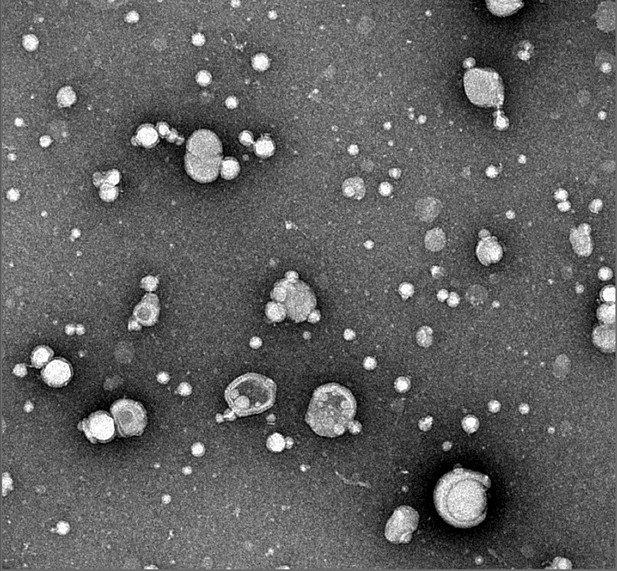
Vesicles of lipid membranes that have been modified by two ancient proteins, known as SAA and sPLA2. Image credit: Shobini Jayaraman and Donald L. Gantz (CC BY 4.0)
Cell boundaries are made up of fatty substances known as lipids. When cells get severely damaged, their lipid membranes break apart. These broken fragments of membrane become highly toxic, and must be removed as soon as possible to allow the tissue to heal. A small protein called serum amyloid A, SAA for short, was recently proposed to play a pivotal role in this process. In humans, SAA levels in the blood rapidly spike to over a thousand times their normal level following inflammation, injury or infection. Combined with the fact SAA has been conserved for over 500 million years, this suggests that SAA must be important for survival. But, it is not entirely clear how this protein works.
One clue for how SAA works is its relationship to another ancient protein called secretory phospholipase A2. This protein, also known as sPLA2, is part of a big family of enzymes that break down lipids in the cell membrane. Notably, sPLA2 levels rise at the same time and place as SAA during inflammation. This led Jayaraman et al. to ask whether SAA and sPLA2 might be working together to clean up the cell membrane debris.
To find out, Jayaraman et al. mixed mouse SAA with vesicles of membrane lipids, and then added sPLA2. This revealed that SAA reshapes the lipid membrane into smaller ‘nanoparticles’ with tightly curved surfaces that are easier for sPLA2 to break down. As the sPLA2 breaks up these particles, SAA then gathers up and gets rid of the leftover toxic fragments. This suggests that SAA has two roles: helping sPLA2 break down the membrane, and removing any toxic debris.
Clearing debris after injury is essential for proper healing. So, understanding how it works is crucial to find new ways to treat inflammation. Further work to understand SAA and sPLA2 could improve our understanding of how to treat acute and chronic inflammation and its life-threatening complications.




