Equity, Diversity and Inclusion: Mental health in medical and biomedical doctoral students during the 2020 COVID-19 pandemic and racial protests
Abstract
Concerns about the mental health of students, trainees and staff at universities and medical schools have been growing for many years. Recently, these have been exacerbated by the COVID-19 pandemic and a period of heightened reckoning and protests about systemic racism in the United States in 2020. To better understand the mental health of medical students and biomedical doctoral students at the University of North Carolina at Chapel Hill during this challenging period, we performed a cross-sectional study (n=957) using institutional annual survey data on measures of depression, anxiety, hazardous alcohol use, problems related to substance use, and suicidal ideation. These data were collected in 2019 and 2020, and were analyzed by type of training program, race/ethnicity, gender, sexual orientation, and survey year. Results indicated significant differences for rates of depression, anxiety, and suicidal ideation, with biomedical doctoral students showing greater incidence than medical students, and historically excluded students (e.g., people of color, women, LGBQ+ trainees) showing greater incidence compared to their peers. Of note, mental health remained poor for biomedical doctoral students in 2020 and declined for those belonging to historically excluded populations. The high rates of depression, anxiety, and suicidal ideation reported suggest that training environments need to be improved and support for mental health increased.
Introduction
Graduate and professional programs in the biomedical and health sciences are stressful environments for junior researchers and clinicians. Indeed, the mental health of medical students declines during medical school and is worse than that of the general population by graduation (Dyrbye et al., 2005; Dyrbye et al., 2006; Brazeau et al., 2014). In fact, poor mental health in medical education is evidenced by a robust, decades-old body of literature, including a systematic review of mental health evidence-based research encompassing nearly 200 relevant studies to date (e.g., Slavin et al., 2014; Rotenstein et al., 2016; Quek et al., 2019).
In comparison, evidence-based research on mental health of doctoral students has only begun to emerge over the past five years. Recent reports indicate elevated rates of anxiety and depression among graduate students in all disciplines (UC Berkeley Graduate Assembly, 2014; Evans et al., 2018; Nagy et al., 2019; Levecque et al., 2017). For example, a multi-campus study of undergraduate and graduate students found that 17.3% scored positive for depression, 9.8% scored positive for anxiety, and 6.3% reported suicidal ideation (Eisenberg et al., 2013). One study found that graduate students in the Faculty of Medicine at the University of Calgary have higher anxiety and depression than undergraduates (Toews et al., 1993), and a survey of graduate students at a university in the United States showed that approximately half of respondents reported emotional or stress-related problems (Hyun et al., 2006). In an international sample of Masters’ and PhD students, 39% of respondents indicated moderate to severe depression, and 41% moderate to severe anxiety scores (Evans et al., 2018). In comparison, the Centers for Disease Control and Prevention (CDC) estimate that approximately 16% of adults in the United States experience anxiety, and approximately 5% depression. Moreover, approximately 1 in 6 Americans will experience depression in their lifetime, and more women than men experience anxiety (CDC, 2021; Terlizzi and Villarroel, 2020). However, while these general population incidences can be informative as a benchmark, these rates are not truly comparable to the student population due to multiple potential confounding factors (e.g., age group, socio-economic status, education levels of graduate level students, etc.).
Less is known about the mental health of biomedical doctoral students specifically, as disparate disciplines are often combined when graduate students are included in student mental health studies. Still, these students train in environments which may feature long work hours, pressures to produce, influential and sometimes unsupportive relationships with advisors, as well as financial concerns, uncertainty about future employment, and non-transparent university processes which may all negatively impact doctoral student mental health (Hazell et al., 2020; Mackie and Bates, 2019).
Of note, some studies highlight that Asian, Black, Hispanic, and multi-racial undergraduate students score higher for depression than white students (Eisenberg et al., 2013). Many theories have attempted to account for these racial and ethnic disparities, such as the effects of structural racism on symptoms, diagnosis, treatment and access to care (Kendi, 2019) and the use of white populations as the baseline norm (Legha and Miranda, 2020; for review see Conrad, 2022). Additionally, studies based on data from the national survey on drug use and health have shown ongoing mental health disparities among people identifying as Black, Indigenous, and people of color (BIPOC), women, and lesbian, gay, bisexual, and queer (LGBQ+) people (SAMHSA, 2021). These populations are also particularly at risk in academia due to structural inequities, barriers, and microaggressions among other challenges (for example, academic cultural barriers and stressors for BIPOC, Halsey et al., 2020; barriers for women doctoral students, see Carter et al., 2013; LGBQ+ academics experience toxic environments and microaggressions, see Beagan et al., 2021 and Linley and Nguyen, 2015) that can impact the mental health of these populations. To acknowledge the systemic barriers faced by historically excluded groups, and to recognize that people of certain backgrounds were intentionally excluded from parts of American society for various political, economic, and social reasons (e.g., Berhe et al., 2021; Rollnick, 2015) the terms ‘historically excluded by race/ethnicity, gender, or sexual orientation’ will be used to refer to these groups respectively. While the list of historically excluded groups is not comprehensive, we aim to decenter Whiteness by referring to historically excluded (HE) versus non-historically excluded (NHE) groups.
The COVID-19 pandemic has resulted in globally increased symptoms of anxiety, depression, post-traumatic stress disorder and psychological stress, particularly among healthcare workers, those with pre-existing mental health conditions, women, college students, and individuals under 45 (Xiong et al., 2020). Furthermore, it may also have impacted mental health during academic training (Byrom, 2020). Compounding systemic inequities and racial injustice, COVID-19 disproportionally impacted communities of color in the United States (Li, 2020; Webb Hooper et al., 2020; CDC, 2020). In particular, the highest risk of age-adjusted mortality during COVID was identified for Hawaiian and other Pacific Islander, American Indian or Alaska Native, and Latinx or Hispanic people (Feldman and Bassett, 2021).
While students themselves may be classified as associated with some lower risk groups for direct effects of COVID due to their levels of education, families of students identifying as BIPOC may be disproportionately affected, especially when intersecting with risk factors associated with social class (e.g., Pathak et al., 2021; Feldman and Bassett, 2021). Hence, students historically excluded because of their race and ethnicity (also termed persons excluded due to ethnicity or race, see Asai, 2020) may experience disproportionate impact and heightened concerns about individual, community and family health (Pathak et al., 2021; Feldman and Bassett, 2021; Limas, 2021; Blake et al., 2021). Indeed, a recent longitudinal study on undergraduates at the University of North Carolina at Chapel Hill (UNC-Chapel Hill; same location as the present study) found that the prevalence of anxiety and depression increased among first-year undergraduate students of color, sexual minority students, and women-identifying students during the pandemic (Fruehwirth et al., 2021).
Moreover, the stress caused by the COVID-19 pandemic coincided with heightened responses and protests against the persistent racial injustice found in the United States – notably killings of Black Americans by police and vigilantes. These also took place alongside heightened anti-Asian violence, which may have also affected the mental health of Asian American students within academia.
At UNC-Chapel Hill, a large public university in the United States, the pandemic impacted courses and degrees in different ways. Most biomedical doctoral programs require didactic classes in the first two years only; afterwards students require full-time laboratory access to continue their research for another three to four years, precluding a transition to fully online instruction. Due to health and safety measures, biomedical doctoral student training was severely curtailed at our institution in the spring of 2020, and students returned to labs in June 2020 with strict occupancy limits. In contrast, medical student training is characterized by two years of didactic coursework and frequent test-taking, followed by another two years of sequential clinical experiences in hospitals or other clinical settings. In 2020, medical students could continue their academic progress with online learning options fostered by a switch to remote instruction in place of didactic in-person courses and clinical rotations. Hence, these students were temporarily removed from clinical rotations due to shortages of personal protective equipment; conversely though, graduation dates were not delayed.
Given this background, we sought to examine effects of the concurrent COVID-19 pandemic and heightened community reactions to racial injustice between 2019 and 2020 by exploring the mental health of medical students and biomedical doctoral students at UNC-Chapel Hill. We investigate comparisons between historically excluded (HE) and non-historically excluded (NHE) groups in science, focused on race/ethnicity, gender, and sexual orientation in medical and graduate biomedical students during the intersection of the COVID-19 pandemic and a time of reckoning of persistent racial injustice. Recognizing that an intersectional approach encompasses a multitude of identities (Cho et al., 2013), the facets of identity explored in this study are not intended to be comprehensive, but rather to represent major subpopulations represented in our sample and commonly found in US biomedical graduate and medical education.
Methods
The UNC-Chapel Hill School of Medicine annually enrolls approximately 800 medical and 600 biomedical PhD students; part of the student body is representative of diverse identities including trainees from a variety of racial and ethnic groups, genders and LGBQ +identities. For example, a recent report (UNC School of Medicine Office of Diversity Equity and Inclusion, 2021) indicated that the medical student population at UNC-Chapel Hill consisted of 54% women, 58% white, 14% Asian, and 24% underrepresented students (4% not reported); the biomedical graduate student population consisted of 57% white, 15% Asian, and 26% underrepresented students (2% not reported). The present study was reviewed and approved by the Institutional Review Board (#18–0112).
The annual School of Medicine survey used for this study includes self-reported mental health status (examined in this work), as well as assessment of current and desired student-support programs. It is conducted to inform current and future mental health and wellness programming and global satisfaction with services provided (https://doi.org/10.17605/OSF.IO/H9UCX). The same School of Medicine survey was administered to medical and biomedical doctoral students approximately one year apart in 2019 and 2020 (n=431, Fall 2020; n=526, Fall 2019). Each survey was open for four weeks between September and October and distributed using the same mechanisms (e.g., same internal listservs) to be as comparable as possible.
In the primary analysis, mental health data was analyzed by type of training program (MD vs. PhD; that is, medical students vs. biomedical doctoral students), year (2019 vs 2020), and historically excluded vs. non-historically excluded (HE vs NHE) populations based on race/ethnicity (HE-RE vs. NHE-RE) and gender (HE-G vs. NHE-G, that is students identifying as women vs. men). A post hoc analysis included the primary variables as well as historically excluded on the basis of sexual orientation (HE-SO vs. NHE-SO, that is LGBQ+ vs. non-LGBQ+ populations).
Measures
Demographic data including race/ethnicity were collected. In some cases, partial survey data was recorded (n=957 total responses; n=931 completed the survey; of those, n=740 submitted some or all demographic data). Partial surveys were used, however, only fully completed measures were included in the analysis (a blocked survey design enabled a data cleaning check that ensured participants completed each section/measure they were working on before closing the survey).
We assessed four measures of mental health (depression, anxiety, hazardous alcohol use, and problems related to substance use) using widely utilized and validated questionnaires. For each of these four measures, the values of responses were summed and sorted into categories of increasing severity ranging from 0 (indicating a lack of presentation of symptoms/no problematic substance use) to 3 or 4 (indicating increasing population-normed levels of severity for each variable), and then recoded into no symptoms (0) versus any symptoms (1). Depression scores/categories were calculated using the Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001); anxiety scores/categories were calculated using the Generalized Anxiety Disorder Assessment (GAD-7; Spitzer et al., 2006); hazardous alcohol use was assessed using the Alcohol Use Disorder Identification Test (AUDIT; World Health Organization, 2001); problems with drug use was assessed by the Drug Abuse Screening Test (DAST-10; Skinner, 1982; Yudko et al., 2007; see Table 1 for details of the categories and how they were created). To assess meaningful categories of symptomatic versus asymptomatic responses, each mental health outcome measure (for depression, anxiety, alcohol use and drug use) was recoded into bivariate (0/1) variables with a value of one (1) indicating symptoms or problems with each category (see Table 1).
