Seizures are a druggable mechanistic link between TBI and subsequent tauopathy
Figures
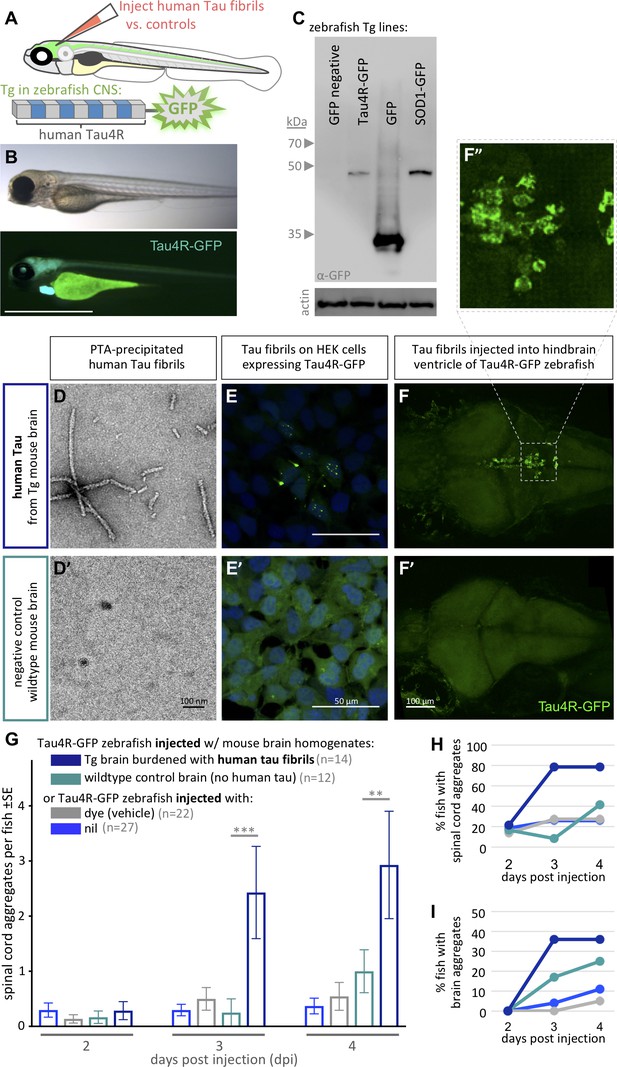
Validating tauopathy fluorescent biosensor in vitro and in zebrafish.
The biosensor Tau4R-GFP was validated for its ability to detect tauopathy seeds in vitro and in zebrafish. (A) Schematic of Tau4R-GFP ‘Tau biosensor’ that contains the four binding repeats (4R) region of wild-type human Tau linked to green fluorescent protein (GFP; see also Figure 1—figure supplement 1A). (B) Transgenic zebrafish engineered to express Tau4R-GFP biosensor throughout neurons of the CNS. Wild-type GFP is also abundant in the heart, which serves as a marker of the transgene being present but is otherwise irrelevant to our analyses. Scale bar ≅1 mm. (C) Western blot on zebrafish brain confirmed production of Tau4R-GFP at the expected size, similar to a SOD1-GFP biosensor and coordinately larger than GFP alone. (D) Human Tau fibril precipitated from transgenic (Tg TauP301L) mouse brain homogenates using PTA and assessed by EM. (E) Application of PTA-purified brain homogenate induced the formation of Tau inclusions similar to clarified brain homogenate (scale bar 50 μm; compare to Figure 1—figure supplement 1D), but application of equivalent preparations from non-Tg mice produced no GFP+ inclusions. (F–I) Tau biosensor zebrafish detects disease-associated human Tau fibrils following intraventricular injection of brain homogenate. Crude brain homogenates were microinjected into the hindbrain ventricle of Tau4R-GFP zebrafish larvae at 2 days post-fertilization, and Tau inclusions were analyzed at several time points. (F) Tau biosensor zebrafish larvae developed readily apparent GFP+ inclusions in the brain and spinal cord (Figure 1—figure supplement 2) when injected with brain homogenate burdened with Tau pathology (from Tg mice) but not from healthy brain homogenate (F’, from non-Tg mice). F’ inset shows many adjacent cells exhibiting GFP+ Tau aggregates. (G) Tau biosensor zebrafish injected with human Tau fibrils (within Tg mouse brain homogenate) developed significantly more aggregates on the spinal cord compared to uninjected control and other control groups, including compared to wildtype mouse brain homogenate (**p=0.0033 ***p=0.0006, ordinary two-way ANOVA and Tukey’s multiple comparison test). (H) Same data as in G, expressed as the percentage of larval fish showing Tau aggregates in the spinal cord, and (I) those same fish also showed Tau aggregates in the brain, over time. n = number of individual larvae. Images in E and F are 5 days post-application or post-injection, respectively.
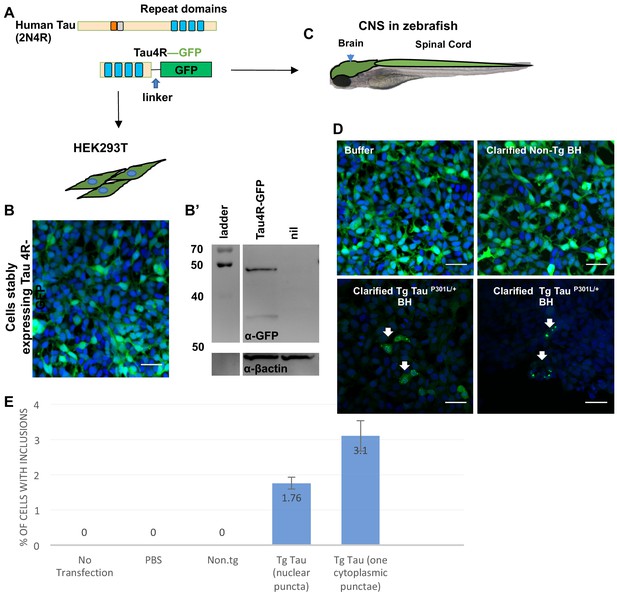
Quantification GFP+ inclusions in HEK cells expressing Tau4R-GFP biosensor.
