Infection-exposure in infancy is associated with reduced allergy-related disease in later childhood in a Ugandan cohort
Figures
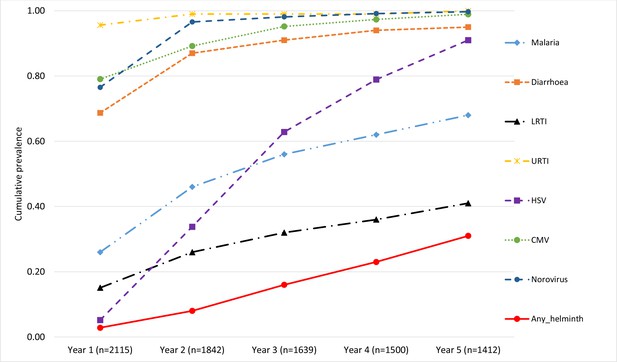
Map of Entebbe and Katabi showing the study area and the three main geographical zones of maternal residence at enrolment.
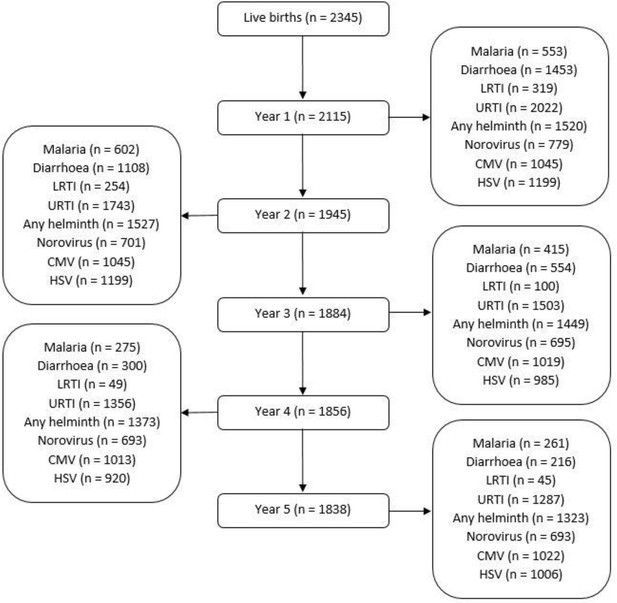
Flowchart showing number of the Entebbe Mother and Baby Study participants with data on illnesses/infections during each year.
Numbers for each year (centre column of the flowchart) represent the children who presented at the study clinic at any point during that year. Numbers for malaria, diarrhoea, lower respiratory tract infection (LRTI) and upper respiratory tract infection (URTI) represent the children who were positively diagnosed (at least once during a given year) for each of those illnesses, on presentation at the study clinic. Numbers for any helminth, norovirus, cytomegalovirus (CMV), and herpes simplex virus (HSV) represent children samples assessed for any of those infections at the respective annual visit.
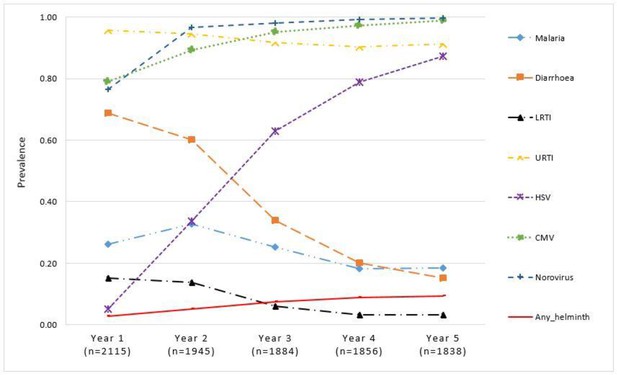
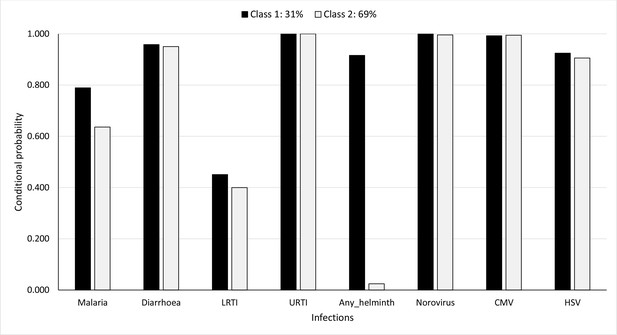
Proportion of children with illnesses/infections, over time, in the Entebbe Mother and Baby Study cohort.