Coding of the four measures of mental health used in the analyses.
Each measure of mental health (depression, anxiety, hazardous alcohol use, and problems related to substance use) was examined and coded according to its respective validated scale (PHQ-9, GAD-7, AUDIT, DAST-10). The scores were recoded as interim measures based on symptom severity, from 0 to 4. These were then transferred into a clinically meaningful bivariate category (no symptoms, 0; any symptoms, 1) to facilitate the planned analysis (bivariate logistic regression).
| Measures | No Symptoms(Coded as 0) | Any Symptoms(Coded as 1) | |||
|---|---|---|---|---|---|
| Interim Recoded as 0 | Interim Recoded as 1 | Interim Recoded as 2 | Interim Recoded as 3 | Interim Recoded as 4 | |
| PHQ-9 | 1–4: Minimal or No Depression | 5–9: Mild Depression | 10–14: Moderate Depression | 15–19: Moderately Severe Depression | 20–27: Severe Depression |
| GAD-7 | 0–4: Minimal Anxiety | 5–9: Mild Anxiety | 10–14: Moderate Anxiety | 15–21: Severe Anxiety | |
| AUDIT | 0–7: Low Risk | 8–15: Hazardous | 16–19: Harmful | 20+: Possible Dependence | |
| DAST-10 | 0: No problems | 1–2: Low Problems | 3–5: Moderate Problems | 6–8: Substantial Problems | 9–10: Severe Problems |
In addition, suicidal ideation was assessed using the following three “Yes” or “No” questions: “Have you ever thought about ending your life?”; “Have you ever thought about ending your life while enrolled?”; “Have you ever thought about ending your life in the last 12 months?”.
Participants
All of the approximately 800 medical students and 600 biomedical doctoral students on campus were invited to participate in the survey each year via student listservs. Respondents included both medical and biomedical doctoral students (Fall 2020 n=431, Fall 2019 n=526, n=957 total respondents). This sample included 622 medical students, 309 biomedical doctoral students, with 26 surveys missing data, for a total of 931 completed surveys. Amongst those 931 respondents, 91 medical students were classified as HE-RE and 531 as NHE-RE; and 57 biomedical doctoral students were classified as HE-RE, with 252 being classified as NHE-RE.
Ages ranged from 18 to 40+, with the majority of students (59%) being ages 21–25 years (59% of medical students, 60% of biomedical doctoral students), followed by 35% being ages 26–30 (34% of medical students, 35% of biomedical doctoral students), and the remainder 5% being ages 31–35 (6% of medical students, 5% of biomedical doctoral students), with <1% each respectively (for both medical students and biomedical doctoral students) for ages 18–20 years and 35–40+years.
Respondents classified as belonging to NHE-RE groups identified as follows: 66% white (67% of medical students, 66% of biomedical doctoral students), 14% Asian (16% of medical students, 9% of biomedical doctoral students), or 2% other (2% of medical students, 3% of biomedical doctoral students). In accordance with National Institutes of Health definitions of ‘underrepresented’ in the biomedical, clinical, behavioral, and social sciences (National Institutes of Health, 2020), respondents were classified as belonging to HE-RE groups if they identified as follows: 7% African American (7% of medical students and biomedical doctoral students), 7% Latinx (4% of medical students, 11% of biomedical doctoral students), 2% Middle Eastern (3% of medical students, 1% of biomedical doctoral students), 1% American Indian/Alaskan Native (1% of medical students and biomedical doctoral students), and <1% Pacific Islander (<1% of medical students and biomedical doctoral students). Historically, Asian Americans have also faced exclusion from American culture, as evidenced by the Chinese Exclusion Act and the internment of Japanese Americans during the Second World War. However, Asian Americans have been well-represented in the sciences and thus are included as NHE-RE for analysis. Additionally, Middle Eastern is not an identity included in the United States Census or NIH definitions as underrepresented; however, this group is included as HE-RE due to the marginalization this population as experienced in the United States, especially in recent years and specifically over the decades following 9/11/2001 (e.g., Crawford et al., 2021; Daraiseh, 2012; Clay, 2011).
The majority of respondents identified as women (67%; 63% of medical students, 75% of biomedical doctoral students), followed by men (32%; 36% of medical students, 24% of biomedical doctoral students), and <1% other (genderqueer, gender nonconforming, gender non-binary, and transgender; equally represented across medical and biomedical doctoral students). Institutionally, the overall medical and biomedical doctoral student populations include more women than men, so these distributions are not unexpected. Women were classified as historically excluded and men as non-historically excluded. Though transgender individuals also experience mental health and substance use disparities (National Center for Transgender Equality, 2016), we were unable to include analyses in this study due the small sample size; future studies focused on the mental health and wellbeing of gender diverse people, including transgender and gender non-conforming individuals are needed.
Respondents were classified as non-historically excluded on the basis of sexual orientation (NHE-SO) if they identified as straight/heterosexual (83%; 85% of medical students, 79% of biomedical doctoral students); or historically excluded on the basis of sexual orientation (HE-SO) if they identified as bisexual (7%; 5% of medical students, 10% biomedical doctoral students), gay/lesbian (5%; 5% of medical students, 4% of biomedical doctoral students), queer (2%; 3% of medical students, 2% of biomedical doctoral students), pansexual (2%; 1% of medical students, 3% of biomedical doctoral students), asexual (1%;<1% of medical students and biomedical doctoral students), or other (1%; <1% of medical students, 2% of biomedical doctoral students).
Analysis plan
A logistic regression was conducted, including significant interaction terms, to examine the effects of each variable on mental health outcomes using a parsimonious model. Full models with main effects and interactions were run for each variable, with stepwise addition of the largest interaction terms to the main effects, until the next largest interaction term added was no longer significant. At that point, the prior model with significant main effects and any significant interactions was retained as the final model for that variable (see Source data 1).
As previously described, each mental health outcome variable was split into clinically meaningful bivariate categories for depression, anxiety, problems with drug use and hazardous alcohol use such that the baseline category (none or fewest symptoms, as defined by each scale) was coded as zero (0), and any symptoms, as defined by more or worse symptoms than the baseline category, were coded as one (1). A bivariate logistic regression model was used to assess the impact of our primary factors of interest across the medical and biomedical doctoral student populations to maintain a large sample size and sufficient power to compare historically excluded (HE) and non-historically excluded (NHE) groups pre- and during COVID-19; groups were analyzed via Race/Ethnicity (RE) and Gender (G) for the primary analysis.
Year was coded into a practically meaningful bivariate category, with pre-COVID-19 as zero (2019; 0) and during the COVID-19 pandemic and racial unrest as one (2020; 1). Finally, HE and NHE statuses (based on race/ethnicity, gender, and sexual orientation) were coded into practically meaningful bivariate categories, with endorsement of any historically excluded category being coded as one (1), whereas all others were coded as NHE using the value of zero (0).
The primary analysis included type of program (MD vs. PhD) x Year x Race/Ethnicity x Gender. A post hoc model included all these variables, with the addition of sexual orientation (all three historically excluded social identity groups; HE-RE, HE-G, & HE-SO).
Limitations
Response bias is always a consideration in cross-sectional self-report research. Relatedly, there were no matched controls, hence it is possible that sampling distributions may have differed by chance. Furthermore, it is possible that respondents differed based on how important mental health is to them, potentially skewing the sample; hence we cannot definitively evaluate the respondent sample as representative of the full population. Due to anonymous data collection and optional questions to protect participant identities, we cannot assess granular response rates by demographic characteristics. Future studies could be completed with a controlled sample matched with participant identifiers to know who in the sample is and is not responding, as this could impact findings. Nonetheless, we achieved a response rate commensurate with voluntary survey data, suggesting a typical level of participation. We also had a high percentage of women respondents, who experience higher rates of depression and anxiety compared to men respondents; however, greater response from women is not atypical of our graduate medical and biomedical doctoral student populations, which include more enrolled women than men.
While anonymized data collection was employed as a strategy to increase sample size (e.g., more participants would feel safe responding if they could be anonymous), another limitation introduced as a byproduct of this design was the inability to examine the extent of repeated participants from year to year, which would be ideal to assess and control for in future studies. Nonetheless, using a between-groups design assuming normal variation in participants, there is no reason to believe that the two samples collected should be atypical from their respective populations over the consecutive years sampled. Methodological congruence of data collection was employed to reduce systematic bias in responses from year to year. Hence, results should be interpreted with caution as we cannot assess the percentage of repeated participants from year to year, though we believe the samples to be representative of the populations at each timepoint.
Conversely, we recognize that a large number of participants responding in both samples could be problematic for assumptions of independence for the use of parametric statistics and logistic regression analysis. Because we collected data anonymously to protect respondents’ privacy, we cannot assess to what extent respondents may have participated in both years, hence results should be interpreted with caution. It would be preferable to have identifiable data and be able to use a repeated-measures design to reduce error variance. Yet, to the extent that significant findings were achieved even with the increased error variance inherent in a between-subjects design, these results likely had large enough effect sizes to be identified even given the loss of power from using a between-subjects design rather than the preferred, more sensitive within-subjects design.
Additional limitations included our lack of ability to control for other possible variables of interest such as pandemic-specific factors, years in training, and departmental affiliation or specialty area. Pandemic-specific questions were not asked because we used the same annual survey questions in 2019 and 2020 to maintain comparable responses. Department and specialty information were not asked in order to protect anonymity, to increase comfort with responding, and to maximize response rates. Yet, populations were purposefully defined by reasonably homogenous training experiences into the two major clusters of interest: medical training and biomedical doctoral training. A large portion of the sample did not complete optional demographic questions (such as number of years in training), limiting our ability to include this in the analysis. Future work should consider controlling for as many of these variables as possible.
Results
The logistic regression model identified significant differences on student mental health outcomes for depression and anxiety by year (interactions), as well as by program (biomedical doctoral students scored worse than medical students), and for those historically on the basis of race/ethnicity (HE-RE) and by gender (HE-G) (Figure 1A).
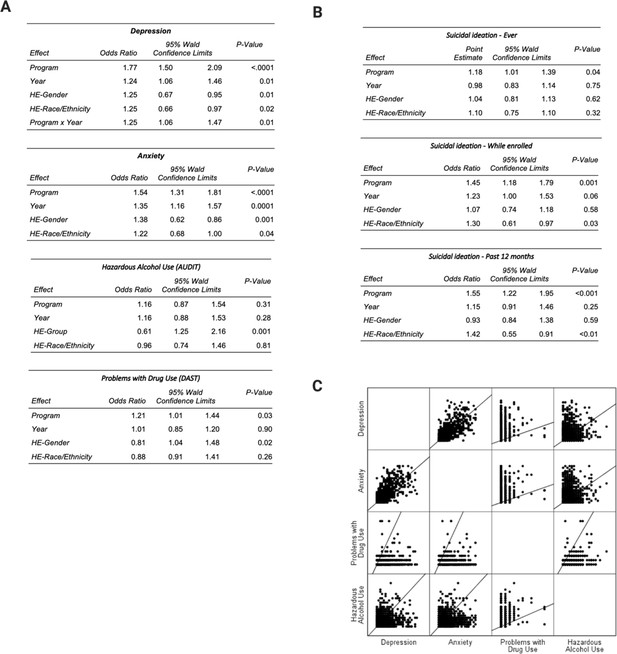
Logistic regression summary tables and correlation scatterplot matrix.
