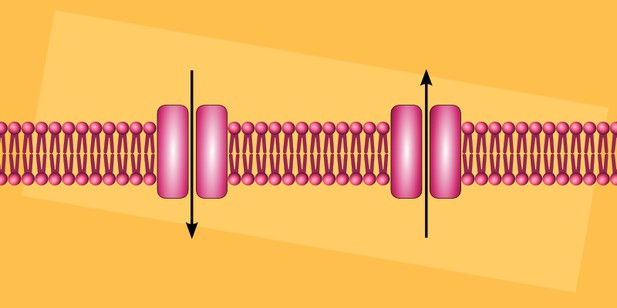
Schematic of ion channels. Image credit: Adapted from work by Peter Duncan (CC BY-SA 4.0)
Inherited brain disorders often cause severe problems for those affected by them. One example is a group of diseases, collectively termed “developmental and epileptic encephalopathies”, or DEE for short. People with these diseases usually have both epilepsy and intellectual disabilities, and in some patients these conditions are associated with two mutations that change a gene called TRPM3.
The TRPM3 gene encodes a protein called an ion channel. Ion channels form pores on the surfaces of cells. When channels are active, the pores open, allowing charged particles – which, in the case of TRPM3, are sodium and calcium ions – to pass through, carrying tiny electrical currents. In the nervous system, ion channels help nerve cells communicate and also allow them to sense changes in the environment.
The TRPM3 channel is known to open in response to heat and certain chemical “activators”. In mice, TRPM3 is found in sensory nerve cells, where it acts as a heat sensor. Although altering TRPM3 in mice affects their ability to sense intense or painful heat stimuli, they are otherwise completely normal and have no symptoms resembling human DEE disorders.
Although TRPM3 is found in the human brain, little is known about its role there or what effects the DEE-associated mutations have on its activity. Zhao et al. therefore set out to determine, whether each of the mutation was a ‘loss of function’, meaning that it stopped the channel from opening, or a ‘gain of function’, meaning it made the channel open more often.
Frog egg cells and mammalian cells grown in the laboratory were engineered to produce the TRPM3 ion channel. Measurements of electrical activity on these cells revealed that the two mutations seen in people with DEE were both ‘gain of function’. Both mutants were more sensitive to heat and chemical activators than the normal protein. They were also more active overall, even without any stimuli. However, one mutation had a greater effect on heat sensitivity, while the other caused a larger increase in chemical-induced activity.
Imaging experiments revealed that both mutant channels also increased the amount of calcium inside the cells. This could explain why the mutations cause disease, since abnormally high calcium levels can damage nerve cells. In addition, the epilepsy drug primidone switched off the mutant channels, pointing to potential treatment of this disease using primidone.




