Sex differences in biological aging with a focus on human studies
Figures
Figure 1
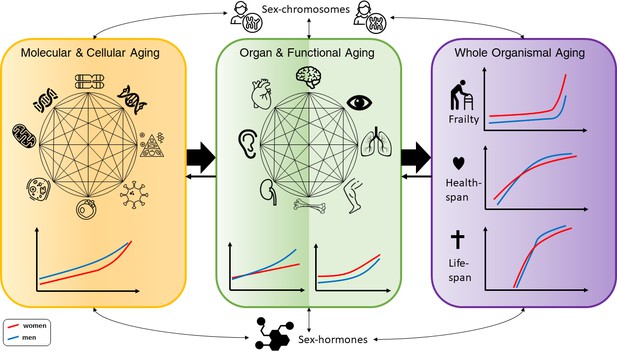
Conceptual framework of the complex interactions between molecular, cellular, functional, organ, and whole body aging processes across the life course in men and women, with influences from chromosomes and hormones on the sex differences.
The different illustrations made for men and women are based on descriptions in the text. For healthspan and lifespan, trajectories are taken from a recent publication by Li et al., 2021.
Tables
Table 1
Sex specificity in human biological aging and associated theories.
| Human biomarker of aging | Sex-specific effects | References | Aging theories | Sexual dimorphism theories |
|---|---|---|---|---|
| Genetic factors in aging | Sex chromosomes, X-chromosome inactivation in women, Loss of Y in men, Common genetic variants for anthropometric traits, Transcriptional regulation | Bernabeu, 2020; Forsberg, 2017; Gentilini et al., 2012; Randall et al., 2013 | Senescence theory of aging: 1. Disposable soma 2. Mutation accumulation Programmed theory of aging: 1. Developmental processes and growth | Sex chromosomes Hormones |
| Mitochondria-linked mechanisms | Better respiratory function in women, Mutation accumulation, Higher mtDNA abundance in women | Hägg et al., 2020; Demarest and McCarthy, 2015; Ventura-Clapier et al., 2017 | Senescence theory of aging: 1. ROS theory of aging 2. Mutation accumulation | Hormones |
| Cellular senescence | More senescent cells in male mice compared to females. | Yousefzadeh et al., 2020 | Senescence theory of aging | Unknown |
| Proteostasis and autophagy | Higher proteasomal activity in female mice and flies | Jenkins et al., 2020; Pomatto et al., 2017 | Senescence theory of aging: 1. ROS theory of aging | Unknown |
| Telomeres | Longer telomeres in girls/women | Factor-Litvak et al., 2016; Gardner et al., 2014 | Programmed theory of aging: 1. Hayflick limit 2. Developmental processes and growth Senescence theory of aging: 1. ROS theory of aging | Sex chromosomes, Hormones |
| Epigenetics | Higher epigenetic age in boys/men, Genome-wide DNA methylation and histone differences | Horvath et al., 2016; Horvath and Raj, 2018; Klein et al., 2019 | Programmed theory of aging: 1. Hayflick limit 2. Developmental processes and growth Senescence theory of aging: 1. Disposable soma 2. Mutation accumulation | Sex chromosomes, Hormones |
| Inflammatory and immunological markers | Men more affected by immunosenescence and inflammaging | Gubbels Bupp, 2015; Gomez et al., 2018; Franceschi, 2019 | Senescence theory of aging: 1. ROS theory of aging | Hormones |
| Nutrient sensing and metabolism | Women have more beneficial (lower) fasting insulin levels | Templeman and Murphy, 2018; Pignatti et al., 2020; Comitato et al., 2015 | Senescence theory of aging: 1. The rate of living theory Programmed theory of aging | Hormones |
| Functional measures | Men perform better in physical functioning, regardless of the measures | Peiffer et al., 2010; Ganna and Ingelsson, 2015; Frederiksen et al., 2006; Finkel et al., 2019 | Senescence theory of aging: 1. ROS theory of aging 2. The rate of living theory | Hormones |
| Frailty | Women have higher levels, but men are more vulnerable to death at any given level | Gordon et al., 2017; Gordon and Hubbard, 2019 | Senescence theory of aging: 1. Disposable soma | Hormones |
| Leading causes of death (noncommunicable diseases) worldwide in 70 + year olds: 1. Ischemic heart disease 2. Stroke 3. Chronic obstructive pulmonary disease 4. Alzheimer's disease and other dementias 5. Diabetes mellitus 6. Trachea, bronchus, lung cancers 7. Kidney diseases 8. Hypertensive heart disease 9. Colon and rectum cancers | Men have higher incidence and death rates in: 1. Ischemic heart disease 5. Diabetes mellitus in midlife 6. Trachea, bronchus, and lung cancers 9. Colon and rectum cancers Men have higher incidence of: 2. Stroke in early adulthood 5. Diabetes mellitus in midlife Women have higher incidence and death rates in: 2. Stroke in late life 3. Chronic obstructive pulmonary disease 4. Alzheimer's disease and other dementias 7. Kidney diseases 8. Hypertensive heart disease Women have higher incidence of: 5. Diabetes mellitus in youth | World Health Organization, 2021; Mauvais-Jarvis et al., 2020 | Programmed theory of aging Senescence theory of aging | Hormones, Sex chromosomes |
Download links
A two-part list of links to download the article, or parts of the article, in various formats.
Downloads (link to download the article as PDF)
Open citations (links to open the citations from this article in various online reference manager services)
Cite this article (links to download the citations from this article in formats compatible with various reference manager tools)
Sex differences in biological aging with a focus on human studies
eLife 10:e63425.
https://doi.org/10.7554/eLife.63425