Logistic regression tables show main effects and interactions for each of the primary factors (Program, Year, HE-Gender, HE-Race/Ethnicity) across four measures of mental health (Depression, Anxiety, Hazardous Alcohol Use, Problems with Drug Use) and three measures of suicidal ideation (Ever, While Enrolled, In The Last 12 Months); the correlation matrix scatter plots illustrate the relationships between the four mental health measures. All percentages were calculated out of total valid responses; see Figure 2 for percentages. Mental health outcomes were coded into a bivariate 0/1 indicating the absence or presence of the respective symptoms for depression and anxiety (see Measures). For suicidal ideation, response options included ‘Yes’ (indicating suicidal ideations) or ‘No’ (indicating no suicidal ideations) for each of the three categories (see Methods for exact question wording). (A & B) Logistic Regression. A significant odds ratio greater than 1 indicates that the target category is more likely than the comparison group to indicate a higher score on that variable, whereas a significant odds ratio of less than 1 indicates that the target category is less likely than the comparison group to indicate a higher score on that variable. Nonsignificant effects suggest odds ratios do not show a difference greater than expected by chance (~1). If the 95% confidence interval includes 1, then the odds ratio does not differ more than expected by chance (e.g., OR = 0.98, CI95%=0.83–1.14 means there is not a significant effect of Year for Suicidal Ideation Ever); if the confidence interval does not include 1, then it differs more than expected by chance. (C) Scatterplots of the relationship between variables of interest (Depression, Anxiety, Problems with Drug Use and Hazardous Alcohol Use) displayed include graphical representations in a matrix format.
In the combined population (when medical and biomedical doctoral students are considered together) there was a decrease in depression and anxiety, likely driven by the medical student improvements; see Discussion. In general, HE-RE students exhibited significantly higher rates of depression and anxiety at about 1.5 times the rate of their NHE-RE peers across the combined medical and biomedical doctoral student sample. No differences were evidenced on either drug or alcohol use by year, type of program or historically excluded/non-excluded status.
Overall, across medical and biomedical doctoral students, HE-RE students were approximately twice as likely to say they had thought about ending their life in the last 12months than their NHE-RE peers, and about 1.8 times more likely while enrolled (Figure 1B); such high rates are extremely concerning. Due to different patterns emerging for training type and racial/ethnic identity by year, examining effect solely by year obscured these differences, hence interactions were further explored.
Depression and anxiety
Surprisingly, for medical students, there was a significant decrease in depression and anxiety between 2019 and 2020 (P<.001), whereas doctoral students observed no change between years. However, HE-RE students differed from their NHE-RE peers, being significantly more likely to be depressed (P<.02) and anxious (P<.04). Women (HE-G) exhibited higher depression and anxiety scores than men (NHE-G) consistent with known mental health trends; hence these effects are controlled for in the analyses.
Problems with drug use and hazardous alcohol use
No significant differences of note emerged between populations or within populations (e.g., NHE/HE by Program, Race/Ethnicity, Gender) on the primary measures. Reported problems with substance use and hazardous alcohol use were comparatively low in contrast to depression and anxiety, which were more pervasive. Men (NHE-G) exhibited more problems with drug use and hazardous alcohol use than women (HE-G) consistent with known substance use trends; hence these effects are controlled for in the analysis.
Suicidal ideation
Medical students showed trends toward improvement, whereas biomedical doctoral students exhibited no change between 2019 and 2020. As compared with NH-RE peers, there were significant increase in HE-RE student suicidal ideation ‘while enrolled’ (P=.03), and ‘in the last 12 months’ (P<.01). There were no significant effects of gender on suicidal ideation (ps = .58 -.62, not significant).
Medical school versus biomedical doctoral training
Prior to 2020, both medical and biomedical doctoral students suffered from depression (46% of medical students, 65% of biomedical doctoral students) and anxiety (47% of medical students, 67% of biomedical doctoral students) at high rates (Figure 2A and B), as defined by no symptoms compared with any symptomatic categories (see Methods for categorical definitions). Doctoral student mental health in 2020 remained very poor (depression: 26% of medical students, 64% of biomedical doctoral students; anxiety: 32% of medical students, 61% of biomedical doctoral students), whereas, surprisingly, the mental health of medical students improved. Suicidal ideation ‘in the last 12 months’ among biomedical doctoral students (compared with medical students) was markedly higher, both before (11% of medical students, 16% of biomedical doctoral students) and during 2020 (6% of medical students, 19% of biomedical doctoral students).
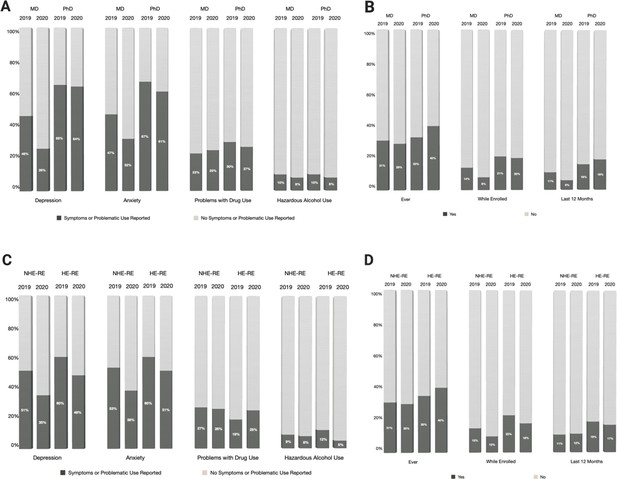
Levels of depression, anxiety, problems with drug use, hazardous alcohol use and suicidal ideation based on type of training and historically excluded status linked to race/ethnicity.
(A) Percentages of medical (MD) and biomedical doctoral (PhD) students reporting the presence (dark grey) or absence (light grey) of symptoms/problematic use pertaining to depression, anxiety, problems with drug use and hazardous alcohol use. (B) Percentages of medical (MD) and biomedical doctoral (PhD) students in 2019 and 2020 reporting having had (dark grey) or not having had (light grey) suicidal thoughts ever, in the last 12 months or while enrolled. (C) Percentages of historically excluded and non-historically excluded students based on race and ethnicity (HE-RE vs HE-NRE) reporting the presence (dark grey) or absence (light grey) of symptoms and problematic use pertaining to depression, anxiety, problems with drug use and hazardous alcohol use. HE-RE students showed higher rates of depression in both 2019 (60% of HE-RE, 51% of NHE-RE) and 2020 (48% of HE-RE, 35% of NHE-RE). This pattern was also seen for anxiety (in 2019: 60% of HE-RE, 53% of NHE-RE; in 2020: 51% of HE-RE, 38% of NHE-RE). (D) Percentages of historically excluded and non-excluded students based on race and ethnicity (HE-RE vs HE-NRE) reporting, in 2019 and 2020, having had (dark grey) or not having had (light grey) suicidal thoughts ever, in the last 12 months or while enrolled. Historically excluded students exhibit higher rates of suicidal ideation, in particular ‘while enrolled’ and ‘during the last 12 months’ (2019, positive responses for ‘while enrolled’: 23% of HE-RE, 15% of NHE-RE; positive responses for ‘during the last 12 months’: 19% HE-RE, 11% NHE-RE; 2020, positive responses for ‘while enrolled’: 18% of HE-RE, 10% of NHE-RE; positive responses for ‘during the last 12 months’ 17% HE-RE, 12% NHE-RE). All percentages were calculated out of total valid responses. HE-RE students were coded as such if they indicated that they belonged to historically excluded racial or ethnic categories (e.g., African American/Black, Hispanic/Latinx; see Methods for details); NHE-RE included students who did not indicate a marginalized racial/ethnic identity.
We assessed differences between medical and biomedical doctoral students for depression (PHQ-9), anxiety (GAD), problematic drug use (DAST), and hazardous alcohol use (AUDIT) using nominal outcome variables (Figure 2A and B). We identified significantly higher rates of depression and anxiety for biomedical doctoral students compared with medical students, as well as higher rates of suicidal ideation ‘while enrolled’ and ‘in the last 12 months’. No significant differences emerged for problems with drug use or hazardous alcohol use by training type, year, or historical exclusion by race/ethnicity; furthermore, problems with drug use rates were comparatively low in contrast to depression and anxiety. Known gender effects were consistent with expectations for both problematic substance use categories (greater use found in prior studies is also reflected in our sample for NHE-G vs. HE-G).
Historically excluded versus non-historically excluded students based on race/ethnicity (HE-RE vs. NHE-RE)
Mental health results for groups historically and non-historically excluded on the basis of race/ethnicity (HE-RE vs. NHE-RE) across a combined pool of biomedical doctoral students and medical students were also compared (Figure 2C and D). In both 2019 and 2020, HE-RE students experienced higher rates of depression and anxiety compared to their NHE-RE peers (Figure 2C and D). Suicidal ideation was also worse for HE-RE students as compared with their NHE-RE peers, specifically ‘while enrolled’ and ‘in the last 12 months’. In summary, HE-RE outcomes in general were worse for depression and anxiety (Figure 2C), as well asthese students experiencing more suicidal ideation ‘while enrolled’ and ‘over the last 12 months’ (Figure 2D).
While individuals identifying as Asian are well-represented in the academic workforce, 2020 saw an increase in anti-Asian violence, which led us to conduct additional analyses to compare the mental health of Asian American and HE-RE students in 2019 and 2020. People who identified as of Asian descent generally scored better than other NHE-RE or HE-RE groups, indicating fewer mental health challenges on all four outcome variables and the three suicidal ideation variables. However, conditional odds ratios based on these models indicated some changes by year that may be associated with the negative psychosocial and environmental factors many Asian Americans experienced between 2019–2020. Accounting for the effect of race (3-level: HE-RE Asian, HE-RE Non-Asian, HE-NRE) while controlling for year, type of training and gender, Asian American participants showed greater mean depression scores (P<.03) and anxiety scores (P<.04) in 2020 compared with 2019; there was no change in either alcohol use (P=.07, though marginal) or drug use (P=.28). There were no significant changes in conditional probabilities for suicidal ideation of Asian American participants during that time.
Associations
A robust positive association was evident between depression and anxiety (r=.69, P<.001), not surprisingly as these conditions are often comorbid. Both depression (r=.14) and anxiety (r=.33) were associated with problems with drug use (ps <.001). Neither depression (r=-.01, P=.74) nor anxiety (r=-.01, P=.77) were associated with hazardous alcohol use. Since this was only correlational in nature, a causal direction cannot be determined; nonetheless, these associations may indicate a connection between problems with drug use either as a precursor to or as an effect of experiencing mental health symptoms.
Post hoc analysis: historically excluded versus non-historically excluded students based on sexual orientation (HE-SO vs. NHE-SO)
To further examine additional aspects of intersectionality, we completed a post hoc analysis including LGBQ+ identities (HE-SO) into a simplified model (controlling for main effects of the four primary variables and identifying any significant two-way interactions). Due to a smaller sample size, this was included as a post hoc analysis.