(A) Schematic of genetically encoded fluorescent Tau4R-GFP ‘Tau Biosensor’ which was produced by fusing the C-terminal four binding repeats (4R) region of wild-type human Tau (Tau4R) to GFP via a linker. This construct was expressed as a transgene (C) in the zebrafish CNS under the promoter enolase 2, and (B) in human embryonic kidney HEK293T cells for validation. (B’) Immunoblot vs. GFP suggests the fusion protein Tau4R-GFP remains intact as a fusion protein when expressed in HEK cells and is an appropriate size (similar to when expressed in zebrafish CNS, Figure 1C). (D) Tau4R-GFP biosensor cells display GFP+ inclusions only upon transduction of crude brain homogenate burdened with tauopathy (from Tg mice expressing human TauP301L), but not when transduced with brain homogenate from normal mice (non-Tg BH). (E) HEK cells from D had a detection rate of approximately 2–3% of cells having GFP+ puncta, whereas various negative controls (no transfection, transfection with PBS only, or transfection of brain homogenate from non-Tg control mice) consistently showed no puncta. For the quantification, the number of cells with inclusions and the number of total cells from nine field images were counted. Bars represents mean of three independent experiments.
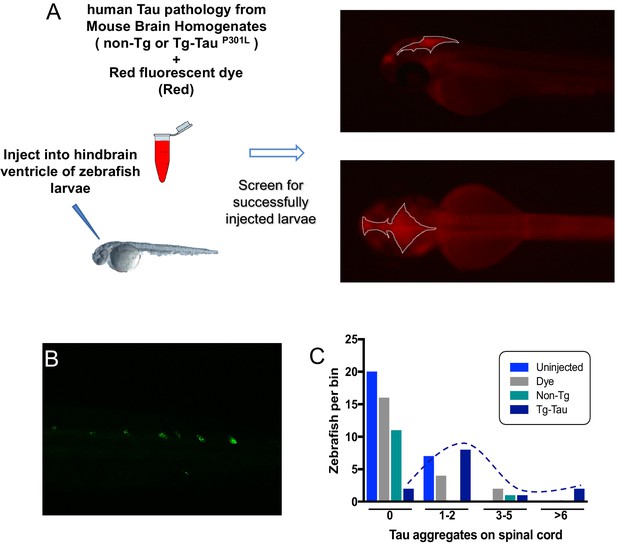
Quantification GFP+ inclusions in CNS of zebrafish expressing Tau4R-GFP biosensor, following injection of human Tau into the zebrafish hindbrain ventricle.
(A) Schematic showing the microinjections of mouse brain homogenate into the brain ventricles of zebrafish larvae (age is 2 days post-fertilization). Injected material was brain homogenate from transgenic mice expressing human Tau, that is with Tau pathology (e.g. see pathology characterized in Eskandari-Sedighi et al., 2017, DOI 10.1186/s13024-017-0215-7) or brain homogenate from normal control mice. Red fluorescent dye included in the diluted brain homogenate allowed imaging and selection of properly injected embryos. Right: Successfully injected embryos had the injected brain homogenate localized within the zebrafish brain ventricles, with sharp edges and non-diffuse dye. The area encompassing the injected dye is outlined by white dotted lines. (B) Similar to Tau4R-GFP aggregating in the brain, GFP+ aggregates were also detected in the spinal cord following delivery of human Tau, akin to the brain aggregates in Figure 1F. (C) Quantification of spinal cord aggregates. Same data as Figure 1G re-plotted to show the distribution of larvae displaying various quantities of aggregates in the spinal cord. Color coding of treatments equivalent to Figure 1G. Dotted line is hand drawn to emphasize the distribution of larvae injected with tau-burdened brains, compared to various the controls with peak distributions of GFP+ puncta near to zero.
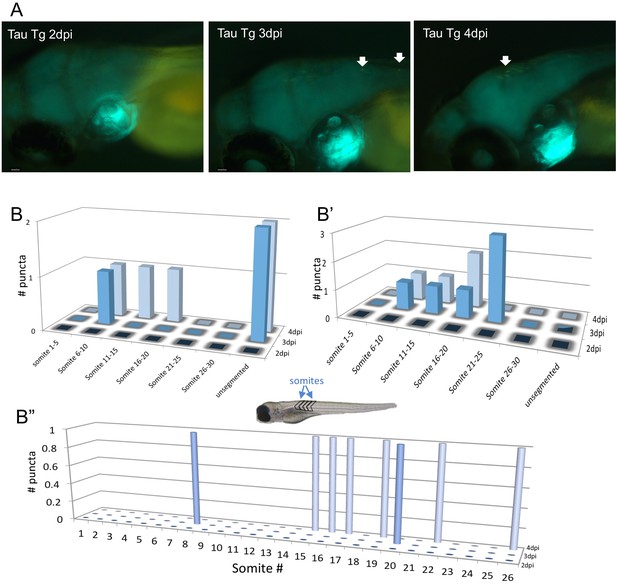
Movement of some Tau puncta over time following injection of zebrafish larvae with brain homogenate burdened with human tauopathy.
(A) Images of the zebrafish brain area, after injection with Tg hTau+/p301L mouse brain homogenate, for the same zebrafish larvae over 3 consecutive days post-injection (dpi), showing the movement of one puncta over time. (B, B’ and B”) The location of Tau aggregates on the spinal cord of three exemplar individual larvae over multiple days, denote movement of some of these puncta over time. Somite numbers were used as landmarks to report the location along the spinal cord over multiple days - somites are blocks of tissue (e.g. muscle) that are readily visible in the trunk of the larva; larger somite number are more posterior (i.e. more distal to the injected brain region) with the most distal region being ‘unsegmented’.
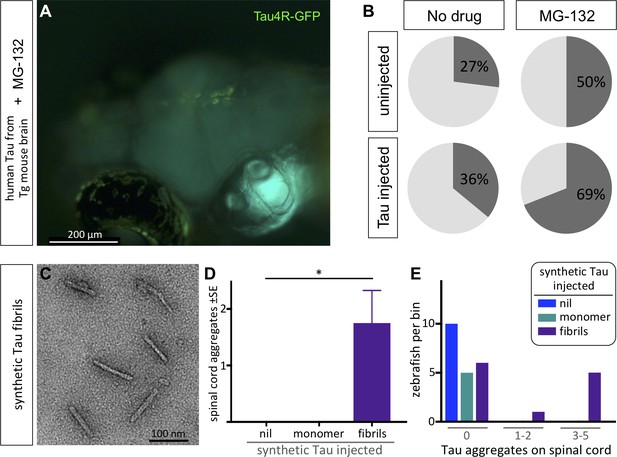
Protein-only induction of Tau puncta in vivo detected in biosensor zebrafish.
