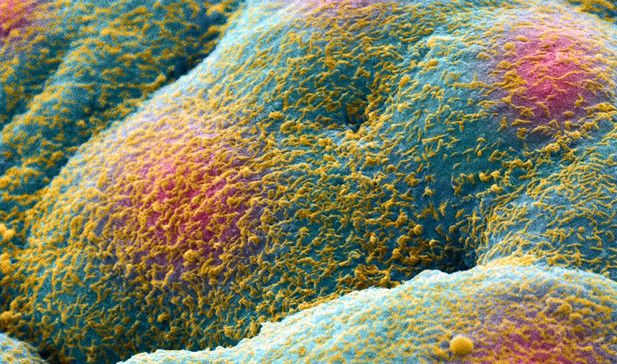
Prostate cancer cells forming a tumor or spheroid. Image credit: Khuloud T Al-Jamal (CC BY 4.0)
Decisions regarding the treatment of patients with early-stage prostate cancer are often based on the risk that the cancer could grow and spread quickly. However, it is not always straightforward to predict how the cancer will behave. Studies from 2017 and 2018 found that samples of less aggressive prostate cancer have higher levels of a group of proteins called MEIS proteins. MEIS proteins help control the production of numerous other proteins, which could affect the behavior of prostate cancer cells in many ways. VanOpstall et al. – including some of the researchers that performed the 2017 and 2018 studies – have investigated how MEIS proteins affect prostate cancer.
When prostate cancer cells are implanted into mice, they result in tumors. VanOpstall et al. found that tumors that produced MEIS proteins grew more slowly. Next, MEIS proteins were extracted from the prostate cancer cells and were found to interact with another protein called HOXB13, which regulates the activity of numerous genes. When the cells were genetically modified to prevent HOXB13 being produced, the protective effect of MEIS proteins was lost.
MEIS proteins work with HOXB13 to regulate the production of several other proteins, in particular a protein called Decorin that can suppress tumors. When MEIS proteins and HOXB13 are present, the cell produces more Decorin and the tumors grow more slowly and are less likely to spread. VanOpstall et al. found that blocking Decorin production rendered MEIS proteins less able to slow the spread of prostate cancer. These results suggest that MEIS proteins and HOXB13 are needed to stop tumors from growing and spreading, and some of this ability is by prompting production of Decorin.
This study explains how MEIS proteins can reduce prostate cancer growth, providing greater confidence in using them to determine whether aggressive treatment is needed. A greater understanding of this pathway for tumor suppression could also provide an opportunity for developing anti-cancer drugs.