The HE-SO variable showed significant main effects across main outcome variables, with HE-SO participants more than twice as likely to experience depression (OR = 2.19, P<.0003) and anxiety (OR = 2.66, P<.0001). In addition, there was a significant interaction with ‘Year’ for depression (P=.03), such that 2020 was significantly worse for HE-SO depression than 2019.
There were also main effects for alcohol use (OR = 2.31, P<.01) and drug use (OR = 2.37, P<.0002), such that HE-SO participants were more at risk for substance use; however, an interaction between gender and sexual orientation (P=.03) indicated that among HE-SO participants, NHE-G (LGBQ +men) were more likely to report drug use than HE-G participants (LGBQ+ women; conditional OR = .29, P<.003). HE-SO NHE-G participants (LGBQ+ men) compared to NHE-SO HE-G participants (LGBQ+ women) were nearly four times as likely to report drug use (conditional OR = 3.91, P<.0002), whereas HE-SO HE-G participants (LGBQ+ women) were not significantly more likely to report drug use (P=.19).
HE-SO participants experienced more suicidal ideation (ever, OR = 4.37, P<.001; while enrolled, OR = 3.66, P<.0001; in the last 12 months, OR = 4.77, P<.0001; see Figure 3 for visualization of comparative percentages). In addition, there was a marginal interaction between ‘HE-SO’ and ‘Program’ (P=.05), such that medical participants were much less likely (OR = .25) than biomedical doctoral students to indicate suicidal ideations while enrolled. Hence, biomedical doctoral HE-SO participants were almost six times more likely to report suicidal ideations than NHE-SO biomedical doctoral participants while enrolled (conditional OR = 5.94, P<.0001) whereas HE-SO medical students where about twice as likely to indicate suicidal ideations while enrolled than NHE-SO medical students (conditional OR = 2.925, P<.02).
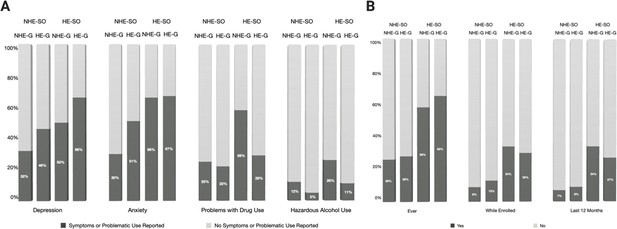
Levels of depression, anxiety, problems with drug use, hazardous alcohol use, and suicidal ideation for historically excluded/non-excluded populations based on gender and sexual orientation.
Graphical representation displaying the percentages for each of the two primary factors in this figure (Gender and Sexual Orientation) across the four measures of mental health and three measures of suicidal ideation for populations historically excluded on the basis of sexual orientation or gender (HE-SO and HE-G). All percentages were calculated out of total valid responses. Historically excluded versus non-historically excluded students based on sexual orientation (HE-SO vs. NHE-SO) were compared. Members of the HE-SO group were classified as such if they indicated an excluded identity (e.g., Lesbian, Bisexual, Queer – LGBQ+ sexual orientation; see Methods for details); NHE-SO included any students who did not indicate a historically excluded identity. Historically excluded on the basis of gender included women; non-historically excluded students by gender included men (HE-G vs. NHE-G). (A) Percentages of LGBQ+ (HE-SO) and non-LGBQ+ (NHE-SO) men and women (NHE-G vs. HE-G) reporting the presence (dark grey) or absence (light grey) of symptoms and problematic use pertaining to depression, anxiety, problems with drug use and hazardous alcohol use. (B) Percentages of LGBQ+ (HE-SO) and non-LGBQ+ (NHE-SO) men and women (NHE-G vs. HE-G) reporting having had (dark grey) or not having had (light grey) suicidal thoughts ever, in the last 12 months or while enrolled.
Discussion
Overall, medical student mental health improved from 2019–2020 on measures of both depression and anxiety, whereas biomedical doctoral students showed no change, their scores remaining concernedly high. HE-RE students were worse off than their NHE-RE peers in measures of depression, anxiety, and suicidal ideation – particularly reporting more suicidal ideation than their counterparts both ‘while enrolled’ and in the ‘last 12 months’. All analyses controlled for gender, for which women (HE-G) generally experienced anxiety and depression more than men (NHE-G), whereas men generally reported higher substance use. Post hoc analyses also indicated that those identifying as HE-SO (LGBQ+ respondents) experienced more anxiety and depression than NHE-SO (non-LGBQ+) respondents, as well as greater suicidal ideation.
Trends in medical students versus biomedical doctoral students
Despite unique challenges between 2019 and 2020, many metrics of medical student mental health improved. In mid-March of 2020, medical students were pulled from clinical settings and from typical coursework due to the pandemic. Usual academic and clinical responsibilities were replaced with a four-week online course named ‘Medical Management of COVID-19’, which focused for instance on wellness, self-care, medical management and personal protective equipment related to COVID-19 (UNC Health and UNC School of Medicine, 2020). It is possible that the pause in traditional medical student training and the new course focused on timely topics mitigated stress-induced mental health erosion. In contrast, biomedical doctoral students did not receive any similar interventions addressing emerging COVID knowledge or mental health coping strategies.
Furthermore, medical students at our institution were able to continue some form of their training remotely, to maintain some social contact and peer support networks through academic training, and to avoid graduation delays. Additionally, while medical students pay for their training, which could contribute to financial stress, these financial demands did not change between 2019 and 2020. This consistency of circumstances, combined with expectations of income post-graduation and a near-guarantee of eventual employment in medicine, could also have mitigated the downward trend in medical student mental health. Furthermore, we also speculate that being in a medical training program with obvious direct impact during a time when medical professionals were publicly celebrated (at least initially) had a positive effect on the mental health of medical students.
Finally, and in contrast to biomedical doctoral programs, medical school accreditation bodies mandate and enforce the presence of more structured mental health and wellness support systems, ensuring that support services for medical students are more easily accessible and freely available (no cost, and/or available funding to cover any out-of-pocket mental health medical expenses). At our institution, both medical and biomedical doctoral students have limited access to facilitated and triaged on-campus resources; however, while the equivalent of 1.5 person working full time is dedicated to support the ~800 medical students (e.g., 533:1 student-counsellor ratio), the ~600 biomedical doctoral trainees only have access to the equivalent of 0.5 full-time employee dedicated to their support (e.g., 1200:1 student-counsellor ratio). The more robust support for medical students, combined with being removed from the acute stressors often encountered in rotations (due to being pulled from clinical duties during the pandemic) may have magnified the ameliorative effect of the cohort-based intervention that medical students received.
In contrast to medical students, biomedical doctoral students exhibited alarmingly high levels of depression and anxiety that dwarfed the rates in the medical student population, which were themselves higher than in the general population. This is similar to previous findings (e.g. Evans et al., 2018), even accounting for COVID trends (see Gordon, 2021). When considering recent suicidal ideation in particular, the mental health of biomedical doctoral student worsened between 2019 and 2020. This may be linked to changes imposed on biomedical doctoral student training: laboratory research had to be stopped and lab occupancy was then restricted in Spring 2020, which reduced supportive social interactions and peer camaraderie. The loss of progress on dissertation projects (given that graduation times are open-ended) was frustrating and may have exacerbated mental health issues. In addition, the concurrent economic recession may have depressed optimism about job opportunities for biomedical doctoral students, who pursue a much wider range of careers after graduation compared to medical students. The dismissal of science by politicians and the media, popular sentiments against public health policies based on scientific recommendations and public degradation of trust in science and scientists may have all contributed to a worsened experience for biomedical scientists (e.g., Couée, 2020; Gross, 2020; Kreps and Kriner, 2020).
For biomedical doctoral students whose research was not directly related to COVID-19, it may have been harder to find meaning and purpose in their formerly satisfying research on other diseases. Anecdotally, some biomedical doctoral students sought opportunities to volunteer their skills in molecular biology in diagnostic COVID-19 labs, indicating a desire to contribute to the immediate crisis. In contrast, medical students may have found it easier to connect their training with the real-world crisis of COVID-19. Moreover, when labs were shutting down, medical education shifted to COVID-19 prevention topics directly related to the pandemic.
Additionally, medical students will soon become medical doctors in a society where this profession took center stage. On the other hand, the success of the vaccine effort – which received praise but also backlash – may yet improve how basic research scientists are considered in society in the coming years (Bogel-Burroughs, 2020; Kauer, 2020; Kolata, 2021). Future education and mental health research should delve into the aspects of medical education versus biomedical doctoral training that drive different mental health outcomes during a crisis and in normal times.
Mental health trends for student from historically excluded racial or ethnic groups
Irrespective of medical or doctoral program, mental health metrics for depression, anxiety and suicidal ideation were worse for students from historically excluded groups based on race/ethnicity compared to students from non-historically excluded racial groups, and they worsened between 2019 and 2020. Overall, the incidence of suicidal thoughts for HE-RE students increased proportionately both ‘while enrolled’ and ‘in the last 12 months’ compared with NHE-RE students, and particularly for biomedical doctoral HE-RE students ‘in the last 12 months’. We hypothesize that the COVID-19 pandemic and heightened racial unrest contributed to these differences, although future research is needed to isolate the factors causing the observed effects. This result may be partially explained by the added stressors of systemic racism in academic, medical, and American cultures. Academic culture, in particular, is based on norms that systematically exclude minority groups and create additional mental health challenges for people of color (e.g., persons excluded due to ethnicity or race, see Asai, 2020).
Associations
Our finding that depression was correlated with both anxiety and problematic drug use was consistent with previous work which demonstrates common comorbidity of depression and anxiety, as well as of substance use disorders with mental illness (e.g., National Institute on Drug Abuse, 2010); hence, it is plausible that problematic drug use could represent a contributing factor and/or a coping strategy for depression but this should be interpreted with caution. Furthermore, the lack of association in our sample between hazardous alcohol use and mental illness was surprising given the common associations found between these variables in previous work (e.g., Smith and Randall, 2012; McHugh and Weiss, 2019).
Mental health trends for students belonging to groups historically excluded because of sexual orientation
Our findings that LGBQ+ students experience worse mental health outcomes align with national studies showing that sexual minorities are approximately twice more likely than heterosexual people to experience mental health conditions such as anxiety, depression, suicide, and substance use (Medley et al., 2016; SAMHSA, 2020; SAMHSA, 2021). Similar to national trends, gender interacted with sexual orientation to indicate worse effects for LGBQ+ women for depression and anxiety, but worse substance use for LGBQ+ men. While our small sample suggests that these results should be interpreted with caution, the large effect size evident in our analysis was extremely concerning and indicates a crucial need for studies to further examine this population and how it could be better supported. In addition, our inability to evaluate these hypotheses for transgender and gender non-conforming students (due to an insufficient sample size to run a parallel analysis) was a limitation. This should certainly be evaluated in future studies, especially due to transgender people being at increased risk and incidence for mental health problems, as evidenced nationally (National Center for Transgender Equality, 2016).
