Scientists have shed new light on the role of the placenta in managing the relationships between maternal vitamin D and foetal development, according to a study published today in eLife.
The findings demonstrate a complex interplay between vitamin D and the placenta, and could help inform future interventions using vitamin D to support foetal development and maternal adaptations to pregnancy.
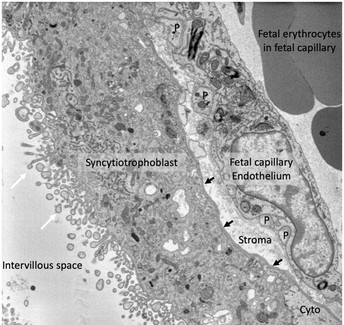
Vitamin D must be transferred from the maternal blood across the layers of the human placental barrier to the foetus, as shown in this electron microscopy image. The maternal blood fills the intervillous space and vitamin D crosses a continuous barrier called the syncytiotrophoblast (white arrows). Metabolism occurs within this layer and substances exit across the foetal-facing basal membrane and basal lamina (black arrows). The connective tissue of the stroma lies between the syncytiotrophoblast and the foetal capillaries. Image credit: Ashley et al. (CC BY 4.0)
As vitamin D is unable to be produced by a foetus, it must be transferred across the placenta. This is important for both foetal and lifelong health. Maternal vitamin D concentrations are positively associated with foetal bone growth and birth weight, and these associations continue into postnatal life.
Previous work has suggested that maternal vitamin D transfers passively across the placenta, but the current study challenges this idea.
“Research in kidneys has questioned the role of passive diffusion in the uptake of vitamin D. It has instead shown that this uptake is driven primarily by endocytosis of vitamin D, where the vitamin is bound to the binding protein albumin and introduced into the organ tissue cells,” explains Dr Claire Simner, Research Assistant at the University of Southampton, UK. Simner is a co-first author of the study alongside Dr Brogan Ashley, who was also at the University of Southampton at the time the work was carried out. “We proposed that a similar endocytic mechanism exists in the placenta, suggesting that this organ plays an active role in the delivery of vitamin D to the foetus.”
To explore this idea further, the team designed a study to find out how maternal vitamin D is taken up, metabolised and mediates gene expression within the human placenta. They used a perfusion model – involving the use of human placental samples collected from term pregnancies immediately after delivery – and placental fragment cultures to study the behaviour of the organ tissue. These methods contrast with cell-model approaches of previous research into how vitamin D transfers across the placenta.
To determine the mechanisms of placental vitamin D uptake, the team incubated fresh term human placental fragments with vitamin D alongside albumin for eight hours. They then analysed the gene expression of the fragments using a technique called quantitative rtPCR. Their analysis revealed a significant increase in the expression of the CYP24A1 gene – which is involved in controlling the amount of vitamin D in the body – in the fragments following incubation, compared to fragments that were incubated with vitamin D only. This suggests that albumin might enable vitamin D uptake.
“These findings show that endocytosis may play an important role in the uptake of vitamin D into the human placenta, as previously seen in the kidneys,” says Dr Jane Cleal, Lecturer in Epigenetics at the University of Southampton, and a co-senior author of the study alongside Professor Nicholas Harvey, Professor of Rheumatology and Clinical Epidemiology at the MRC Lifecourse Epidemiology Centre, University of Southampton.
Additionally, the team demonstrated that vitamin D exposure leads to rapid effects on the full set of messenger RNA molecules (the transcriptome) and of proteins (the proteome) expressed by the placenta. Their results revealed that the underlying epigenetic landscape of the placenta – the interaction between the genes and the environment – helps to dictate this transcriptional response to vitamin D treatment.
“This is the first quantitative study demonstrating the active transfer and metabolism of vitamin D by the human placenta, with widespread effects on the placenta itself,” Dr Cleal concludes. “As our data are generated from term placenta only, additional studies are needed to determine how our findings relate to earlier stages of gestation. Together, the insights from our work and future research will be helpful for identifying potential new options for targeted interventions to improve pregnancy outcomes.”
Media contacts
Emily Packer
eLife
e.packer@elifesciences.org
+441223855373
About
eLife is a non-profit organisation created by funders and led by researchers. Our mission is to accelerate discovery by operating a platform for research communication that encourages and recognises the most responsible behaviours. We review selected preprints in all areas of biology and medicine, including Developmental Biology, while exploring creative new ways to improve how research is assessed and published. eLife receives financial support and strategic guidance from the Howard Hughes Medical Institute, the Knut and Alice Wallenberg Foundation, the Max Planck Society and Wellcome. Learn more at https://elifesciences.org/about.
To read the latest Developmental Biology research published in eLife, visit https://elifesciences.org/subjects/developmental-biology.




