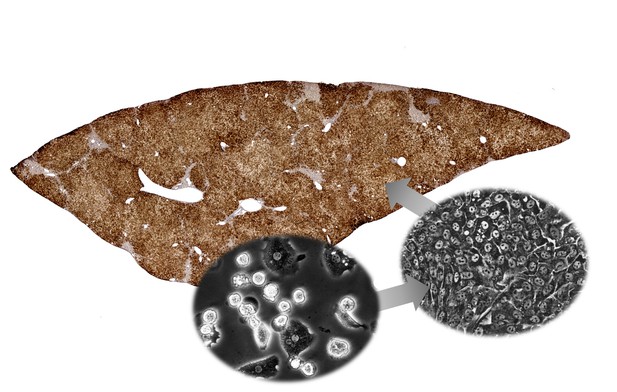
Human infant liver cells (left hand circle) were converted into cells known as human CLiPs (right hand circle), which when transplanted can replace the damaged liver cells of mice and re-populate parts of the organ (shown in brown). Image credit: Takeshi Katsuda (CC BY 4.0)
One of the most successful treatments for liver disease is transplanting a donor liver into a patient. But demands for donor livers far outstrips supply. A promising alternative could be, rather than replacing the whole organ, to transplant patients with individual liver cells called hepatocytes. These cells can then move into the liver, replace damaged cells, and help support the organ. However, hepatocytes are also in short supply, as despite the liver’s amazing regenerative abilities, these cells struggle to divide outside of the body. Improving how these cells multiply, could therefore help more people receive hepatocyte transplants.
In 2017, researchers found a way to convert mouse and rat hepatocytes into cells that could divide more rapidly using a cocktail of three small molecules. These 'chemically induced liver progenitors', or CLiPs for short, were able to mature into working hepatocytes and support injured mouse livers. But, discoveries made in rats and mice are not always applicable to humans. Now, Katsuda et al. – including some of the researchers involved in the 2017 work – have set out to investigate whether CLiPs can also be made from human cells, and if so, whether these cells can be used for hepatocyte transplantations.
Using a similar cocktail of molecules, Katsuda et al. managed to convert infant human hepatocytes into CLiPs. As with the rodent cells, these human CLiPs were able to turn back into mature, working liver cells. When transplanted into mice with genetic liver diseases, the human CLiPs moved into the liver and became part of the organ. These transplanted cells were able to reconstruct the liver tissue of diseased mice, and in some cases, replaced more than 90% of the liver’s damaged cells.
Developing human CLiP technology could provide a new way to support people on the waiting list for liver transplantation. But there are some obstacles still to overcome. At present the technique only works with hepatocytes from infant donors. The next step is to improve the method so that it works with liver cells donated by adults.