Conclusions and recommendations
Whereas medical schools have had mental health recommendations in place since 1992 (AAMC Executive Council, 1992; enforced by the Liaison Committee on Medical Education accreditation standards), biomedical doctoral programs have had no such parallel policies regarding mental health provisions nationwide. Our new data suggest a need for swift action to address the very urgent mental health needs of biomedical doctoral students both before and during the COVID-19 pandemic, especially for students who have been traditionally excluded from the academy based on their gender, race/ethnicity, and sexual orientation. Furthermore, the data we present suggests that depression, anxiety, and suicidality for historically excluded medical and biomedical research students have been exacerbated during the ongoing COVID-19 pandemic and climate of heightened visibility of racial inequity. Future studies should explore additional disparities between historically and non-historically excluded students in addition to those highly concerning trends.
It is crucial, now more than ever, to provide mental health support both on campus and remotely to ensure that students have access to the mental health services they need (see Krause and Harris, 2019). On-campus mental health resources should reflect the diversity of the student body, including in terms of race/ethnicity and sexual orientation. Meanwhile, mental health resources, communities, and support groups are starting to emerge online (e.g., PhDBalance, TAE Consortium, RVoice).
While offering more resources is an important step, the increasing national demand for mental health services on university and college campuses may make it difficult to provide comprehensive mental health care to all students who need it (Seppälä et al., 2020). In addition, simply providing services and programs may not be enough due to inequitable access to these resources and systemic issues that negatively impact mental health outcomes. Preventative health measures should therefore be investigated at the graduate level, particularly regarding the learning environment. Prevention, wellness resources, LGBTQ+ Safe Zone, anti-racism and resiliency training as well as assessment of impact are crucial to reduce the acute need for mental health support, including substance use.
Given the higher indicators of distress, the factors driving the mental health crisis, particularly for BIPOC students, those from gender and sexual minorities, and biomedical doctoral students, should be identified. Some potential causes to explore include toxic work environments, systemic racism, sexism, homophobia and unhealthy cultural and academic norms. In addition, the following factors contribute to historical exclusion based on race and ethnicity: bullying and harassment, precarity of work contracts in higher education, science inequities based on barriers and limitations to diversity, inclusion, and accessibility, and a disproportionate effect of the competitive culture in academia on historically excluded groups (Limas et al., 2022; Limas, 2021). Researchers must continue to examine how these and other factors may contribute to negative experiences for historically excluded groups particularly, and to extend this research to proposing, implementing and evaluating needed programmatic and policy changes empirically. This should also include evidence-based research focused on the mental health of faculty and staff to better cater to this population’s needs, as well as to recognize and improve the support they provide to students (e.g., Loissel, 2019; Loissel, 2020).
While individual protective measures can alleviate some negative impacts of operating within a flawed system (e.g., the academic environment), systemic change must occur rather than relying on those most likely to be impacted to create change (Halsey et al., 2020). It is imperative that leaders in higher education use evidence-based quantitative and qualitative research to examine population trends, create visibility for lived experience, and ultimately identify and reduce causes of mental health problems rather than just treating symptoms when they emerge. Academic culture needs to be actively reformed by those in power to model, encourage, and sustain student, faculty and staff wellbeing.
Study limitations and future directions
Limitations related to anonymous data collection include the inability to estimate exact response rates, percentage of repeated versus new respondents, or non-respondents who skipped entering demographic data. In addition, self-reported mental health status may be biased, and independent assessments by a clinician would provide greater accuracy. Importantly, given the observational nature of our data collection, many confounds could also not be accounted for which changed over the course of the year between data collection timepoints. Nonetheless we believe that our work provides a compelling starting point to further examine trends and emergent concerns in the mental health of medical and biomedical doctoral students. Even given the limitations of our dataset, the unexpectedly high rate of suicidal ideation is concerning: among respondents alone, nearly 40 trainees (16 medical students and 21 biomedical doctoral students) reported recent suicidal ideation in 2020.
Many segments of society in the United States have been intentionally excluded from social, economic, and cultural opportunities via law, policy, and cultural expectations in order for dominant groups to retain power and privilege. Some groups have explicitly and implicitly experienced more systemic barriers than others – for example, the legal discrimination against African Americans throughout American history, or the restriction of voting privileges to exclude women and non-white voters. Historically, this has been reinforced by social norms and cultural biases, even in situations when overt racial discrimination has been addressed. We recognize that race is a social construct, and that other social identity groups beyond race and ethnicity (Rothman et al., 2020) may also experience inequitable impacts of COVID-19. For instance, we noted that women and LGBTQ+ students also showed evidence of negative impacts on their mental health in the current study. We have controlled for differences by gender as well as examined effects for sexual orientation (see Salerno et al., 2020), but we recognize that these analyses are not comprehensive of all social groups experiencing inequities, and we acknowledge the impact of additional identities that we were not able to study such as, among others, international and undocumented status (Hunt, 2020; Chen et al., 2020) and disability (Goggin and Ellis, 2020; Gray et al., 2020). In fact, the NIH has recently expanded its definition of underrepresented in science to include women, people with disabilities, first-generation college students and those from disadvantaged backgrounds (including people who have experienced or are experiencing homelessness, foster care participation, recipients of free and reduced lunch, Pell grants, SNAP or WIC, and those who grew up in a low-income or rural areas; National Institutes of Health, 2020; National Institutes of Health, 2018, rescinded and replaced in 2019; National Institutes of Health, 2019).
Yet this expanded definition remains flawed as some groups are still excluded from recognition and inclusion as societal norms and practices shift over time. The concept of ‘historically excluded’ should therefore continue to evolve and be re-examined or expanded over time as warranted by newly identified historical trends. For instance, people of Middle Eastern descent have faced heightened discrimination following 9/11/2001. Students identifying as Asian may also face distinct challenges that affect their mental health among rising anti-Asian violence (e.g., Yam, 2021a; Yam, 2021b). In fact, our analyses showed that the 2019–2020 year brought additional challenges that impacted mental health in a negative direction for both depression and anxiety in this population, despite overall scores that indicate, on average, better mental health outcomes. This supports the need for examining Asian HE-RE populations separately in future work (and to contrast Asian American with white American experiences) in order to identify distinct experiences, protective factors and challenges. In sum, while not all groups nor all aspects of exclusion were represented in this paper, we aim to amplify the importance of examining multiple layers of identity and historical exclusion: future directions should include examination of the intersectionality of these and other identity groups, as well as systemic barriers that each may encounter differentially.
Furthermore, additional structural factors not accounted for herein (e.g., isolation, financial stressors, policy and law impacts) may have also exacerbated the mental health status of trainees and created systemic inequities for different groups. For instance, while data collection was completed before the 2020 election in the United States, political tensions were building throughout the summer and fall of 2020. Future research should examine the way that political cycles, economic trends and governmental policies impact trainee populations in the United States, and in particular how xenophobic, nationalist, ableist, sexist, and homophobic legislation affect the mental health of students from historically excluded communities.
Data availability
Underlying data is available on the Open Science Framework at https://doi.org/10.17605/OSF.IO/H9UCX. In accordance with IRB approval, the presentation of data does not include demographic information that could potentially lead to the identification of a student. Furthermore, to protect student anonymity, responses with fewer than ten individuals will not be shared. Accordingly, data sharing is limited to those variables directly relevant to the analyses conducted (e.g., underlying data) and composite categories (e.g., underrepresented vs. well-represented) are shared when applicable rather than granular demographic information to protect the identity of respondents also noted in in the Human Subjects section.
-
Open Science FrameworkMental health disparities among biomedical trainees during COVID-19 and racial inequity.https://doi.org/10.17605/OSF.IO/H9UCX
References
-
ExcludedJournal of Microbiology & Biology Education 21:21.1.18.https://doi.org/10.1128/jmbe.v21i1.2071
-
Microaggressions experienced by LGBTQ academics in Canada: “just not fitting in… it does take a toll.”International Journal of Qualitative Studies in Education 34:197–212.https://doi.org/10.1080/09518398.2020.1735556
-
Black, Indigenous, people of color, and international students: experiences and resolutions beyond COVID-19American Journal of Public Health 111:384–386.https://doi.org/10.2105/AJPH.2020.306118
-
WebsiteAntivaccination activists are growing force at virus protestsThe New York Times. Accessed April 5, 2022.
-
Different for women? The challenges of doctoral studiesTeaching in Higher Education 18:339–351.https://doi.org/10.1080/13562517.2012.719159
-
A black and white history of psychiatry in the United StatesThe Journal of Medical Humanities 43:247–266.https://doi.org/10.1007/s10912-020-09650-6
-
WebsiteCosts of war: racial profiling and islamophobiaBrown University Watson Institute of International Affairs. Accessed August 8, 2022.
-
Effects of Arab American discrimination post 9/11 in the contexts of the workplace and educationMcNair Scholars Research Journal 4:3.
-
Medical student distress: causes, consequences, and proposed solutionsMayo Clinic Proceedings 80:1613–1622.https://doi.org/10.4065/80.12.1613
-
Mental health in American colleges and universities: variation across student subgroups and across campusesThe Journal of Nervous and Mental Disease 201:60–67.https://doi.org/10.1097/NMD.0b013e31827ab077
-
Evidence for a mental health crisis in graduate educationNature Biotechnology 36:282–284.https://doi.org/10.1038/nbt.4089
-
Disability, communication, and life itself in the COVID-19 pandemicHealth Sociology Review 29:168–176.https://doi.org/10.1080/14461242.2020.1784020
-
WebsiteOne year in: COVID-19 and mental healthNational Institutue of Mental Health. Accessed August 8, 2022.
-
COVID-19 and the other pandemic: populations made vulnerable by systemic inequityNature Reviews. Gastroenterology & Hepatology 17:520–522.https://doi.org/10.1038/s41575-020-0330-8
-
Communicating science in a crisisCurrent Biology 30:R737–R739.https://doi.org/10.1016/j.cub.2020.06.052
-
Graduate student mental health: needs assessment and utilization of counseling servicesJournal of College Student Development 47:247–266.https://doi.org/10.1353/csd.2006.0030
-
WebsiteKati Kariko helped shield the world from the coronavirusNew York Times. Accessed April 7, 2022.
-
The PHQ-9: validity of a brief depression severity measureJournal of General Internal Medicine 16:606–613.https://doi.org/10.1046/j.1525-1497.2001.016009606.x
-
An anti-racist approach to achieving mental health equity in clinical careThe Psychiatric Clinics of North America 43:451–469.https://doi.org/10.1016/j.psc.2020.05.002
-
Work organization and mental health problems in PhD studentsResearch Policy 46:868–879.https://doi.org/10.1016/j.respol.2017.02.008
-
BookAdaptation to Overexpression of Cyclin E in Epithelial Cells Doctoral DissertationUniversity of North Carolina.https://doi.org/10.17615/6cpy-mx59
-
LGBTQ experiences in curricular contextsNew Directions for Student Services 2015:41–53.https://doi.org/10.1002/ss.20144
-
Contribution of the doctoral education environment to PhD candidates’ mental health problems: a scoping reviewHigher Education Research & Development 38:565–578.https://doi.org/10.1080/07294360.2018.1556620
-
Alcohol use disorder and depressive disordersAlcohol Research 40:arcr.v40.1.01.https://doi.org/10.35946/arcr.v40.1.01
-
Burnout and mental health problems in biomedical doctoral studentsCBE Life Sciences Education 18:ar27.https://doi.org/10.1187/cbe.18-09-0198
-
WebsiteComorbidity: addiction and other mental illnesses (NIH Publication Number 10-5771)NIDA Research Report Series. Accessed April 7, 2022.
