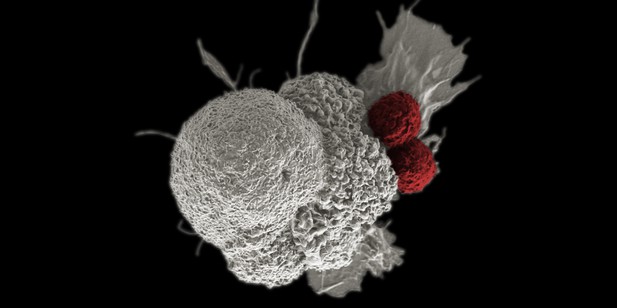
Microscopy image (pseudo-colorized) showing two T cells (red) attacking a cancer cell (white). Image credit: Rita Elena Serda, Duncan Comprehensive Cancer Center at Baylor College of Medicine, National Cancer Institute (CC BY-NC 2.0)
Over time cancer patients can become resistant to traditional treatments such as chemotherapy and radiotherapy. In some cases, this can be counteracted by administering a new type of treatment called immune checkpoint inhibition which harnesses a patient’s own immune system to eradicate the tumor. However, a significant proportion of cancers remain resistant, even when these immunotherapy drugs are used. This is potentially caused by tumors reactivating a gene called DUX4, which is briefly turned on in the early embryo shortly after fertilization, but suppressed in healthy adults.
Activation of DUX4 during the early stages of cancer has been shown to remove the cell surface proteins the immune system uses to recognize tumors. However, it remained unclear whether DUX4 changes the response to immunotherapy in more advanced cancers which have begun to spread and metastasize to other parts of the body.
To investigate, Pineda and Bradley analyzed publicly available sequencing data which revealed the genes turned on and off in patients with different types of cancer. The analysis showed that DUX4 is reactivated in approximately 10–50% of advanced bladder, breast, kidney, prostate and skin cancers.
Next, Pineda and Bradley studied a cohort of patients with advanced bladder cancer who had been treated with immune checkpoint inhibitors. They found that patients with tumors in which DUX4 had been turned back on had shorter survival times than patients who had not reactivated the gene.
These results suggest that the activity of DUX4 could be used to predict which patients with advanced bladder cancer may benefit from immune checkpoint inhibitors. In the future, this work could be extended to see if DUX4 could be used as a prognostic tool for other types of cancer. Future studies could also investigate if the DUX4 gene could be a therapeutic target for mitigating resistance to immunotherapy in metastatic cancers.




