (7/3/2014) [Neurology] | The treatment of symptomatic lumbar stenosis has included epidural glucocorticoid injections (Harrast, 2008). This treatment is frequently prescribed by physicians to treat lumbar stenosis and other conditions, with an estimated 25% of the Medicare population and 74% of patients at the Veteran’s Administration being prescribed this treatment. As the usage of glucocorticoid injections increased to treat various ailments, so did the cost. From 1994 to 2001 there was a 271% growth in usage of the treatment, and the cost went from $24 million to over $175 million (Friedly et al., 2007). The LESS trial (N = 441) was designed to compare the effectiveness of epidural injections of glucocorticoids plus anesthetic vs. injections of anesthetic alone. At six weeks after randomization, there were no significant differences in RMDQ scores (used to measure functional disability), (adjusted difference in the average treatment effect between the glucocorticoid–lidocaine group and the lidocaine-alone group, −1.0 points; 95% confidence interval [CI], −2.1 to 0.1; p=0.07), or pain intensity, (adjusted difference in the average treatment effect, −0.2 points; 95% CI, −0.8 to 0.4; p=0.48), between the patients treated with glucocorticoids plus lidocaine and those in the lidocaine alone group. This is a reversal of administering epidural glucocorticoid injections in patients who have lumbar central spinal stenosis and moderate-to-severe leg pain and disability. | 2015. AHRQ. “Evidence was limited for epidural corticosteroid injections versus placebo interventions for spinal stenosis (SOE: low to moderate) or nonradicular back pain (SOE: low), but showed no differences in pain, function, or likelihood of surgery.” (Chou, 2015)Møller et al., 2012 |
| Lamy et al. 2016. Five-Year Outcomes after Off-Pump or On-Pump Coronary-Artery Bypass Grafting. NEJM 375:2359–2368. (12/15/2016) [Cardiovascular] | Coronary-artery bypass grafting (CABG) can be performed either with a still heart (on-pump CABG) or without a cardiopulmonary bypass on the beating heart (off-pump). Traditionally, surgeons performed surgery on the arrested heart, on-pump CABG, which allowed for increased surgical precision (Shroyer et al., 2009). However, surgeons grew concerned that the cross clamping of the aorta, necessary for the on-pump CABG procedure, may be harmful to patients and increase mortality and risk of stroke or other systemic embolic events in these patients. The off-pump method, operating on a beating heart, was developed to decrease the perioperative risks (Grover, 2012). However, the clinical literature reported different results about the relative efficacy of off-pump CABG as compared with on-pump CABG (Lamy et al., 2012). The CORONARY trial (n = 4752) compared on-pump and off-pump CABG surgery in patients with coronary heart disease. This follow up study on the results of the CORONARY trial found the after 4 years, patients who underwent on-pump and off-pump CABG has similar rates of outcomes of death, stroke, myocardial infarction, renal failure, and repeat revascularization (23.1%% and 23.6%, respectively; hazard ratio with off-pump CABG, 0.98; 95% confidence interval [CI], 0.87–1.10; p=0.72). The costs between the two treatments was similar as well. This is a reversal of off-pump coronary-artery bypass grafting. | 2018. “Off-pump CABG increases long-term (≥5 years) mortality compared with on-pump CABG, based on a meta-analysis of eight medium- to large-size RCTs enrolling a total 8780 patients.’ (Takagi et al., 2017) 2012. Cochrane review. "Our systematic review did not demonstrate any significant benefit of off-pump compared with on-pump CABG regarding mortality, stroke, or myocardial infarction. In contrast, we observed better long-term survival in the group of patients undergoing on-pump CABG with the use of cardiopulmonary bypass and cardioplegic arrest. Based on the current evidence, on-pump CABG should continue to be the standard surgical treatment. However, off-pump CABG may be acceptable when there are contraindications for cannulation of the aorta and cardiopulmonary bypass. Further randomised clinical trials should address the optimal treatment in such patients." (Møller et al., 2012) This review precedes study. |
Katz et al. 2013. Surgery versus Physical Therapy for a Meniscal Tear and Osteoarthritis. NEJM 368:1675–1684. (5/2/2013) [Orthopedic] | Clinicians who suspect a tear in the meniscus may refer patients either to a surgeon for arthroscopic partial meniscectomy or to physical therapy. This procedure is frequently done in the United States; one estimate is that more than 465,000 patients receive this procedure annually (Bozic et al., 2012). Given the frequency and cost of arthroscopic partial meniscectomy and lack of concrete evidence on the clinical benefit of the procedure, the METEOR trial was designed to assess the efficacy of arthroscopic partial meniscectomy surgery as compared with a physical-therapy for increasing physical function of patients with a meniscal tear and moderate osteoarthritis (Katz et al., 2013). METEOR found that there was not a significant decrease in the WOMAC score—a measure of physical function in which a higher score means worse physical function—between the patients undergoing surgery and those receiving initial physical therapy. The WOMAC score after 6 months was 20.9 points (95% confidence interval [CI], 17.9 to 23.9) in the surgical group and 18.5 (95% CI, 15.6 to 21.5) in the physical-therapy group (mean difference, 2.4 points; 95% CI, −1.8 to 6.5). The authors conclude that the finding of the METEOR trial advocates for an initial nonoperative strategy for treatment. This is a reversal of surgery for a meniscal tear detected on magnetic resonance imaging (MRI) and osteoarthritis in patients 45 year of age or older. | 2016. “Further evidence is required to determine which patient groups have good outcomes from each intervention. Given the current widespread use of arthroscopic meniscal surgeries, more research is urgently needed to support evidence-based practice in meniscal surgery in order to reduce the numbers of ineffective interventions and support potentially beneficial surgery.” (Monk et al., 2017) |
Additional files
-
Supplementary file 1
Funding sources for articles in which a medical reversal was identified.
- https://doi.org/10.7554/eLife.45183.006
-
Supplementary file 2
Reversal summaries identified, by journal.
- https://doi.org/10.7554/eLife.45183.007
-
Transparent reporting form
- https://doi.org/10.7554/eLife.45183.008
Download links
A two-part list of links to download the article, or parts of the article, in various formats.
Downloads (link to download the article as PDF)
Open citations (links to open the citations from this article in various online reference manager services)
Cite this article (links to download the citations from this article in formats compatible with various reference manager tools)
Meta-Research: A comprehensive review of randomized clinical trials in three medical journals reveals 396 medical reversals
eLife 8:e45183.
https://doi.org/10.7554/eLife.45183





