Sleep regularity and mortality: a prospective analysis in the UK Biobank
Figures
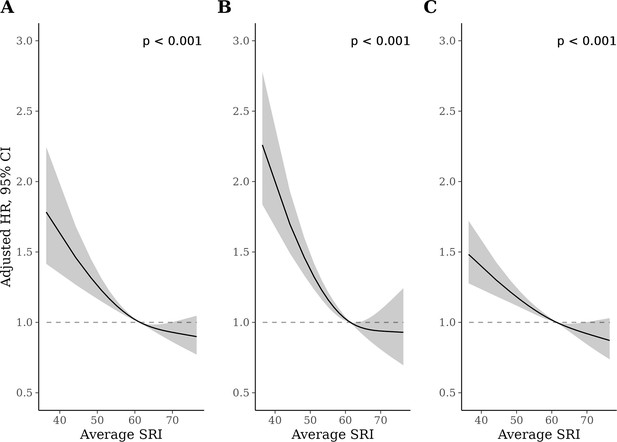
Adjusted hazard ratios (HRs) for all-cause (A), cardiovascular disease (CVD) (B), and cancer (C) mortality.
p-Values from global (2 degrees of freedom) test of spline term. HRs are relative to the median sleep regularity index (SRI) (SRI = 60). HRs for all-cause mortality, CVD mortality, and cancer mortality were estimated using Cox proportional hazards models, adjusted for age, Townsend deprivation index, sex, antidepressant, antipsychotic, and sedative medication, ethnicity, household income, education, smoking status (former, current, never), smoking pack years, shift work, retirement status, and sick or disabled (self-reported employment category). All continuous confounders and the SRI were modeled with restricted cubic splines (knots at 10th, 50th, and 90th percentiles) to allow for departures from linearity.

Cumulative incidence of all-cause mortality across sleep regularity index (SRI).
Standardized cumulative incidence of all-cause mortality for SRI at 41 (5th percentile), 61 (median), and 75 (95th percentile). Estimates from a discrete-time hazards models including an interaction between SRI and time (aggregated into 3-month intervals and modeled with a restricted cubic spline with knots at the 5th, 35th, 65th, and 95th percentiles) and primary model covariates. Confidence intervals were obtained by bootstrapping.
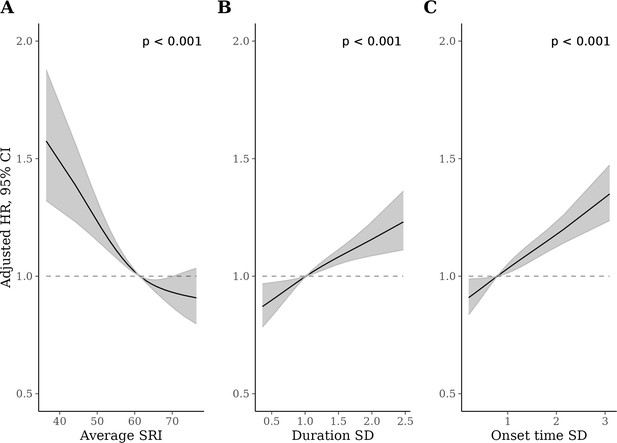
Adjusted hazard ratios (HRs) for all-cause mortality for the sleep regularity index (SRI) (A), sleep duration standard deviation (SD) (B), and sleep onset SD (C) measures.
p-Values from global (2 degrees of freedom) test of exposure spline term. HRs are relative to the median SRI (SRI = 60). HRs were estimated using Cox proportional hazards models, adjusted for age, Townsend deprivation index, sex, antidepressant, antipsychotic, and sedative medication, ethnicity, household income, education, smoking status (former, current, never), smoking pack years, shift work, retirement status, and sick or disabled (self-reported employment category). All continuous confounders and the sleep regularity metrics were modeled with restricted cubic splines (knots at 10th, 50th, and 90th percentiles) to allow for departures from linearity.
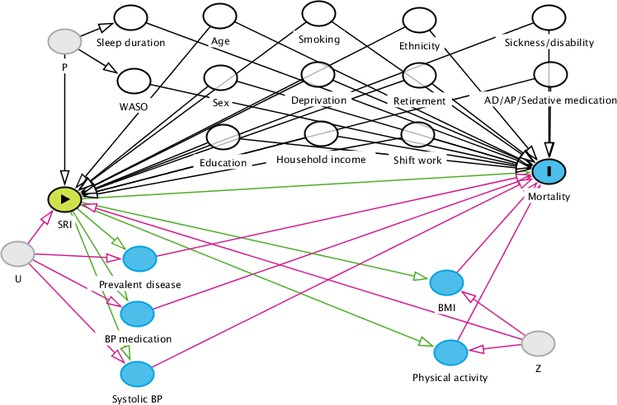
Directed acyclic graph for identification of adjustment variables.
