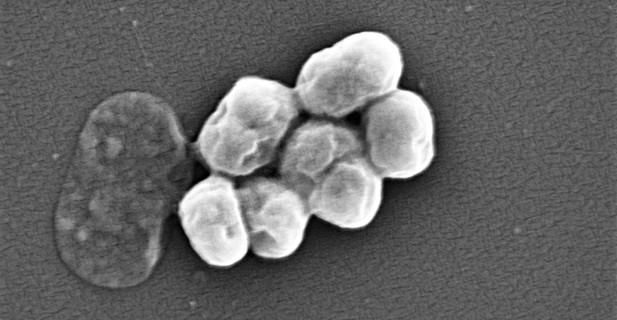
Acinetobacter baumannii. Image credit: Vader1941 (CC BY-SA 4.0)
A bacterium known as Acinetobacter baumannii causes serious lung infections in people with weakened immune systems. These illnesses are becoming more common largely because A. baumannii is increasingly developing resistance to antibiotics.
Inside the airways, individual A. baumannii cells can stick together and coat themselves in a slimy substance to form a structure called biofilm, which physically protects bacteria from antibiotics. This may be one of the reasons why it is often harder to treat bacterial infections associated with biofilms.
Another possibility is that bacteria may evolve differently in biofilms compared with cells living independently. For example, A. baumannii may colonize several regions of the lungs during an infection, leading to distinct groups of bacteria that experience different conditions and evolve separately. Each population may therefore respond differently to an antibiotic. In contrast, bacteria living independently in a well-mixed population – such as in the bloodstream of their host – would be more likely to all evolve in the same way.
Santos-Lopez, Marshall et al. tested this theory by exposing populations of A. baumannii that lived either independently or in biofilms to increasing levels of an antibiotic called ciprofloxacin. The genetic information of these cells was examined as the populations were evolving, and the bacteria were also put in contact with other types of antibiotics.
The analyses revealed that bacteria in well-mixed populations shared the same limited number of mutations: these gave the bacteria high levels of resistance to the antibiotic’s primary target, an enzyme involved in DNA processes. The bacteria had also become resistant to other classes of antibiotics.
In contrast, the bacteria in biofilm populations evolved to be more genetically diverse, exhibiting different types of mutations that helped the cells to pump out the drug. These bacteria were less resistant to ciprofloxacin and more sensitive to other types of antibiotics.
Further experiments looked into the fitness of the bacteria – their ability to survive, reproduce and compete with each other. High levels of antibiotic resistance came with lower fitness: biofilm bacteria had evolved to become being fitter than those from well-mixed population. Even in the absence of drugs, these populations were in fact fitter than the original cells.
Overall, understanding how the lifestyles of bacteria affect the way they respond to drugs may help researchers to develop new approaches that limit the spread of antibiotic resistance and improve treatment.




