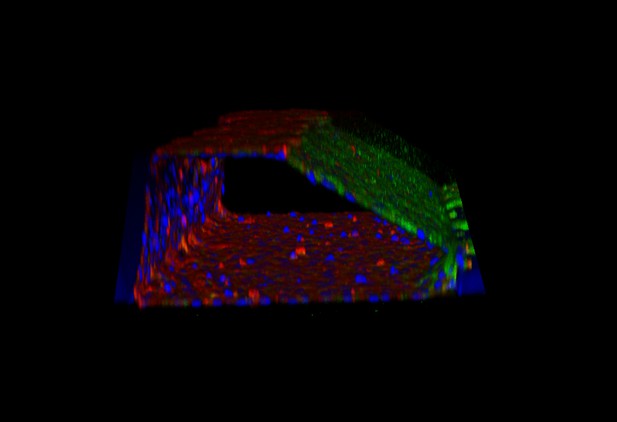
A 3D reconstruction of a human blood vessel. Image credit: Junaid et al. (CC BY 4.0)
In a range of conditions called autoimmune diseases, the immune system attacks the body rather than foreign elements. This can cause inflammation that is harmful for many organs. In particular, immune cells can produce excessive amounts of a chemical messenger called tumor necrosis factor alpha (TNFα for short), which can lead to the release of fatty molecules that damage blood vessels.
This process is normally studied in blood vessels cells that are grown on a dish, without any blood movement. However, in this rigid 2D environment, the cells become ‘stressed’ and show higher levels of inflammation than in the body. This makes it difficult to assess the exact role that TNFα plays in disease.
A new technology is addressing this issue by enabling scientist to culture blood vessels cells in dishes coated with gelatin. This allows the cells to organize themselves in 3D, creating tiny blood vessels in which fluids can flow. However, it was unclear whether these ‘microvessels-on-a-chip’ were better models to study the role of TNFα compared to cells grown on a plate.
Here, Junaid et al. compared the levels of inflammation in blood vessels cells grown in the two environments, showing that cells are less inflamed when they are cultured in 3D. In addition, when the artificial 3D-blood vessels were exposed to TNFα, they responded more like real blood vessels than the 2D models. Finally, experiments showed that it was possible to monitor the release of fatty molecules in this environment. Together, this work suggests that microvessels-on-a-chip are better models to study how TNFα harms blood vessels.
Next, systems and protocols could be develop to allow automated mass drug testing in microvessels-on-a-chip. This would help scientists to quickly screen thousands of drugs and find candidates that can protect blood vessels from TNFα.