-
WebsiteNotice of NIH’s interest in diversity (Notice Number: NOT-OD-20-031)Accessed November 22, 2019.
-
The global prevalence of anxiety among medical students: a meta-analysisInternational Journal of Environmental Research and Public Health 16:E2735.https://doi.org/10.3390/ijerph16152735
-
BookAccess of historically excluded groups to tertiary STEM educationIn: Gunstone R, editors. Encyclopedia of Science Education. Dordrecht: Springer. pp. 1–6.https://doi.org/10.1007/978-94-007-2150-0_425
-
The mental health impact of the COVID-19 epidemic on immigrants and racial and ethnic minoritiesQJM : Monthly Journal of the Association of Physicians 113:779–782.https://doi.org/10.1093/qjmed/hcaa203
-
The drug abuse screening testAddictive Behaviors 7:363–371.https://doi.org/10.1016/0306-4603(82)90005-3
-
Anxiety and alcohol use disorders: comorbidity and treatment considerationsAlcohol Research 34:414–431.
-
A brief measure for assessing generalized anxiety disorder: the GAD-7Archives of Internal Medicine 166:1092–1097.https://doi.org/10.1001/archinte.166.10.1092
-
WebsiteSymptoms of generalized anxiety disorder among adults: United StatesAccessed April 5, 2022.
-
Impact of COVID-19 pandemic on mental health in the general population: a systematic reviewJournal of Affective Disorders 277:55–64.https://doi.org/10.1016/j.jad.2020.08.001
-
A comprehensive review of the psychometric properties of the drug abuse screening testJournal of Substance Abuse Treatment 32:189–198.https://doi.org/10.1016/j.jsat.2006.08.002
Decision letter
-
Elsa LoisselReviewing Editor; eLife, United Kingdom
-
Peter RodgersSenior Editor; eLife, United Kingdom
In the interests of transparency, eLife publishes the most substantive revision requests and the accompanying author responses.
Decision letter after peer review:
Thank you for submitting your article "Mental health disparities among biomedical trainees during COVID-19 and racial inequity" to eLife for consideration as a Feature Article.
Four peer reviewers have reviewed your article, and the evaluation has been overseen by two members of the eLife Features Team (Elsa Loissel and Peter Rodgers). The following individuals involved in reviewing your submission have agreed to reveal their identity: Marcus Lambert and Amanda Haage.
The reviewers and editors have discussed the reviews and we have drafted this decision letter to help you prepare a revised submission.
Please also note that if your manuscript is accepted, we would like to publish some of the relevant code with the article: please let me know if this will be a problem.
In addition, the eLife Features Editor may also contact you separately about some editorial issues that you will need to address.
Summary:
The article aims to explore the wellbeing of medical students and biomedical PhD students at an R1 institution using self-reported markers of mental health across race/ethnicity. This work was conducted over two years, one of which was marked by the COVID-19 pandemic and a wave of racial and civil unrest. This manuscript is important and timely for a broad biomedical audience, highlighting major concerns around the prevalence of mental health challenges, especially in biomedical PhD and underrepresented students.
However, several points need to be addressed to make the article suitable for publication. In particular, the reviewers were concerned with some aspects of the methodology and the discussion.
Essential revisions:
Comparing medical and PhD students:
1 – Please consider discussing in the introduction (and the discussion) why there may be a difference between medical and biomedical PhD students. In particular, please expand on:
a. The level of institutional support provided by the respective programs: For instance, what are the mental health resources provided to medical and PhD students? Are they the same and are they easily accessible e.g. paid for? facilitated/triaged? on-campus?
b. The awareness of the two populations of their mental health (one might argue that medical students are trained to recognize certain signs and symptoms).
c. The differences that are intrinsic to their training: for example, those familiar with the medical student training process might suggest more acute stressors but more structured support due to LCME requirements.
d. The response to the COVID pandemic from the two different programs: for instance, the curriculum and/or level of support changed for the medical students in 2020, which is highlighted in the discussion. However, this is a big limitation in interpreting the data (comparatively between MD and PhD students). This can be viewed as an intervention that the PhD students did not have.
2 – Following that thought: medical and graduate students have extremely different training paradigms and, in this institution, medical students received an intervention that could have mitigated the effects of the pandemic on their mental health. Therefore, please consider whether directly comparing medical to graduate students is relevant, and if so, how to do so: for example, the bar graphs side by side are fine, but the chi-sq tests may be an unfair comparison. Or at least, please discuss the caveat of the different training paradigms and levels of support provided throughout the 2020 year.
3 – The reason why PhD students have worse PHQ9 outcomes over time comparatively is because the medical students show a decrease from 2019 to 2020. Could you please report whether you have looked at the trends across the medical student years (1 through 4), and justify if not.
Discussing the sample, and how it was coded:
4 – Line 158: Please detail the criteria for sample invitations (e.g. are there any inclusion or exclusion criteria for the study, and if so, are they the same for the 2019 and 2020 surveys?).
5 – Line 158: Please clarify whether the respondents (n=431, Fall 2020; n=526, Fall 2019) are a representative sample that closely matches the characteristics of your population. If not, please address this selection bias in the discussion.
6 – Line 166-167. "Middle Eastern", while an important subcategory, is not a part of the NIH definition of underrepresented groups. If you would like to use the NIH guidelines, please remove this subcategory from the UR coding. Alternatively, please directly justify the coding of "Middle Eastern" as underrepresented. Please see revisions #13 and #14 for further discussion about NIH guidelines.
7 – Please ensure that the in-text reported percentages and N values are easy to understand, as they are quite unclear in the current version. This is particularly the case in the "participants" section of the methods and figure legends, where it is unclear what year each number represents.
Methodological and statistical issues:
8 – The data collected in 2019 and 2020 was combined for data analysis, suggesting that some participants may have participated in both years. Logistic regression requires the observations to be independent of each other: that is, the observations should not come from repeated measurements. This could bias/inflate the results – the larger number of repeated respondents, the higher chance to obtain biased results – and it therefore needs to be carefully justified and addressed. If you can identify repeated respondents, please report how many, and justify why you think you can include them in the analysis: in addition, please consider exploring whether your findings stay the same if you take out those repeated respondents, and/or use a repeated measures design to compare the difference in mental health between 2019 and 2020. If you are not able to identify repeated respondents, please discuss this limitation.
9 – The mental health outcomes are sensitive to recent events and affected by many factors/variables (e.g., variables related to the pandemic, years in the degree, disciplines, etc.): it is possible that the mental health disparities you report might be no longer statistically significant once these covariates are included in the analysis. Please either include these covariates in your logistic regression, or explain in the manuscript why they were not included.
10 – The collected mental health measures could be treated as continuous variables, which could offer better variabilities for statistical modelling. Please clarify why you decided to simplify the scale (0 and 1) to run logistic regression analyses (binary outcome) rather than multiple regressions (continuous outcome). If you are not able to provide the reason, please make sure that both approaches (logistic regression and multiple regression) yield consistent findings.
Additional analyses and discussion points pertaining to intersectionality approaches:
11 – Please consider conducting additional analyses to explore whether they were any differences across gender identity. The N values seem similar to the other populations you have chosen to compare, and this would significantly increase the impact of this study. Otherwise, please justify why this variable was not explored.
12 – If feasible, please adopt an intersectionality approach, in particular by examining how gender AND race/ethnicity impact your findings. Otherwise, please justify why these analyses were not performed, and strengthen your discussion around intersectionality.
13 – While Asians are included as well-represented according to NIH standards, the percentage of Asian-identifying individuals in the sample (at 16% and 9%) clearly demonstrates that they are not. This is discussed at the end, but please also include these comments in the Results section and strengthen the language. In addition, please consider comparing the experiences of Asian and White students, or, if you are concerned with anonymity/statistical power, please consider comparing WR vs. UR where "Asian" is moved from WR to UR, as this would allow the reader to understand if coding "Asian" as WR vs. UR makes a difference (this does not necessarily need to be in the main part of the paper). Alternatively, please justify why these analyses were not performed.
14 – On that note: although discussed at the end, please provide a more nuanced discussion of race and ethnicity, and strengthen your stance. In particular, while it is understandable that you want to use NIH standards, please acknowledge more overtly that race is a social construct (so as to not reinforce the notion that these categories may be biological); and please discuss in more depth how the NIH categories may be lacking and not best represent a marginalized identity in science.
Strengthening certain claims
15 – Please provide evidence for the following statements:
a – Line 40 ("biomedical graduate programs are exposed to unique stressors by the nature of their training"): please consider moving up certain citations (e.g. Hazell et al., 2020 and Mackie and Bates 2019) to support this affirmation. Please also consider replacing the word "unique" as long hours, pressure to produce, and unsupportive mentors may not necessarily support a "uniquely" stressful situation.
b – Line 93 ("Trainees of color, especially people identifying as Black, Indigenous, and people of color (BIPOC), may also be affected by heightened concerns about individual, community, and family health."): While covid disparities are certainly real, and likely at play, please provide supporting evidence for this affirmation.
c – Line 340 ("We also speculate that being in a medical training program with obvious direct impact during a time when medical professionals were publicly celebrated had a positive effect on MD student mental health.") This discussion of MDs being "publicly celebrated" and "heroic" and able to connect their training to the crisis compared to PhD lacks evidence, particularly as we see protests outside of hospitals continue.
d – Line 343 ("Furthermore, medical students were able to continue some form of their training remotely, maintain some social contact and peer support networks through academic training, and avoid graduation delays.") Please provide citations for this statement, and clarify whether this is institution-specific.
e – Line 356 ("Biomedical PhD student training was severely curtailed in the 2020 spring months…"). Please clarify if this refers to specific measures at your institution.
f – Line 410 ("the mental health crisis in graduate biomedical education has only recently received considerable attention from the laboratory research community."): Please provide evidence for this statement.
https://doi.org/10.7554/eLife.69960.sa1Author response
Essential revisions:
Comparing medical and PhD students:
1 – Please consider discussing in the introduction (and the discussion) why there may be a difference between medical and biomedical PhD students. In particular, please expand on:
a. The level of institutional support provided by the respective programs: For instance, what are the mental health resources provided to medical and PhD students? Are they the same and are they easily accessible e.g. paid for? facilitated/triaged? on-campus?
b. The awareness of the two populations of their mental health (one might argue that medical students are trained to recognize certain signs and symptoms).
c. The differences that are intrinsic to their training: for example, those familiar with the medical student training process might suggest more acute stressors but more structured support due to LCME requirements.
d. The response to the COVID pandemic from the two different programs: for instance, the curriculum and/or level of support changed for the medical students in 2020, which is highlighted in the discussion. However, this is a big limitation in interpreting the data (comparatively between MD and PhD students). This can be viewed as an intervention that the PhD students did not have.
We thank the reviewers for this important point and have added the following to the discussion to address these valid critiques:
“In contrast, PhD students continued work at best, or experienced forced absence from the lab, with no specific intervention addressing emerging COVID knowledge or mental health coping strategies.”
“Furthermore, accreditation requirements for MD training provide a more structured support system for medical student mental health and wellness compared with PhD student supports. Given the difference in support offered due to enforced standards, this makes MD support services more easily accessible and freely available (no cost, and/or available funding to cover any out-of-pocket mental health medical expenses). Whereas both MD and PhD have availability of limited initial contact of facilitated and triaged on-campus resources, MDs have access to 1.5 FTE dedicated support for 800 students (e.g., 533:1 student-counselor ratio) whereas PhDs have only.5 FTE dedicated support for 600 students (e.g., 1200:1 student-counselor ratio). The combination of the more robust support for MD students with the removal of exposure to acute stressors often encountered in clinical rotations may have magnified this effect.”