Injections of synthetic Tau fibrils into Tau4R-GFP zebrafish induced GFP+ puncta in brains and spinal cord. (A,B) Inhibiting the proteosome with MG-132 enhanced the percentage of larvae bearing GFP+ inclusions in the brain following injection of tau-laden brain homogenate. (C) Synthetic human Tau proteins were fibrillized as confirmed via EM analysis. Human Tau fibrils were microinjected into the larval hindbrain at 2 days post-fertilization, and Tau inclusions were analyzed at 3 days post injections. (D) Tau aggregates were only observed after injection of Tau fibrils, not monomers (*p=0.0104, Kruskal Wallis test). (E) Tau aggregates (same data as D, presented as distribution of larvae that displayed various amounts of GFP+ puncta) appear only after injection of Tau fibrils, not monomers.
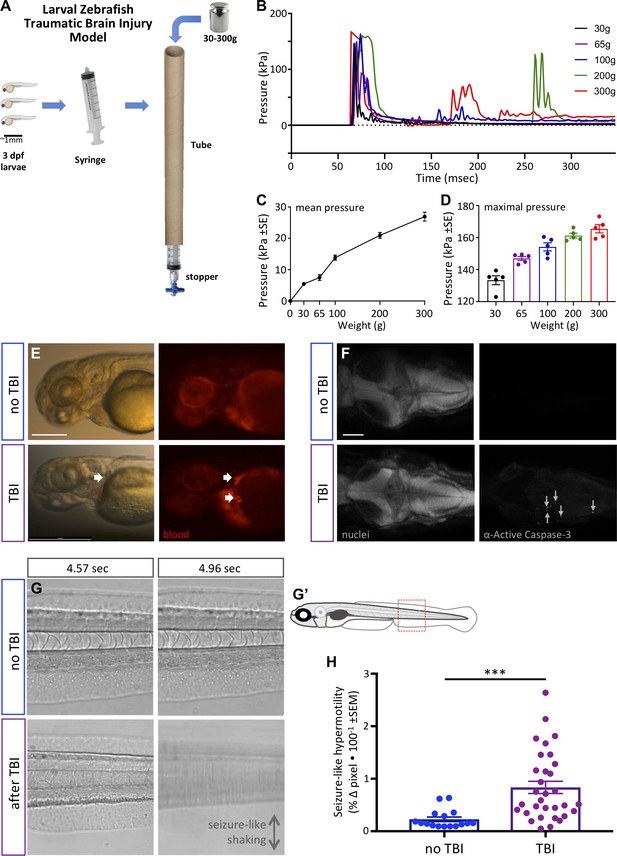
Zebrafish larvae subjected to traumatic brain injury (TBI) exhibited various biomarkers of TBI.
(A) A novel TBI model for larval zebrafish: to induce blast injury, zebrafish larvae were loaded into a syringe with a stopper. A defined weight was dropped on the syringe plunger from a defined height, producing a pressure wave through the fish body akin to pressure waves experienced during human blast injury. (B) Dynamics of the pressure increase after dropping weights of varying masses in our TBI model. (C,D) The mean and maximum pressures generated, respectively, by various weights applied in the TBI model. Dots represent individual trials. (E) Hemorrhage after TBI was observed in some of the larvae fish using Tg[gata1a:DsRed] transgenic zebrafish that express DsRed in erythrocytes, as indicated by white arrows. Lateral view of larval heads with anterior at the left. Scale bar ≅250 μm. (F) Increased cell death in the brain of 4 dpf larvae subjected to TBI as indicated by immunostaining of activated Caspase-3 (magenta). Positive and negative controls for immunostaining are in supplement. Nuclei were stained with DAPI in gray for reference. These are dorsal views of larval zebrafish brains with anterior at the left. Scale bar is 100 μm. (G) Seizure-like clonic shaking is observed in a subset of larvae after TBI. Movie frames are displayed from Video 2. These frames (left and right panels) are separated by ~400 ms in time, and are lateral views of the larval zebrafish trunk (akin to red box in G’). Control fish without TBI show little movement except obvious blood flow. Following TBI, larvae show bouts of calm (bottom left) interspersed (~400 ms later) with bouts of intense seizure-like convulsions (Stage III seizures; bottom right). (H) Larvae subjected to TBI also displayed Stage II seizures, that is weaker seizures that manifest as hypermotility and are detected using a previously optimized behavioral tracking software system – seizures are significantly more intense following TBI compared to the control group (***p=0.0013, paired t-test; dots are raw data for each larva, mean is plotted ± SE).
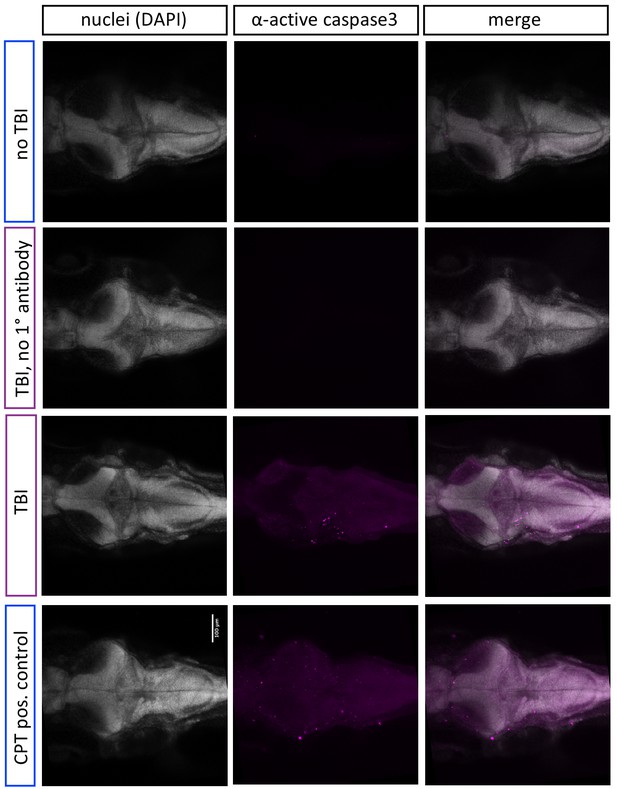
Traumatic brain injury (TBI)-induced cell death.
Some data copied from Figure 3F here for ease of reference. Increased cell death in the brain of 4 dpf larvae subjected to TBI as indicated by immunostaining of activated Caspase-3 (magenta). Larvae exposed to topoisomerase inhibitor camptothecin (CPT, 3 μM) which induce apoptosis, serves as a positive control. Nuclei were stained with DAPI in gray for reference these are dorsal views of zebrafish brains with anterior at the left.
