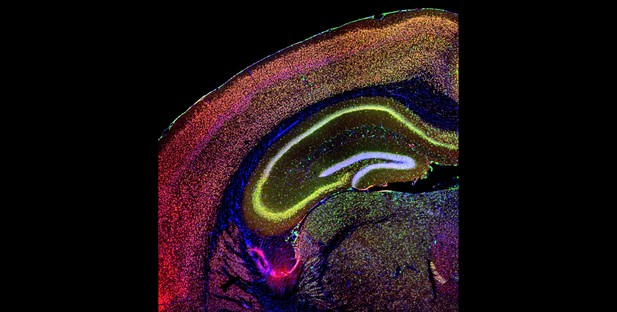
Brain image from a mouse model of 22q11.2 deletion syndrome in which antisense oligonucleotides (green and yellow) have been introduced. Image Credit: Pratibha Thakur and Martin Lackinger (CC BY 4.0)
Our genetic material is ‘packaged’ into chromosomes, which are compact structures made of DNA found in every cell. Chromosomal abnormalities occur either when a person has the wrong number of chromosomes, or when parts of a chromosome are deleted or duplicated. This can cause a wide range of health problems, including psychiatric and cognitive symptoms.
Individuals with ‘22q11.2 deletion syndrome’ are missing a small DNA segment DNA on chromosome 22. This results in cognitive impairment and a high risk of disorders like schizophrenia. Recent research in mice has shown that the DNA deletion in 22q11.2 deletion syndrome disrupts tiny molecules called microRNAs, which help control the activity of many genes (usually by ‘switching’ them off).
The gene for EMC10 is affected by these changes in microRNAs. Normally, the EMC10 protein plays a role in maintaining the health of brain cells. However, further studies in mice have shown that a DNA deletion equivalent to the one in humans with 22q11.2 deletion syndrome leads to excessive production of EMC10 – suggesting that too much EMC10 can be harmful. Reducing the amount of EMC10 in these mice restored normal brain function and behaviour.
Based on these results, Thakur, Lackinger et al. investigated if the same connection between disrupted microRNAs and abnormally high EMC10 levels also occurred in humans with 22q11.2 deletion syndrome. Analysis of cultured brain cells derived from patients with the condition confirmed that problems similar to those previously observed in mice emerged: disruption of microRNAs led to the cells accumulating too much EMC10, resulting in abnormal cell behaviour such as defective growth.
Thakur, Lackinger et al. then tested if gene-targeting tools called antisense oligonucleotides (ASOs) could be used to treat 22q11.2 syndrome. Similarly to microRNAs, ASOs work by turning off specific genes. When adult mice with the deletion were given ASOs targeting the gene for EMC10, their levels of EMC10 protein decreased, and their ‘cognitive function’ (including performance in simple memory tests) improved. Importantly, these benefits lasted over two months after a single treatment.
These results shed new light on the molecular mechanisms behind the effects of 22q11.2 deletion in humans. They also highlight ASOs targeting the EMC10 gene as a potential treatment for the condition, even when treatment begins in adulthood. In the future, Thakur, Lackinger et al. hope that this work will help to develop therapies that improve quality of life for those affected by the syndrome.




