Infectious Diseases: Mathematics and malaria
Parasites are a lot like teenagers. Take a few hundred adolescents in school, each with unique genetic and cultural influences, and you would expect to see huge diversity in behaviour. Instead, we generally find that teenagers fall into one of a small number of groups that have their own distinct identities and patterns of behaviour (or misbehaviour). Similarly, the genetic make-up of Plasmodium falciparum, the parasite that causes most fatal malaria cases, suggests that many different strains of malaria should exist in a host population: in reality, however, only a small number of strains, each with distinctive clinical and epidemiological features, are observed. Peer pressure is the driving force for a finite set of teenager behaviours (Brown et al., 1986), and the immune response of humans appears to be the driving force for the same effect in many pathogens.
Malaria, which arises from P. falciparum carried by mosquitos, is thought to kill more than a million people a year and to infect many more. P. falciparum causes malaria by entering red blood cells and releasing antigens that change the surfaces of the cells; these infected cells then accumulate in the brain and various small blood vessels. The virulence of P. falciparum is believed to arise from its ability to evade the human immune system by changing the antigens that are released. Many important pathogens, including P. falciparum, constantly exchange genetic material: however, the number of strains of malaria (and other diseases) is much lower than expected, given the level of genetic exchange that happens. This has led to ‘strain theory’—the idea that populations of parasites are restricted to specific subtypes (that is, different strains) as a result of their interactions with human immunity (Gupta et al., 1994, 1996). Now, writing in eLife, Yael Artzy-Randrup and co-workers at the University of Michigan, New York University and Princeton University extend strain theory and conclude that immune selection markedly influences populations of P. falciparum, restricting their diversity to a finite number of antigenic strains (Artzy-Randrup et al., 2012).
They focus on the family of 50–60 var genes that code for the PfEMP1 antigens that are central to malarial disease. Each parasite expresses a single var gene at a time, while the rest remain transcriptionally silent. However, as the hosts develop antibodies against the single antigen that is being produced, small sub-populations of P. falciparum begin to produce other types of antigens so as to re-establish the infection. Artzy-Randrup and co-workers developed an ‘agent-based model’ to describe interactions between parasites and humans through simple mathematical rules that quantify genetic and epidemiological processes (Bauer et al., 2009).
The team's model predicts that host immune selection can cause the local P. falciparum population to self-organise into a finite number of strains (see Figure 1), with the degree of genetic overlap between the strains (defined as the number of common var alleles) depending on the transmission intensity (defined as the number of bites per year). The strains do not, in general, have common var alleles, but partially overlapping var alleles can arise when the transmission intensity is high, as it is in many parts of Africa. High transmission intensities also lead to immunity being established in humans at earlier ages than happens in areas with lower transmission intensities, such as parts of Asia: the proportion of people who become immune is also higher in areas with high transmission intensities. The changes in the parasite population appear to be mostly a product of the traits of immune response of humans, while ‘neutral’ factors, such as genetic recombination from random mating, appear to have much less influence.
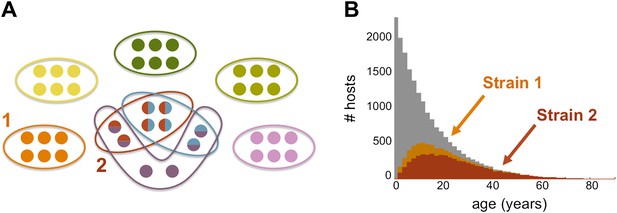
The genome of P. falciparum contains between 50 and 60 var genes that code for different antigens, all of which can lead to malaria. Despite this diversity, only a relatively small number of strains of malaria become established in any population: moreover, these strains tend to have little or no genetic overlap with each other. (A) This illustration (created by Artzy-Randrup et al. and motivated by real data) shows how 40 var genes (circles) can lead to 8 different strains of P. falciparum malaria (each composed of a subset of 6 genes). Five of these strains are unique as they do not genetically overlap with any of the other strains; two strains (shown in red and light blue) share all of their genes with other strains, and one strain (shown in purple) shares four of its genes with other strains. (B) The number of hosts immune to two strains of malaria versus age: strain 1 (orange) is genetically unique, so immunity to this strain is gained only through exposure to it; strain 2 (red) shares genes with other strains of malaria, so immunity to this strain can be acquired through exposure to it and also through exposure to two other strains of malaria. Immunity to strain 1 is higher than for strain 2 as human hosts are exposed to strain 1 at a higher level and at younger ages than strain 2. The grey bars show the host age distribution.
FIGURE: ARTZY-RANDRUP ET AL.
It has long been recognized that malaria infection in humans varies greatly from place to place, and it has been assumed that these differences arise from biological differences in otherwise morphologically similar parasites. As early as 1910, Ronald Ross—the British doctor who won the Nobel Prize in Physiology or Medicine in 1902 for demonstrating that mosquitos transmit the parasites that cause malaria—had noted different types of fever in malaria patients. Then, in work that was just as influential as the work that won him the Nobel Prize, Ross developed mathematical models to describe the spread of malaria (Ross, 1916), which eventually paved the way for the spraying-based strategies that have been widely used in an effort to stop the spread of the disease (see McKenzie et al., 2008 for an historical review).