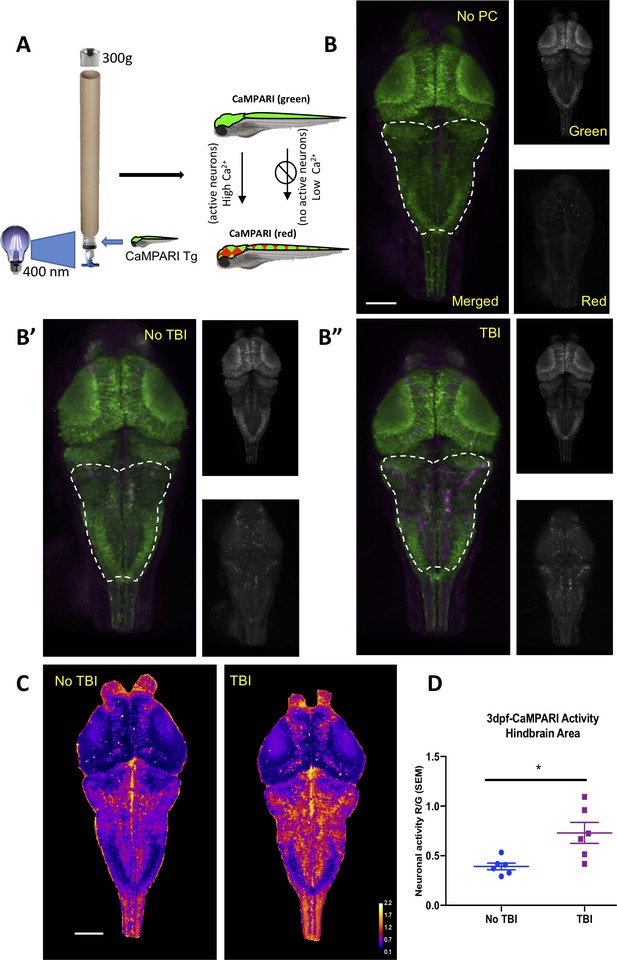
Neural activity increases during traumatic brain injury (TBI) as measured in CaMPARI zebrafish larva.
(A) Schematic of TBI using CaMPARI (Calcium Modulated Photoactivatable Ratiometric Integrator) to optogenetically quantify neuronal excitability. Three dpf CaMPARI larvae were freely swimming while subjected to TBI, coincident with exposure to 405 nm photoconversion light. CaMPARI fluorescence permanently photoconverts from green to red emission only if the photoconversion light is applied while neurons are active (high intracellular [Ca2+]). The ratio of red:green emission is stable such that it is quantifiable via subsequent microscopy. (B) Increased neural activity during TBI is represented by increased red:green emission (red pseudocolored to magenta) in the hindbrain of larvae (B”), compared to larvae not receiving TBI (B’) or fish not exposed to photoconverting light (‘no PC’ in panel B). These representative maximum intensity projection images show dorsal view of zebrafish brain (anterior at top), including merged, or red or green channels alone. (C) Heatmaps encode the CaMPARI signal (higher neural activity = higher red:green = hotter colors), highlighting location of increased neural activity during TBI relative to control larvae not receiving TBI. (D) Quantification of CaMPARI output in the hindbrain area reveals a significant increase in the neuronal excitability during TBI compared to control group not receiving TBI (**p=0.0087, Mann-Whitney test. Each data point is an individual larva). Scale bars = 100 μm.
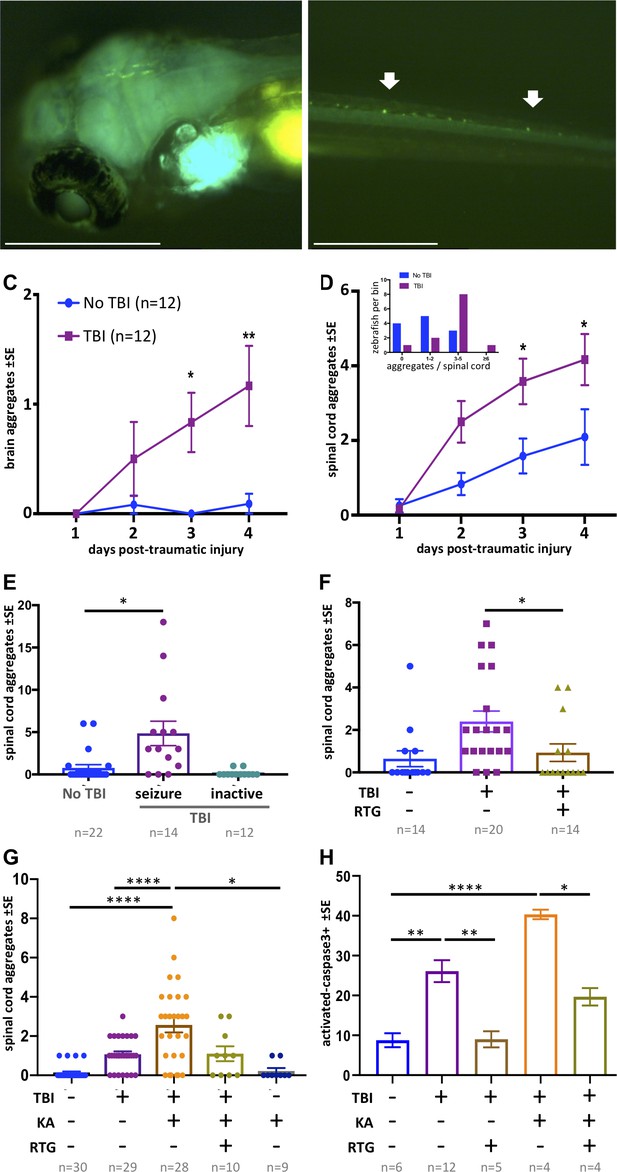
Traumatic brain injury (TBI) induces tauopathy in larval zebrafish.