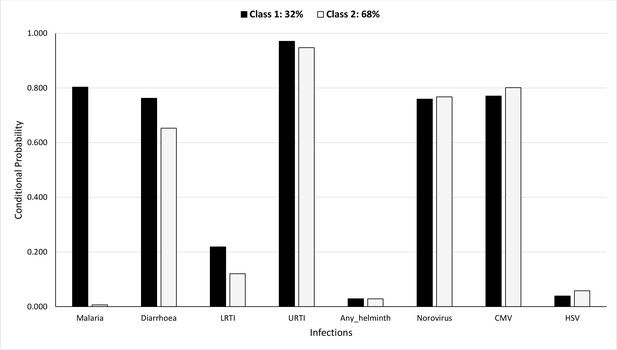
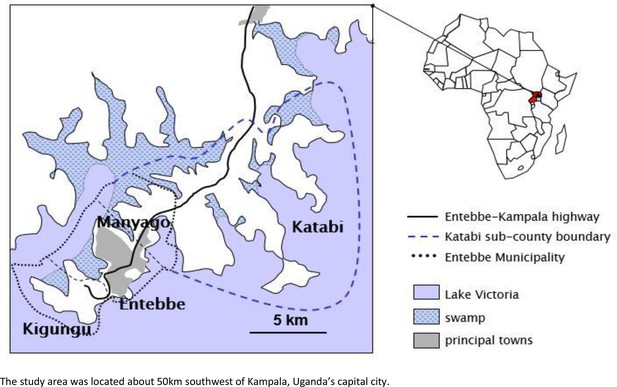
Probability of having infections conditional on latent class membership during the first year.
Tables
Number (and proportion) of children in each latent class at year 1 and at year 5 considering cumulative infection experience.
| LC 1 | LC 2 | |
|---|---|---|
| Number (%) | Number (%) | |
| Year 1 (n = 2077) | 665 (32) | 1412 (68) |
| Year 5 (n = 1668) | 517 (31) | 1151 (69) |
-
LC is latent class. LC 1 represents the class with higher probabilities for various infections as compared to LC 2, however, the profile of infections changes at each time period.
Odds ratio estimates for effects of covariates on membership in latent class 1 at year 1 and at year 5 considering cumulative infection experience.
| Year 1 exposure | 5-Year cumulative exposure | ||||
|---|---|---|---|---|---|
| Covariate | Odds ratio | (95% CI) | Odds ratio | (95% CI) | |
| Mother’s social economic status | |||||
| Higher vs. lower | 0.77 | (0.58, 1.02) | 0.51 | (0.31, 0.82) | |
| Household’s social economic status | |||||
| Higher vs. lower | 0.87 | (0.66, 1.14) | 0.58 | (0.25, 0.92) | |
| Maternal history of asthma or eczema | |||||
| History present vs. absent | 0.74 | (0.43, 1.27) | 0.50 | (0.24, 1.53) | |
| Area of residence at birth | |||||
| Kigungu vs. Entebbe | 0.33 | (0.18, 0.62) | 5.73 | (3.24, 8.12) | |
| Manyago vs. Entebbe | 1.20 | (0.88, 1.63) | 1.08 | (0.88, 1.63) | |
| Katabi vs. Entebbe | 2.43 | (1.62, 3.65) | 2.04 | (1.07, 3.54) | |
-
CI is confidence interval. Bold values indicate statistically significant values at the 5% level.
Probability of allergy-related disease (ARD) outcomes and atopy at 9 years by latent class membership at year 1.
| 95% CI* | |||||
|---|---|---|---|---|---|
| ARD outcomes at 9 years | Latent class | Estimate | Lower CI | Upper CI | p-Value |
| Wheeze | LC† 1 | 0.02 | 0.007 | 0.043 | 0.030 |
| LC 2 | 0.05 | 0.038 | 0.071 | ||
| Eczema | LC 1 | 0.03 | 0.013 | 0.056 | 0.043 |
| LC 2 | 0.06 | 0.047 | 0.084 | ||
| Rhinitis | LC 1 | 0.02 | 0.007 | 0.044 | 0.015 |
| LC 2 | 0.06 | 0.045 | 0.081 | ||
| SPT-any‡ | LC 1 | 0.22 | 0.178 | 0.278 | 0.201 |
| LC 2 | 0.27 | 0.235 | 0.304 | ||
| SPT-Dermatophagoides | LC 1 | 0.14 | 0.103 | 0.188 | 0.051 |
| LC 2 | 0.20 | 0.171 | 0.232 | ||
| SPT-cockroach | LC 1 | 0.11 | 0.074 | 0.149 | 0.760 |
| LC 2 | 0.11 | 0.091 | 0.141 | ||
| SPT-Blomia | LC 1 | 0.12 | 0.089 | 0.169 | 0.144 |
| LC 2 | 0.16 | 0.138 | 0.196 | ||
| IgE-Dermatophagoides | LC 1 | 0.26 | 0.214 | 0.322 | 0.261 |
| LC 2 | 0.31 | 0.271 | 0.343 | ||
| IgE-cockroach | LC 1 | 0.30 | 0.249 | 0.361 | 0.429 |
| LC 2 | 0.33 | 0.295 | 0.370 | ||
| IgE-any§ | LC 1 | 0.42 | 0.357 | 0.478 | 0.395 |
| LC 2 | 0.45 | 0.411 | 0.490 | ||
-
*
CI is confidence interval.