2 – Following that thought: medical and graduate students have extremely different training paradigms and, in this institution, medical students received an intervention that could have mitigated the effects of the pandemic on their mental health. Therefore, please consider whether directly comparing medical to graduate students is relevant, and if so, how to do so: for example, the bar graphs side by side are fine, but the chi-sq tests may be an unfair comparison. Or at least, please discuss the caveat of the different training paradigms and levels of support provided throughout the 2020 year.
We agree that the nuanced discussion of differences between the two populations is very important, and brings to attention the point that adjustment of the training environment (e.g., MD intervention) can in fact positively impact mental health even amidst difficult times. We have replaced the post hoc chi-squared tests with a more complex logistic regression model that allows for statistical control of differences between the two populations, including marginal means and conditional odds ratios to expresses in terms of differences in each population, while simultaneously controlling for the other variables’ impact.
3 – The reason why PhD students have worse PHQ9 outcomes over time comparatively is because the medical students show a decrease from 2019 to 2020. Could you please report whether you have looked at the trends across the medical student years (1 through 4), and justify if not.
We agree that analysis by year in program would be important to include in future work; however, in our sample this was a demographic question that was not completed by a sizeable portion of respondents, which would reduce our ability to complete the main analysis if we included it. We also have concerns about including variables with a significant amount of missing data as this would potentially not be representative of the sample or population.
Discussing the sample, and how it was coded:
4 – Line 158: Please detail the criteria for sample invitations (e.g. are there any inclusion or exclusion criteria for the study, and if so, are they the same for the 2019 and 2020 surveys?).
The same listservs were used each year to recruit School of Medicine trainees in Medical Education (MD students) and Graduate Education (biomedical PhDs), as described in Methods. A standard IRB-approved invitation included a brief paragraph explaining the survey, signed by the appropriate administrator (e.g., SOM Wellness Coach). There were no formal inclusion or exclusion criteria in either year other than being enrolled in either the MD or PhD programs, and anyone included on the SOM trainee listservs was invited to respond.
5 – Line 158: Please clarify whether the respondents (n=431, Fall 2020; n=526, Fall 2019) are a representative sample that closely matches the characteristics of your population. If not, please address this selection bias in the discussion.
Unfortunately, we can’t directly assess how well our samples were representative of their respective populations, the following has been added in limitations to address this:
“Due to anonymous data collection and optional questions to protect participant identities, we cannot assess granular response rates by demographic characteristics. Future studies could be completed with a controlled sample matched with participant identifiers to know who in the sample is and isn’t responding, as this could impact findings.”
6 – Line 166-167. "Middle Eastern", while an important subcategory, is not a part of the NIH definition of underrepresented groups. If you would like to use the NIH guidelines, please remove this subcategory from the UR coding. Alternatively, please directly justify the coding of "Middle Eastern" as underrepresented. Please see revisions #13 and #14 for further discussion about NIH guidelines.
Thank you for pointing out the limitations of NIH definition, here and elsewhere – we have further explained the reasoning for inclusion of Middle Eastern and expanded the discussion of why this category was included. In addition, we adjusted the terminology to better reflect the categories included in our analyses to include identities that have been historically excluded. This category has been retitled accordingly to, “historically excluded (HE)” as reflected in science by race/ethnicity and gender (HE gender discussed elsewhere). Please also see other author responses for a summary; as well as expanded responses about marginalized identity, gender, intersectionality, Asian identity, and an expanded discussion of NIH definition along with limitations thereof.
The following has been added:
“Further, the stress experienced by Asian Americans as scapegoats of the pandemic and targets of anti-Asian violence may also affect the mental health of Asian American students within academia.” (Introduction)
“In the primary analysis, mental health data was analyzed by type of training program (MD vs. PhD), year (2019 vs. 2020), and historically excluded (HE) populations by race/ethnicity (HE-RE vs. NHE-RE) and by gender (HE-G women vs. NHE-G men). A post hoc analysis included the primary variables as wells as historically excluded by sexual orientation (HE-SO LGBQ+ vs. NHE-SO non-LGBQ+).” (Methods)
“in accordance with National Institutes of Health definitions of underrepresented in the biomedical, clinical, behavioral, and social sciences (NIH, 2020). Historically, Asian Americans have also faced exclusion from American culture as evidenced by Japanese Internment and the Chinese Exclusion Act. However, Asian Americans have been well-represented in the sciences and thus are included as NHE-RE for analysis. Additionally, Middle Eastern is not included in the US Census or NIH definitions as underrepresented; however, this identity group is included as HE-RE due to the marginalization especially over the past two decades in the United States following 9/11/2001.” (Methods-Participants)
7 – Please ensure that the in-text reported percentages and N values are easy to understand, as they are quite unclear in the current version. This is particularly the case in the "participants" section of the methods and figure legends, where it is unclear what year each number represents.
We have simplified the figures and legends in favor of an expanded unified description in the Methods, as we recognize that the prior version may be confusing. Previously, the chi-squared post hoc analysis relied on specific n and degrees of freedom for each test that impacted interpretation (no longer crucial for the current analyses). Especially given the updated modeling with interaction terms used to replace the previous chi-squared post hoc tests, the exact n per each subgroup is less important and instead the odds ratios and p-values are the primary focus. Accordingly, to reflect this change, Figure 1 has been simplified per the editors and reviewers’ suggestions; Figure 2 and Figure 3 (new Figure 3 added to visualize effects identified in the post hoc analysis) also now include percentages embedded in the figures rather than embedding these details in the legends.
Methodological and statistical issues:
8 – The data collected in 2019 and 2020 was combined for data analysis, suggesting that some participants may have participated in both years. Logistic regression requires the observations to be independent of each other: that is, the observations should not come from repeated measurements. This could bias/inflate the results – the larger number of repeated respondents, the higher chance to obtain biased results – and it therefore needs to be carefully justified and addressed. If you can identify repeated respondents, please report how many, and justify why you think you can include them in the analysis: in addition, please consider exploring whether your findings stay the same if you take out those repeated respondents, and/or use a repeated measures design to compare the difference in mental health between 2019 and 2020. If you are not able to identify repeated respondents, please discuss this limitation.
Due to data being collected anonymously, we cannot confirm if there were any repeated participants across the year timepoints; we recognize that this is a limitation, and have added the following to the discussion to acknowledge this:
“We recognize that if a large number of participants responded in both samples this could be problematic for assumptions of independence for use of parametric statistics and the Logistic Regression analysis used specifically, hence results should be interpreted with caution. Because we collected data anonymously to protect respondents’ privacy, we cannot assess to what extent there may have been respondents who participated in both years. If we did have identifiable data and were able to use a repeated-measures design, this would be preferable to reduce error variance. To the extent that significant findings were achieved even with the increased error variance inherent in a between-subjects design, these results likely had large enough effect sizes to be identified even given the loss of power from using a between-subjects design rather than the more sensitive within-subjects design that would be preferable.”
9 – The mental health outcomes are sensitive to recent events and affected by many factors/variables (e.g., variables related to the pandemic, years in the degree, disciplines, etc.): it is possible that the mental health disparities you report might be no longer statistically significant once these covariates are included in the analysis. Please either include these covariates in your logistic regression, or explain in the manuscript why they were not included.
We did not collect pandemic-specific data as we used the same annual survey questions from the previous year, future evaluations should ask and control for these variables. Limitations for being able to include years in training is discussed elsewhere (see additional author responses to year in training variable). We did not collet specialty or departmental affiliations to protect anonymity, to increase comfort with responding, and to maximize response rates. Furthermore, disciplinary clusters were deemed homogeneous enough to be considered in the two major categories of biomedical PhD training and medical MD training.
“Additional limitations included our lack of ability to control for other possible variables of interest such as pandemic-specific factors, years in training, and departmental affiliation or specialty area. Pandemic-specific questions were not asked because we used the same annual survey questions from the previous year to maintain comparable responses. Department and specialty information were not asked in order to protect anonymity, to increase comfort with responding, and to maximize response rates. Yet, populations were purposefully defined by reasonably homogenous training experiences into the two major clusters of interest: biomedical PhD training and MD training. Optional demographic questions were not completed for number of years in training for a large portion of the sample, limiting our ability to include this in the analysis. Future work should consider controlling for as many of these variables as possible.”
10 – The collected mental health measures could be treated as continuous variables, which could offer better variabilities for statistical modelling. Please clarify why you decided to simplify the scale (0 and 1) to run logistic regression analyses (binary outcome) rather than multiple regressions (continuous outcome). If you are not able to provide the reason, please make sure that both approaches (logistic regression and multiple regression) yield consistent findings.
The research question of interest was best captured by a bivariate designation of symptomatic versus asymptomatic (or problematic use versus non-problematic use). Hence, we approached the question from a bivariate logistic regression approach to answer the question accordingly. We felt this was the most appropriate model to answer the research question, and could be best interpreted to determined when respondents were functionally affected by their mental health; hence our decision to define it as such in the statistical modeling. Severity of symptoms at a more granular level, especially relying on self-report approaches rather than clinical diagnoses, posed several limitations that we felt made it a less appropriate approach to the data. Furthermore, for implications and policy purposes, we feel that the defined research question best illustrates the sweeping problem of mental health in graduate biomedical and medical education.
Additional analyses and discussion points pertaining to intersectionality approaches:
11 – Please consider conducting additional analyses to explore whether they were any differences across gender identity. The N values seem similar to the other populations you have chosen to compare, and this would significantly increase the impact of this study. Otherwise, please justify why this variable was not explored.
We agree that including gender as variable would add to the intersectional applicability of our model, and hence have added it as a control variable for all primary analyses.
We also decided that if evaluating the impact of gender were to be added to the model, we would be remiss to not also include sexual orientation status if we had a large enough sample size, as the intersectionality of gender and sexual identity can interact with race/ethnicity, trainee type, and year as well. However, we were also cautious about inadvertently reducing power to evaluate main effects beyond the primary research questions in order to ensure enough power to evaluate the primary intersectional identities (race/ethnicity, gender, and trainee type) by year. Hence, we added a post hoc analysis that accounted for both gender and LGBQ status using an intersectional approach.
We have added sections in the results and discussion describing the revised primary analysis (adding gender using a more sophisticated Logistic Regression model including interaction terms, conditional odds ratios, and marginal means to replace the more simplistic Chi-Squared comparisons previously displayed) as well as the post hoc model which includes LGBQ identity. Along with these substantive changes to the analyses, we have included justification and precedent for including both gender and sexual orientation based on previous studies. Transgender identity could not be included due to the small sample size, but should be included in future work and this limitation is also addressed in the manuscript.
Relatedly, to avoid reductions in power we also ran post hoc tests to further examine the impact of Asian social identities in a more granular way, and have reported the new results accordingly (using the model that also controls for gender).
12 – If feasible, please adopt an intersectionality approach, in particular by examining how gender AND race/ethnicity impact your findings. Otherwise, please justify why these analyses were not performed, and strengthen your discussion around intersectionality.