(A) GFP+ Tau puncta are detected in the brain of Tau4R-GFP biosensor zebrafish at 5 days post-traumatic brain injury (dpti). A 300 g weight was used to induce TBI throughout this figure. (B) Tau aggregates formed on the spinal cord as a result of the TBI as shown by arrows. (C) Tauopathy significantly increases over time following TBI compared to control group (No TBI) *p=0.0264, **p=0.007, two-way ANOVA with Tukey’s multiple comparison test. (D) The number of Tau aggregates in spinal cord significantly increases over time following TBI compared to control group (*p=0.0224 at 3dpti and *p=0.0312 at 4dpti). Inset: Tau4R-GFP zebrafish larvae subjected to TBI develop more GFP+ puncta compared to the control group by 3dpti (inset plot is similar to Figure 2E). Figure 5—figure supplements 2 and 3 plot this in individual fish. (E–H) Post-traumatic seizures link TBI to tauopathy. (E) Following TBI, larvae displaying post-traumatic seizures developed many more Tau aggregates relative to those not displaying post-traumatic seizures (**p=0.0011, Kruskal-Wallis ANOVA with Dunn’s multiple comparison test). (F) Inhibiting post-traumatic seizures with the anti-convulsant retigabine (RTG, 10 μM) significantly decreased the abundance of GFP+ puncta in the spinal cord (p=0.0107, Mann-Whitney test). (G) Increasing post-traumatic seizure using the convulsant kainate (KA, 100 μM; see dose-response in Figure 5—figure supplement 5) significantly increased the formation of Tau aggregation following TBI; this effect was prevented by co-treatment with anti-convulsant RTG. ****p<0.0001, ordinary one-way ANOVA with Tukey’s multiple comparison test. (H) Blunting post-traumatic seizures with RTG reduced TBI-related cell death. The main impact of RTG was specific to its anticonvulsant modulation of seizures because its effects were reversed by convulsant KA. Color scheme in panel C applies to other panels. n = number of zebrafish larvae. ****p<0.0001, ordinary one-way ANOVA with Tukey’s multiple comparison test. Scale bars = 500 μm.
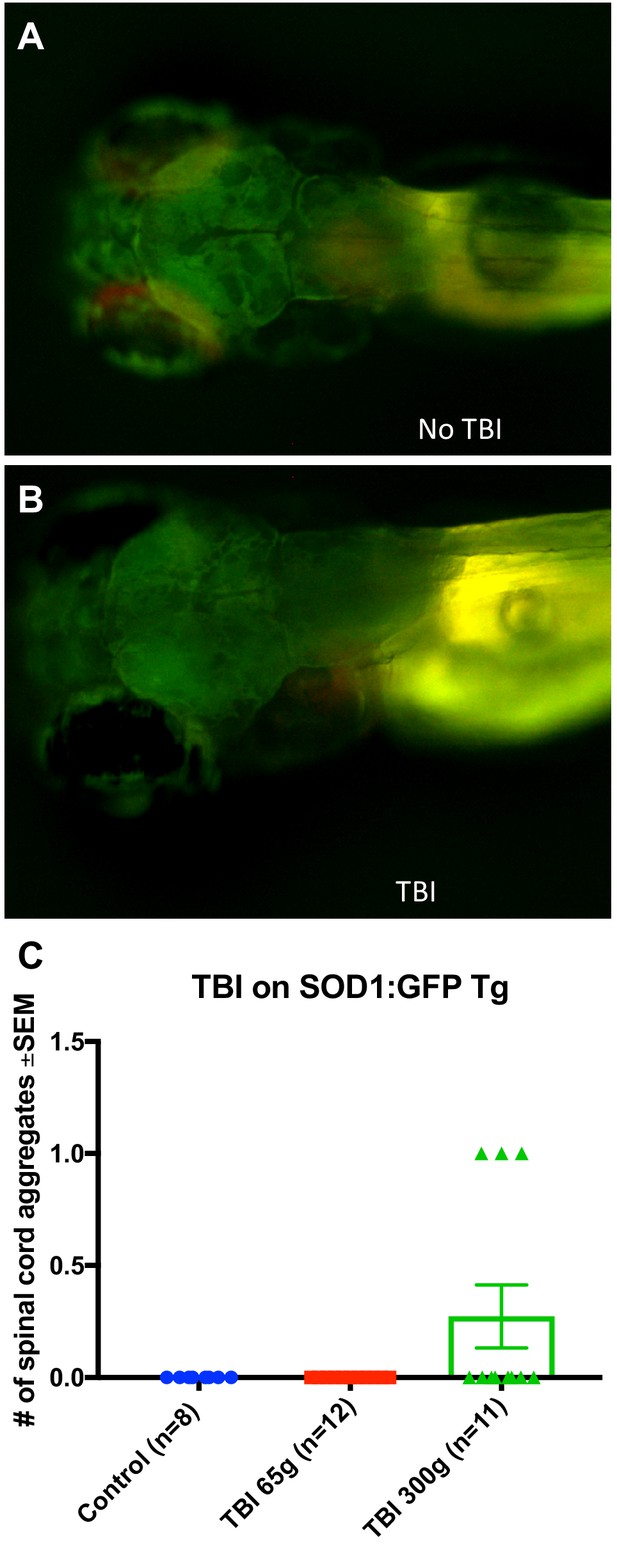
Traumatic brain injury (TBI) did not induce GFP+ puncta in transgenic zebrafish larvae expressing SOD1-GFP.
(A, B) TBI did not induce GFP+ puncta in larvae expressing SOD1-GFP, and appeared similar to control larvae that did not experience TBI. (C) Quantification of GFP+ puncta in the spinal cord of SOD1-GFP showing the majority of samples did not develop aggregates post-TBI.
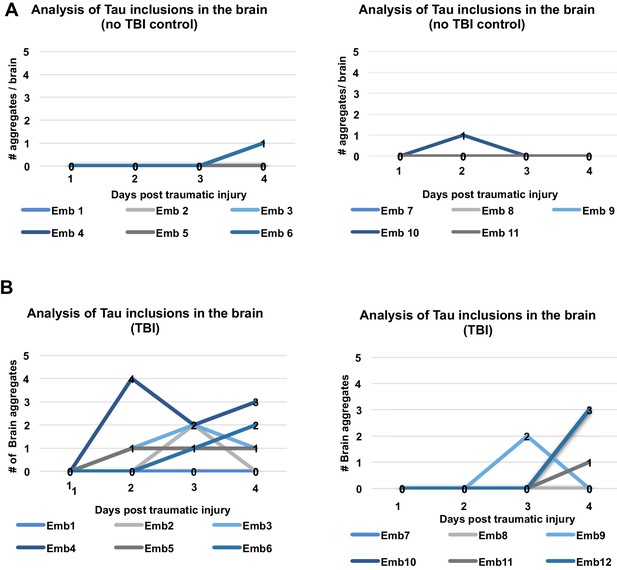
Longitudinal analysis of individual fish after traumatic brain injury (TBI) shows various patterns of TAu inclusion formation and clearance in their brains.
