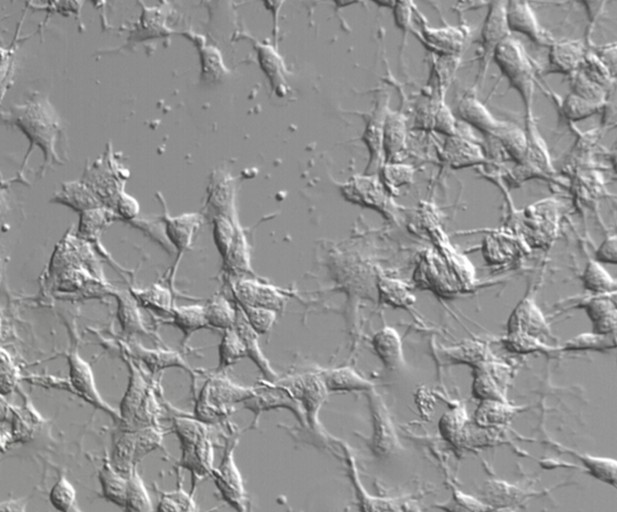
B16 cells, which are mouse tumor cells that are used as a model for human skin cancers, do not respond to PD-1 blockade therapy because they hide themselves from nearby T cells. Image credit: MSK-Cornell Center for Translation of Cancer Nanomedicine (Public domain)
Immunotherapy is a fast-emerging treatment area that turns the body’s own immune system against cancer. One powerful group of treatments are the PD-1 blockers. PD-1 is an inducible protein that is sometimes found on healthy immune cells called T cells and normally acts to stop T cells mistakenly attacking healthy cells. However, it can also prevent T cells attacking cancer. This happens when cancer cells make a protein called PD-1 ligand, which interacts with PD-1 to switch off nearby T cells. Antibodies that block PD-1 or PD-1 ligand can reactivate T cells, allowing them to destroy the cancer, but this PD-1 blocking therapy currently works in less than half of all patients who receive the treatment.
To mount a successful defense against cancer, a T cell needs to be able to perform two key tasks: recognize cancer cells and prepare to attack. T cells are alerted to the presence of the disease by MHC class I proteins on the surface of cancer cells holding up small fragments of molecules that are tell-tale sign that the cell is cancerous. To prepare to attack, a T cell depends on its mitochondria – the powerhouses of the cell – to send a cascade of signals inside the T cell that help it to activate and multiply. It is possible that cancer cells escape PD-1 blocking treatments by interfering with either one of these two tasks. They may either hide their MHC class I proteins to become invisible to passing T cells – a phenomenon known as “local immune ignorance”; or they may release long-range molecules to stop T cells preparing to attack – “systemic immune suppression”.
To explore these options further, Kumar, Chamoto et al. developed a new tumor model in mice. Each mouse had two tumors, one that responded to PD-1 blocking treatment and one that did not. The idea was that, if the unresponsive tumor was simply hiding from passing T cells, its presence should not affect the other tumor. But, if it was releasing molecules to block T-cell activation, the other tumor could become unresponsive to PD-1 blocking treatment too.
Kumar, Chamoto et al. examined different types of unresponsive tumor in this model system and found that they fell into two groups. The first group simply hid themselves from nearby T cells, while the second group released molecules to dampen all T cells. The identity of these molecules is unknown, but further experiments suggested that they likely work by blocking the mitochondria in T cells. In mice with these tumors, drugs that boosted mitochondria activity made anti-PD-1 treatment more effective.
If the findings in this mouse model parallel those in humans, it could open a new research area for immunotherapy. The next step is for researchers need to identify the molecule responsible for systemic immune suppression. This could help to make PD-1 blocking treatments more effective in people who do not currently respond.