-
†
LC is latent class. LC 1 represents the class with higher probabilities for various infections as compared to LC 2.
-
‡
SPT-any is skin prick test reactivity to any of Dermatophagoides mix, Blomia tropicalis, German cockroach, cat, mould, grass pollen, Bermuda grass, or peanut.
-
§
IgE-any is allergen-specific plasma IgE (asIgE) to any of house dust mite (HDM, Dermatophagoides pteronyssinus) or German cockroach.
Probability of allergy-related disease (ARD) outcomes and atopy at 9 years by latent class membership across the first 5 years.
| 95% CI* | |||||
|---|---|---|---|---|---|
| ARD outcomes at 9 years | Latent class | Estimate | Lower CI | Upper CI | p-Value |
| Wheeze | LC† 1 | 0.02 | 0.009 | 0.065 | 0.272 |
| LC 2 | 0.05 | 0.032 | 0.066 | ||
| Eczema | LC 1 | 0.02 | 0.004 | 0.062 | 0.056 |
| LC 2 | 0.07 | 0.050 | 0.090 | ||
| Rhinitis | LC 1 | 0.02 | 0.008 | 0.067 | 0.139 |
| LC 2 | 0.06 | 0.042 | 0.080 | ||
| SPT-any‡ | LC 1 | 0.17 | 0.121 | 0.240 | 0.012 |
| LC 2 | 0.29 | 0.249 | 0.325 | ||
| SPT-Dermatophagoides | LC 1 | 0.11 | 0.069 | 0.169 | 0.010 |
| LC 2 | 0.21 | 0.180 | 0.248 | ||
| SPT-cockroach | LC 1 | 0.08 | 0.048 | 0.135 | 0.184 |
| LC 2 | 0.12 | 0.099 | 0.154 | ||
| SPT-Blomia | LC 1 | 0.11 | 0.070 | 0.169 | 0.096 |
| LC 2 | 0.17 | 0.143 | 0.206 | ||
| IgE-Dermatophagoides | LC 1 | 0.32 | 0.256 | 0.398 | 0.416 |
| LC 2 | 0.28 | 0.247 | 0.325 | ||
| IgE-cockroach | LC 1 | 0.34 | 0.271 | 0.414 | 0.658 |
| LC 2 | 0.32 | 0.279 | 0.359 | ||
| IgE-any§ | LC 1 | 0.48 | 0.403 | 0.555 | 0.316 |
| LC 2 | 0.43 | 0.386 | 0.471 | ||
-
*
CI is confidence interval.
-
†
LC is latent class. LC 1 represents the class with higher probabilities for various infections as compared to LC 2.
-
‡
SPT-any is skin prick test reactivity to any of Dermatophagoides mix, Blomia tropicalis, German cockroach, cat, mould, grass pollen, Bermuda grass, or peanut.
-
§
IgE-any is allergen-specific plasma IgE (asIgE) to any of house dust mite (HDM, Dermatophagoides pteronyssinus) or German cockroach.
Additional files
-
Supplementary file 1
Additional results tables for model fit statistics and measurement invariance for year 1 and year 5 cumulative infection experience.
(a) Model fit statistics for latent class analysis at year 1 and at year 5 considering cumulative infection experience. (b) Results for measurement invariance by sex, at year 1 and at year 5.
- https://cdn.elifesciences.org/articles/66022/elife-66022-supp1-v1.docx
-
Transparent reporting form
- https://cdn.elifesciences.org/articles/66022/elife-66022-transrepform1-v1.pdf
-
Reporting standard 1
STROBE checklist.
- https://cdn.elifesciences.org/articles/66022/elife-66022-repstand1-v1.pdf