(A) In the control group (no TBI) the majority of Tau4R-GFP biosensor larvae did not develop GFP+ aggregates in the brain, although a few either developed aggregates at later time point (3dpi), or developed aggregates that disappeared at later timepoints. (B) Tau4R-GFP biosensor larvae subjected to TBI developed more GFP+ brain aggregates and at earlier timepoints compared to controls, and the number of aggregates typically (although not always) increased with time. Within panels A and B, the left and right graphs are equivalent and display several larvae each.
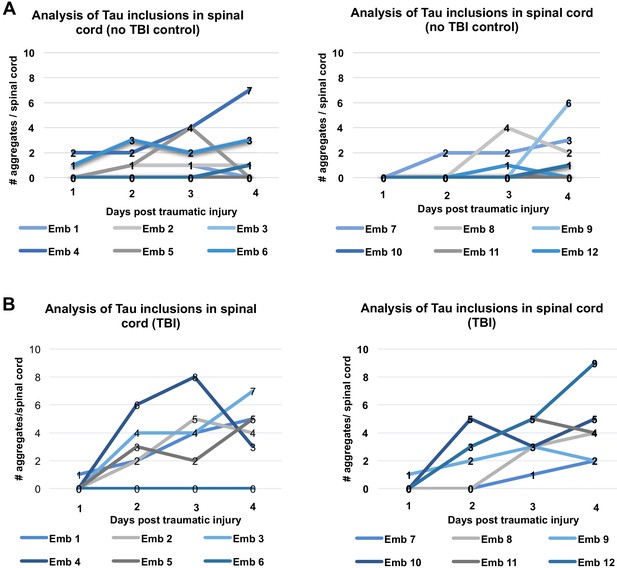
Longitudinal analysis of individual fish after traumatic brain injury (TBI) shows various patterns of Tau inclusion formation and clearance in their spinal cords.
(A) Exemplar data from the control group (no TBI) wherein many of the Tau4R-GFP biosensor larvae did not develop aggregates in the spinal cord, while a few either developed aggregates at later timepoints, or developed aggregates that disappeared later on. (B) Tau4R-GFP biosensor larvae subjected to TBI developed more GFP+ spinal cord aggregates and at earlier timepoints compared to controls, and the number of aggregates typically (although not always) increased with time. Within panels A and B, the left and right graphs are equivalent and display several larvae each.
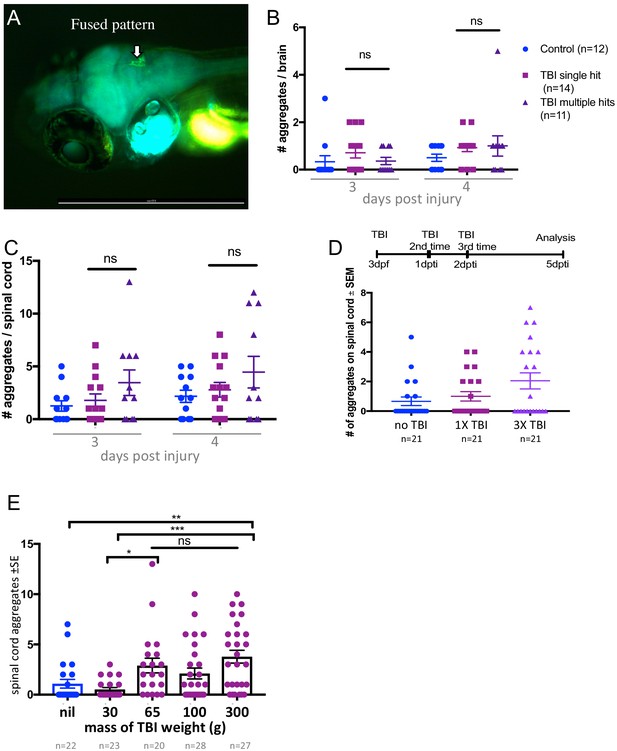
Increasing intensity of traumatic brain injury (TBI) significantly increased Tau4R-GFP puncta abundance, but only modest insignificant increases in Tau puncta were observed with an increasing number of successive brain injuries.
(A) Following TBI of Tau4R-GFP larvae, the GFP+ aggregates in the brain tended to be fused. (B,C) Tau4R-GFP larvae were subjected to TBI via either one single hit or five consecutive hits. The number of GFP+ aggregates in the brain (B) and the spinal cord (C) were quantified at 3 and 4 days post-traumatic brain injury (dpi). The number of aggregates modestly increases with more hits but not consistently (not statistically significant). The symbols for treatment types are equivalent in panels B and C. (D) Performing TBI on Tau4R-GFP larvae on each of 3 consecutive days slightly increased the number of GFP+ Tau puncta in the spinal cord (relative to a single TBI treatment) but the increase was not statistically significant. (E) A nearly linear dose-response of TBI injury intensity varying with the abundance of GFP+ puncta in the spinal cord. TBI intensity was modulated by dropping weights of varying masses in the TBI method. Heavier weights induced more GFP+ puncta (*p<0.01 and **p<0.001). In each panel, raw data is plotted, along with mean ± standard error.
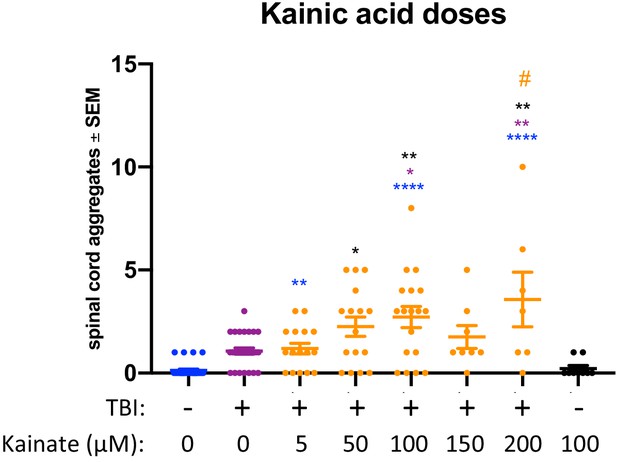
Intensifying seizures following traumatic brain injury (TBI) increased abundance of GFP+ Tau puncta in a dose-dependent manner.