We have adopted an intersectional approach, with additional citations to justify this in the introduction as well as a deeper dive in the discussion. Thank you for this suggestion, we believe it has strengthened our approach and the applicability of the findings greatly.
13 – While Asians are included as well-represented according to NIH standards, the percentage of Asian-identifying individuals in the sample (at 16% and 9%) clearly demonstrates that they are not. This is discussed at the end, but please also include these comments in the Results section and strengthen the language. In addition, please consider comparing the experiences of Asian and White students, or, if you are concerned with anonymity/statistical power, please consider comparing WR vs. UR where "Asian" is moved from WR to UR, as this would allow the reader to understand if coding "Asian" as WR vs. UR makes a difference (this does not necessarily need to be in the main part of the paper). Alternatively, please justify why these analyses were not performed.
Thank you for this suggestion. We agree that a more granular investigation of the impacts on Asian participants is useful, despite having a small sample once dividing HE-RE into 3 classifications; hence have included a supplemental post hoc analysis as mentioned in other author responses which still allows us to address the questions while retaining power for the primary analysis. The following has been added:
“People who identified of Asian descent generally scored better than other NHE or HE groups, indicating fewer mental health challenges on all four outcome variables and the three suicidal ideation variables. However, conditional odds rations based on these models indicated some changes by year that may be associated with the negative psychosocial and environmental factors many Asian Americans experienced between 2019-2020. Accounting for the effect of race (3-level) while controlling for year, MD/PhD, and gender in 2020 compared with 2019, Asian participants showed greater mean depression scores (p<.03) and anxiety scores (p<.04); there was no change in either alcohol use (p=.07, though marginal) or drug use (p=.28). There were no significant changes in conditional probabilities for suicidal ideation of Asian participants during that time. Future directions should include examination of the intersectionality of these and other identity groups, and systemic barriers that each may encounter differentially. Follow-up studies should explore the impact of racism on Asian Americans and contrast Asian American experiences with White American experiences when reporting HE-RE data.”
14 – On that note: although discussed at the end, please provide a more nuanced discussion of race and ethnicity, and strengthen your stance. In particular, while it is understandable that you want to use NIH standards, please acknowledge more overtly that race is a social construct (so as to not reinforce the notion that these categories may be biological); and please discuss in more depth how the NIH categories may be lacking and not best represent a marginalized identity in science.
Thank you for these valuable suggestions, which we have leaned on heavily to reframe much of our discussion and additional analyses. We believe this has strengthened our findings and our ability to interpret implications more broadly. We have: (a) expanded our discussion of intersectionality; (b) added more nuanced analysis controlling for a wider range of identities (including the addition of gender to all of our primary models; c) included a post hoc analysis and discussion of Asian identity as well as sexual orientation); (d) re-envisioned the terminology used to Historically Excluded (HE) in science (HE-RE and HE-G); (e) we have expanded our discussion of limitations to the NIH definitions of WR/UR; and f) we have explicitly noted the social derivation of race.
The following has been added to the discussion (see NIH definition expanded discussion in other author responses):
“We recognize [both that race is a social construct], and that other social identity groups beyond race and ethnicity (Rothman, Gunturu, Korenis, 2020) may also experience inequitable impacts of COVID-19 and similar structural biases may negatively impact mental health for other reasons (Hunt, 2020). (Discussion)
“In fact, the NIH has recently expanded its definition of underrepresented in science to include women, people with disabilities, first generation college students, and those from disadvantaged backgrounds, including people who have experienced or are experiencing homelessness, foster care participation, recipients of free and reduced lunch, Pell grants, SNAP or WIC, and those who grew up in a low-income or rural areas (NIH, 2020; NIH, 2018, rescinded and replaced in 2019; NIH, 2019). This expanded definition is still flawed as some groups are still excluded from recognition and inclusion as societal norms and practices shift over time. For instance, people of middle eastern descent who have faced heightened discrimination, especially following 9/11/2001.” (Discussion)
NIH definition limitations are discussed in a number of other points in the response as well (please see also other author responses regardig Middle Eastern and Asian identities, gender, intersectionality, and NIH definition limitations).
Furthermore, particularly in recent American history, it is noteworthy that over the past 20 years many groups have been systematically marginalized during different periods of time. Future definitions of historically excluded groups may also want to consider the impact of current events with politics and their intersection with discrimination against specific social identities. We must acknowledge that science is not immune from such effects, which can drive out a talented, diverse pool of future scientists in training.
Strengthening certain claims
15 – Please provide evidence for the following statements:
a – Line 40 ("biomedical graduate programs are exposed to unique stressors by the nature of their training"): please consider moving up certain citations (e.g. Hazell et al., 2020 and Mackie and Bates 2019) to support this affirmation. Please also consider replacing the word "unique" as long hours, pressure to produce, and unsupportive mentors may not necessarily support a "uniquely" stressful situation.
b – Line 93 ("Trainees of color, especially people identifying as Black, Indigenous, and people of color (BIPOC), may also be affected by heightened concerns about individual, community, and family health."): While covid disparities are certainly real, and likely at play, please provide supporting evidence for this affirmation.
c – Line 340 ("We also speculate that being in a medical training program with obvious direct impact during a time when medical professionals were publicly celebrated had a positive effect on MD student mental health.") This discussion of MDs being "publicly celebrated" and "heroic" and able to connect their training to the crisis compared to PhD lacks evidence, particularly as we see protests outside of hospitals continue.
d – Line 343 ("Furthermore, medical students were able to continue some form of their training remotely, maintain some social contact and peer support networks through academic training, and avoid graduation delays.") Please provide citations for this statement, and clarify whether this is institution-specific.
e – Line 356 ("Biomedical PhD student training was severely curtailed in the 2020 spring months…"). Please clarify if this refers to specific measures at your institution.
f – Line 410 ("the mental health crisis in graduate biomedical education has only recently received considerable attention from the laboratory research community."): Please provide evidence for this statement.
Unique has been replaced as follows:
“Considering that students in medical school and in biomedical graduate programs are exposed to a multitude of stressors by the nature of their training including long hours, pressure to produce, and unsupportive mentors…”
B – We have reframed the terminology to center on Historically Excluded instead of BIPOC; nonetheless, we have also included an additional reference to support the extension of the COVID-19 impacts to disproportionately impact BIPOC individuals, communities, and family health.
We have also added the following reference, examining HE-RE working class inequities due to COVID-19:
Pathak, E. B., Menard, J. M., Garcia, R. B., and Salemi, J. L. (2021). Social Class, Race/Ethnicity, and COVID-19 Mortality Among Working Age Adults in the United States. medRxiv.
Feldman, J. M., and Bassett, M. T. (2021). Variation in COVID-19 Mortality in the US by Race and Ethnicity and Educational Attainment. JAMA network open, 4(11), e2135967-e2135967.
Limas, J.C. (2021). Adaptation to Overexpression of Cyclin E in Epithelial Cells. (Publication No. 2616907910) [Doctoral dissertation, University of North Carolina at Chapel Hill]. ProQuest Dissertations and Theses Global.
Limas, J. C., Corcoran, L. C., Baker, A. N., Cartaya, A. E., and Ayres, Z. J. (2022). The Impact of Research Culture on Mental Health and Diversity in STEM. Chemistry–A European Journal, e202102957.
“While our students themselves may be classified as associated with some lower risk groups for direct effects COVID due to their levels of education, BIPOC students disproportionately hail from working-class families and identify as first-generation college graduates. Hence, students historically excluded by race and ethnicity (HE-RE; e.g., those identifying as BIPOC) may experience disproportionate impact to their families, in that their families have been most at risk for mortality from COVID during 2020 within each social class (Pathak et al., 2021). Similarly, highest risk of age-adjusted mortality during COVID was identified for Hawaiian and Other Pacific Islander, American Indian or Alaska Native, and Latinx or Hispanic people (Black, Feldman and Bassett, 2021). An illustrative example includes a PhD sharing instances of her own experience as a Mexican-American woman PhD trainee during this time (Limas, 2021).”
C – We acknowledge the very real impact of anti-medical establishment influences as well, and have added the following to address this oversight: “Even so, this was not a ubiquitous experience, as simultaneously continued protests and divisiveness regarding vaccination were also pervasive across the country, which could ameliorate this effect (e.g., Bogel-Burroughs, 2020).”
Bogel-Burroughs, N. (2020). Antivaccination activists are growing force at virus protests. The New York Times. May, 2.
D and E – We have clarified these statements, and qualified them by specifying, “at our institution.”
F – The following has been added to clarify:
“Whereas medical schools have had mental health recommendations in place since 1992 (AAMC, 1992; enforced by Liaison Committee on Medical Education accreditation standards), biomedical PhD programs have had no such parallel policies regarding mental health provisions nationwide. Similarly, while there have been frequent calls for mental health research in higher education and there is already a robust body of literature decades old already in medical education (e.g., Slavin, 2016; a systematic review of medical education mental health evidence-based research included 195 relevant studies, Rotenstein et al., 2016) , evidence-based research on mental health research of PhDs has begun to emerge over the past five years (e.g., Levecque et al., 2017; Evans et al., 2018). Resources have been mobilized to evaluate and respond to the needs of medical students (e.g., 28 studies evaluating interventions, Wasson et al., 2016), which indeed still merit additional attention given high rates of depression, anxiety, and suicidality.”
The following additional references have also been added:
AAMC Executive Council (1992). Recommendations Regarding Health Services for Medical Students. Washington, DC: Association of American Medical Colleges
Available: https://www.aamc.org/professional-development/affinity-groups/gsa/health-services-recommendations
Wasson, L. T., Cusmano, A., Meli, L., Louh, I., Falzon, L., Hampsey, M., … and Davidson, K. W. (2016). Association between learning environment interventions and medical student well-being: a systematic review. Jama, 316(21), 2237-2252.
https://doi.org/10.7554/eLife.69960.sa2Article and author information
Author details
Funding
National Institute of General Medical Sciences (1R01GM140282-01)
- Rebekah L Layton
The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Acknowledgements
The authors thank the Odum Institute for Research in Social Science at UNC-Chapel Hill for its support, resources and consultations on statistical analyses. We thank Nathan Vanderford for valuable insights on earlier versions of this manuscript. Tables were generated from SAS Output, and figures were created using Numbers and BioRender.
Ethics
Human subjects: The study was reviewed and approved as Exempt by the UNC Institutional Review Board (#18-0112). Consent was obtained on the first question of the survey before continuing forward to respond to any additional questions. In accordance with IRB approval, the presentation of data will not include demographic information that could potentially lead to the identification of a student. Furthermore, to protect student anonymity, responses with fewer than ten individuals will not be shared. Accordingly, data sharing is limited to those variables directly relevant to the analyses conducted (e.g., underlying data) and composite categories (e.g., historically excluded by category vs. non-historically excluded by category, such as race/ethnicity, gender, or sexual orientation) are shared when applicable rather than granular demographic information to protect the identity of respondents.
Publication history
- Received:
- Accepted:
- Version of Record published:
Copyright
© 2022, Schad, Layton et al.
This article is distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use and redistribution provided that the original author and source are credited.
Metrics
-
- 2,213
- views
-
- 273
- downloads
-
- 19
- citations
Views, downloads and citations are aggregated across all versions of this paper published by eLife.
Citations by DOI
-
- 19
- citations for umbrella DOI https://doi.org/10.7554/eLife.69960