The biological differences in P. falciparum presumably lead to large variations in its ability to infect mosquitos (only some species of mosquitoes can acquire the parasite), in the patterns of human infection, and in its susceptibility to drugs (Snow et al., 2012). The suggestion by Artzy-Randrup et al. that lower intensity transmission is linked with loss of immunity might be consistent with recent findings from India which suggest that malaria kills substantial numbers of rural adults who lack access to curative therapies (Dhingra et al., 2010).
Mosquito nets treated with insecticides, spraying insecticides inside houses and, most importantly, drugs (notably artemisinin-combination therapies) have proved to be powerful tools in the fight against malaria (Breman et al., 2006). Strain theory suggests that vaccines should be possible, but an effective malaria vaccine has yet to be found: indeed, a recent trial of the RTS,S/AS01 vaccine found that it provided only ‘modest protection against both clinical and severe malaria in young infants’ (The RTS,S clinical trials partnership, 2012).
Malaria is increasingly the subject of attention around the world, and a better understanding of the basic biologic processes involved will be central to developing the tools which can better control this lethal, but curable disease. More than a century after the pioneering work of Ross, malaria still presents a formidable challenge to medical science.
References
-
Agent-based modeling of host–pathogen systems: the successes and challengesInf Sci (Ny) 179:1379–1389.
-
BookChapter 21: Conquering malariaIn: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, Jha P, Mills A, Musgrove P, editors. Disease control priorities in developing countries (2nd Ed). Washington, DC: World Bank. pp. 413–432.
Article and author information
Author details
Publication history
Copyright
© 2012, Jha
This article is distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use and redistribution provided that the original author and source are credited.
Metrics
-
- 726
- views
-
- 59
- downloads
-
- 1
- citations
Views, downloads and citations are aggregated across all versions of this paper published by eLife.
Download links
Downloads (link to download the article as PDF)
Open citations (links to open the citations from this article in various online reference manager services)
Cite this article (links to download the citations from this article in formats compatible with various reference manager tools)
Further reading
-
- Microbiology and Infectious Disease
Understanding the interplay between the HIV reservoir and the host immune system may yield insights into HIV persistence during antiretroviral therapy (ART) and inform strategies for a cure. Here, we applied machine learning (ML) approaches to cross-sectional high-parameter HIV reservoir and immunology data in order to characterize host–reservoir associations and generate new hypotheses about HIV reservoir biology. High-dimensional immunophenotyping, quantification of HIV-specific T cell responses, and measurement of genetically intact and total HIV proviral DNA frequencies were performed on peripheral blood samples from 115 people with HIV (PWH) on long-term ART. Analysis demonstrated that both intact and total proviral DNA frequencies were positively correlated with T cell activation and exhaustion. Years of ART and select bifunctional HIV-specific CD4 T cell responses were negatively correlated with the percentage of intact proviruses. A leave-one-covariate-out inference approach identified specific HIV reservoir and clinical–demographic parameters, such as age and biological sex, that were particularly important in predicting immunophenotypes. Overall, immune parameters were more strongly associated with total HIV proviral frequencies than intact proviral frequencies. Uniquely, however, expression of the IL-7 receptor alpha chain (CD127) on CD4 T cells was more strongly correlated with the intact reservoir. Unsupervised dimension reduction analysis identified two main clusters of PWH with distinct immune and reservoir characteristics. Using reservoir correlates identified in these initial analyses, decision tree methods were employed to visualize relationships among multiple immune and clinical–demographic parameters and the HIV reservoir. Finally, using random splits of our data as training-test sets, ML algorithms predicted with approximately 70% accuracy whether a given participant had qualitatively high or low levels of total or intact HIV DNA . The techniques described here may be useful for assessing global patterns within the increasingly high-dimensional data used in HIV reservoir and other studies of complex biology.
-
- Microbiology and Infectious Disease
Antibiotic tolerance in Mycobacterium tuberculosis reduces bacterial killing, worsens treatment outcomes, and contributes to resistance. We studied rifampicin tolerance in isolates with or without isoniazid resistance (IR). Using a minimum duration of killing assay, we measured rifampicin survival in isoniazid-susceptible (IS, n=119) and resistant (IR, n=84) isolates, correlating tolerance with bacterial growth, rifampicin minimum inhibitory concentrations (MICs), and isoniazid-resistant mutations. Longitudinal IR isolates were analyzed for changes in rifampicin tolerance and genetic variant emergence. The median time for rifampicin to reduce the bacterial population by 90% (MDK90) increased from 1.23 days (IS) and 1.31 days (IR) to 2.55 days (IS) and 1.98 days (IR) over 15–60 days of incubation, indicating fast and slow-growing tolerant sub-populations. A 6 log10-fold survival fraction classified tolerance as low, medium, or high, showing that IR is linked to increased tolerance and faster growth (OR = 2.68 for low vs. medium, OR = 4.42 for low vs. high, p-trend = 0.0003). High tolerance in IR isolates was associated with rifampicin treatment in patients and genetic microvariants. These findings suggest that IR tuberculosis should be assessed for high rifampicin tolerance to optimize treatment and prevent the development of multi-drug-resistant tuberculosis.