Tau4R-GFP larvae were subjected to TBI and post-traumatic seizures were intensified by addition of the convulsant kainate. Although kainate treatment alone (without TBI) did not appreciably increase GFP+ Tau puncta in the spinal cord (black), kainate significantly increased the abundance of puncta in larvae receiving TBI (*p<0.5, **p<0.01, ****p<0.0001 compared to TBI alone [blue text]; #p<0.01 compared to TBI+5 μM dose). Raw data is plotted for each larva, along with mean ± standard error.
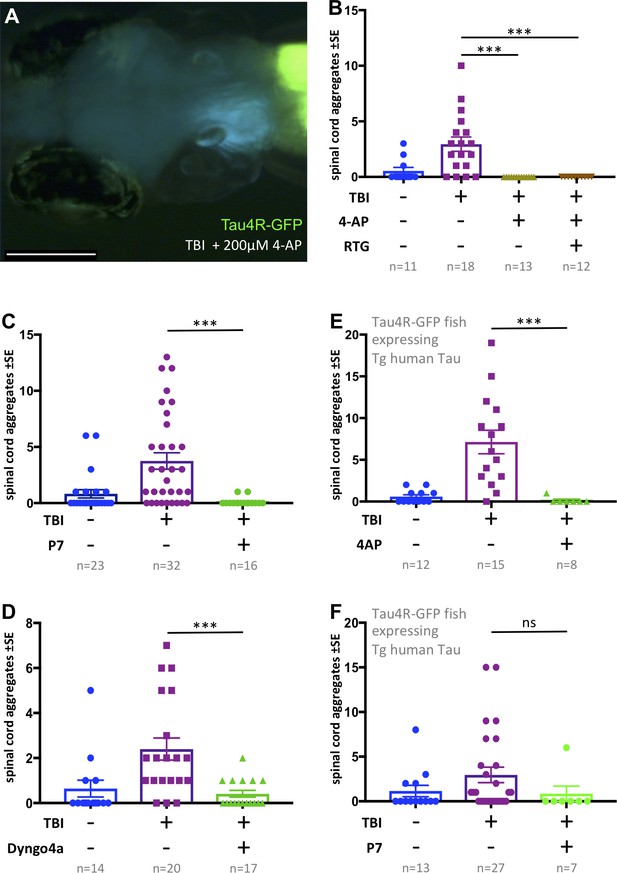
Tauopathy induced by traumatic brain injury (TBI) was attenuated by 4-aminopyridine (4-AP) via mechanisms independent of seizures.
(A) Tau4R-GFP biosensor zebrafish larvae subjected to TBI and treated with the convulsant 4-AP show no brain puncta. Scale bar = 200 μm. (B) 4-AP significantly reduced (apparently eliminated) the abundance of GFP+ puncta in the brain and spinal cord compared to untreated TBI control. Results from alternative doses and timings of 4-AP are reported in Figure 6—figure supplement 1. The impact of 4-AP on tauopathy appears to be independent of its actions on post-traumatic seizures because reducing the latter with anti-convulsant retigabine (RTG) had no measurable effect. (C-F) Pharmacological inhibition of endocytosis reduced tauopathy following TBI. (C) Blocking endocytosis with Pyrimidyn-7 (P7) treatments significantly inhibited the formation of Tau4R-GFP+ puncta following TBI in zebrafish larvae (***p=0.001). (D) Dyngo 4a treatment significantly reduced Tau aggregates in the spinal cord (**p=0.0025) in a manner similar to P7. (E) 4-AP treatment significantly inhibited the formation of Tau4R-GFP+ puncta in the spinal cord (***p=0.0003) of Tau biosensor line that also express human Tau (0N4R) after traumatic brain injury compared to untreated TBI control group. (F) A notable reduction in Tau aggregates was observed in the same line after treatment with P7 drug. Statistical analysis shows no significance difference (ns, p=0.2223) between groups. n = number of larvae. ****p<0.0001, Kruskal-Wallis ANOVA with Dunn’s multiple comparison test used throughout this Figure.
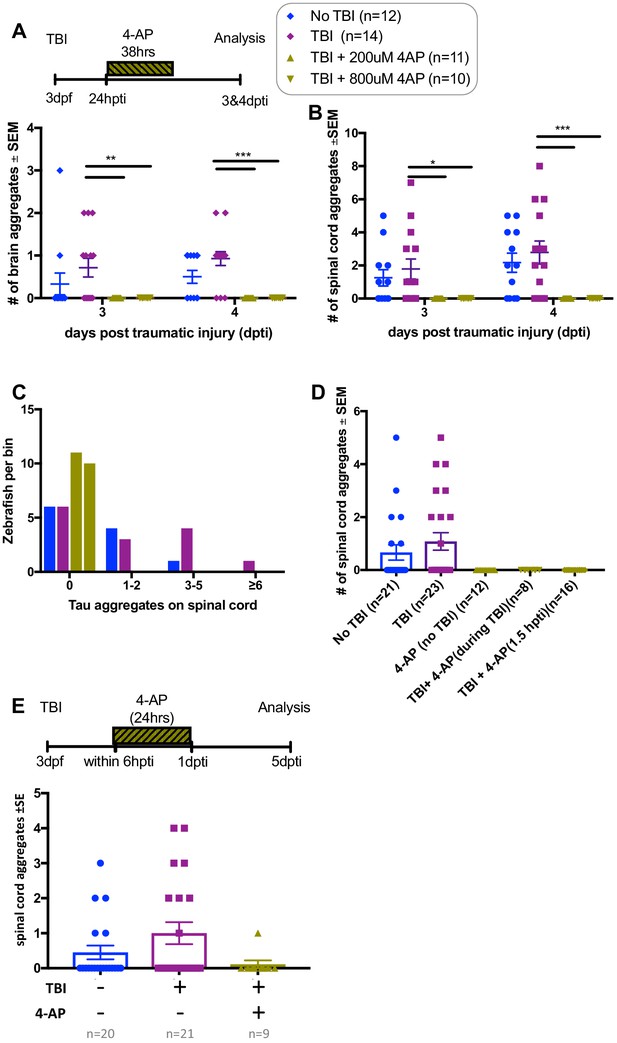
4-Aminopuridine (4-AP) abrogates TBI-induced Tau aggregates when applied at various doses or for various times.
(A) Tau4R-GFP biosensor zebrafish larvae subjected to TBI and treated with the convulsant 4-AP show no brain puncta. 4-AP was added to the TBI larvae 1 day post-traumatic brain injury (dpti) and left for 38 hr as displayed in timeline at top. (A,B) 4-AP significantly reduced (apparently eliminated) the abundance of GFP+ puncta in the brain and spinal cord compared to untreated TBI control (**p<0.009 at 3dpti and ***p<0.0003 at 4dpti) at two different doses. (C) All larvae treated with 4-AP failed to display any GFP+ puncta (# of aggregates is 0), displayed as distribution of larvae binned into the number of GFP+ puncta they exhibited. (D,E) Timing and duration of 4-AP treatments following TBI had no appreciable effect on 4-AP abrogating the TBI-induced Tau aggregates. Symbols and colors for all panels are consistent with the legend at the top right of the Figure.
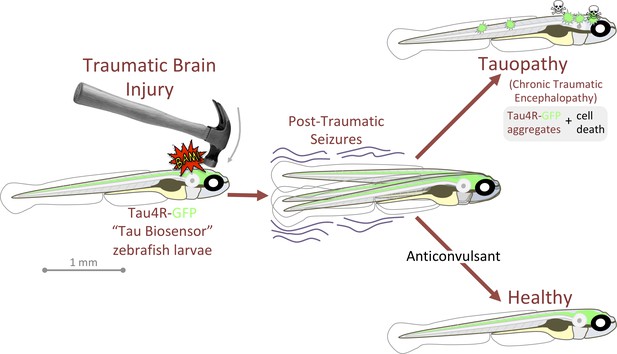
Graphical summary: anticonvulsants reverse the tauopathy and cell death exhibited by zebrafish larvae following traumatic brain injury (TBI).
Tauopathy was reported via aggregation of a genetically encoded chimeric protein, Tau4R-GFP, that was expressed throughout the central nervous system. TBI led to seizures, and subsequently to Tau aggregation and cell death (akin to chronic traumatic encephalopathy, CTE). The tauopathy and cell death were ameliorated, producing healthy larvae, by blocking seizures with anti-convulsants; these effects were specific insomuch that they could be reversed by co-application of convulsants.
Videos
TBI-induced blood flow abnormalties.
TBI-induced seizures and blood flow abnormalities.
Tables
| Reagent type (species) or resource | Designation | Source or reference | Identifiers | Additional information |
|---|---|---|---|---|
| Strain (zebrafish) | Tg(eno2:hsa.MAPT-ires-egfp)Pt406 | Burton’s Lab (Bai et al., 2007) | ZFIN ID: ZDB-ALT-080122–6 | Zebrafish that express human four repeat TAU |
| Strain (zebrafish) | Tg(eno2:SOD1-GFP) ua3181 | This paper | N/A | zebrafish biosensor engineered to detect human SOD1 aggregation |
| Strain (zebrafish) | Tg[elavl3:CaMPARI (W391F+V398L)]ua1344 | In house allele (Kanyo et al., 2020b) established using vector provided by Eric Schreiter’s lab | zebrafish expressing the calcium sensor CaMPARI | |
| Strain (Zebrafish) | Tg(eno2:Hsa.MAPT_Q244-E372−EGFP)ua3171 | This paper | N/A | Zebrafish biosensor engineered to detect human Tau aggregation |
| Genetic reagents (zebrafish) | Multisite Gateway technology (BP Clonase II Enzyme mix and LR Clonase II Plus enzyme) | Thermo Fisher | Cat# 11789020 Cat# 12538120 ZFIN ID: ZDB-PUB-170809–10 | Guo and Lee, 2011; Kwan et al., 2007 |
| Cell line (Homo-sapiens) | HEK293T | ATCC Provided by Dr. David Westaway’s laboratory | Cat# CRL-3216, RRID:CVCL_0063 | |
| Sequence-based reagent | GFP_R | This paper | PCR primer | TCTCGTTGGGGTCTTTGCTC |
| Biological sample (mouse) | Whole brains | Tissues were provided by Dr. David Westaway (Eskandari-Sedighi et al., 2017; Murakami et al., 2006) | Isolated from wild -type mice with 129/SvEvTac genetic background, and TgTauP301L mice | |
| Antibody | Anti GFP (rabbit monoclonal) | Abcam | Cat# ab183734, RRID:AB_2732027 | WB(1:3000) |
| Antibody | Anti-β-actin (rabbit polyclonal) | Sigma-Aldrich | Cat# A2066, RRID:AB_476693 | WB (1:10000) |
| Antibody | Anti-Active-Caspase-3 (rabbit polycolonal) | BD Pharmingen | Cat# 559565, RRID:AB_397274 | IHC (1:500) |
| Antibody | Alexa Fluor 647 (chicken anti-rat IgG) | Invitrogen | Cat# A-21472, RRID:AB_2535875 | WB (1:500) |
| Peptide, recombinant protein | Human MAPT (2N4R) | rPeptide | Cat# T-1001–2 | Resuspended to 2 mg/ml before use |
| Chemical compound, drug | Kanic acid monohydrate | Sigma Aldrich | K0250 | |
| Chemical compound, drug | Retigabine | Toronto research chemicals | R189050 | |
| Chemical compound, drug | 4-Aminopyridine (4AP) K+ channel blocker | Sigma | Cat# 275875–1G | |
| Chemical compound, drug | Pyrimidyn-7 (P7) Dynamin inhibitor | Abcam | Cat# ab144501 | 50 mM concentration supplied in DMSO |
| Chemical compound, drug | Dyngo 4a | Abcam | Cat# ab120689 | |
| Software, algorithm | Lab Chart 7 (software) | AD Instruments | ||
| Software, algorithm | Geneious Prime (bioinformatics software) | geneious.com | Version 8 | |
| Other | Human MAPT (Gene block) | Ordered from IDT | This is aa 244–372 of the full-length TAU 2N4R with seven-amino acid C-terminal linker (RSIAGPA) | |
| Other | Power lab Data acquisition device (equipment) | AD Instruments | 2/26 | |
| Other | Piezoresistive pressure transducer (equipment) | AD Instruments | Cat# MLT844 | |
| Other | Lipofectamine. 2000 (transfection reagents) | Invitrogen | Cat# 11668–019 | |
| Other | DAPI stain | Thermo Fisher | D1306 | (1 µg/mL) |
Additional files
-
Source data 1
Source data and statistics.
- https://cdn.elifesciences.org/articles/58744/elife-58744-data1-v1.zip
-
Transparent reporting form
- https://cdn.elifesciences.org/articles/58744/elife-58744-transrepform-v1.pdf