The green node indicates the exposure variable (SRI), and the blue node (Mortality) is the outcome variable. Pale gray nodes indicate unobserved variables; white nodes indicate a variable which has been conditioned on (by regression adjustment or restriction). Paths in red are biasing paths. Arrows indicate the direction of causal effect between two nodes. P is an unobserved variable representing unmeasured causes of sleep habits (e.g., genetics). U is an unobserved variable representing unmeasured causes of disease and cardiovascular dysfunction (e.g., genetics, biological aging). Z is an unobserved variable representing unmeasured causes of health behaviors (e.g., personality factors, genetics). Green paths from SRI to Prevalent disease, BP medication, Systolic BP, BMI, and Physical activity and from these nodes to Mortality represent potential mediation of an SRI effect. Conversely, red paths indicate potential sources of confounding (e.g., a backdoor path from Mortality to Prevalent disease to SRI via U). Given the current evidence base, we are unable to determine whether and to what extent variables such as Prevalent disease act as mediators or confounders (via U) of the SRI-mortality association. AP = anti-psychotic; AD = antidepressant; BMI = body mass index; BP = blood pressure; CVD = cardiovascular disease; Deprivation = the Townsend deprivation index; SRI = sleep regularity index; WASO = wake after sleep onset.
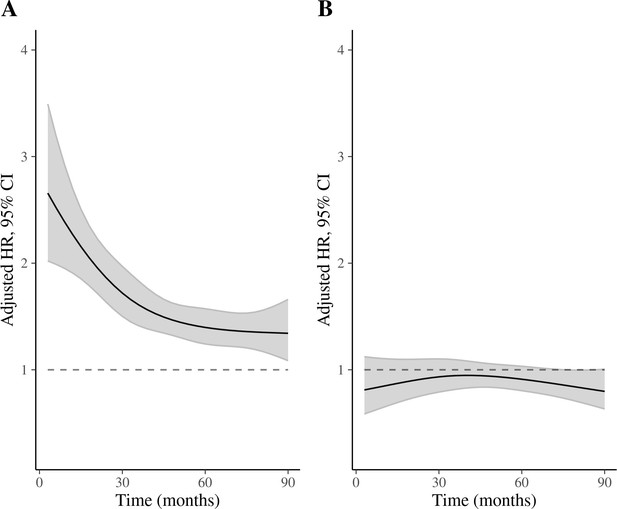
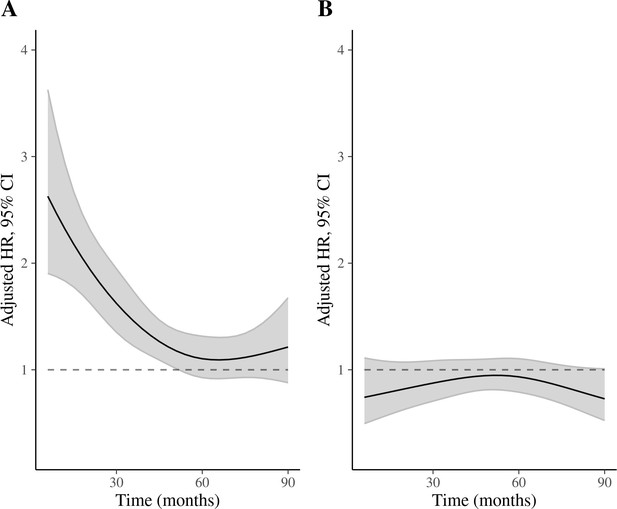
Time-varying hazard ratios (HRs) for 5th and 95th percentiles of sleep regularity index (SRI) (relative to median) for all-cause mortality.
(A) HRs for 5th percentile vs median SRI; (B) HRs for 95th percentile vs median SRI. Discrete-time hazards model including time (aggregated into 3-month intervals and modeled with a restricted cubic spline with knots at the 5th, 35th, 65th, and 95th percentiles), SRI, and an SRI by time interaction. Adjusted for age, Townsend deprivation index, sex, antidepressant, antipsychotic, and sedative medication, ethnicity, household income, education, smoking status (former, current, never), smoking pack years, shift work, retirement status, and sick or disabled (self-reported employment category). All continuous confounders and the SRI were modeled with restricted cubic splines (knots at 10th, 50th, and 90th percentiles) to allow for departures from linearity. There was strong evidence of an interaction between time and SRI (p [interaction]<0.001).
Time-varying hazard ratios (HRs) for 5th and 95th percentiles of sleep regularity index (SRI) (relative to median) for cancer mortality.
(A) Hazard ratios for 5th percentile vs median SRI; (B) HRs for 95th percentile vs median SRI. Discrete-time hazards model including time (aggregated into 3-month intervals and modeled with a restricted cubic spline with knots at the 5th, 35th, 65th, and 95th percentiles), SRI, and an SRI by time interaction. Adjusted for age, Townsend deprivation index, sex, antidepressant, antipsychotic, and sedative medication, ethnicity, household income, education, smoking status (former, current, never), smoking pack years, shift work, retirement status, and sick or disabled (self-reported employment category). All continuous confounders and the SRI were modeled with restricted cubic splines (knots at 10th, 50th, and 90th percentiles) to allow for departures from linearity. There was strong evidence of an interaction between time and SRI (p [interaction]<0.001).
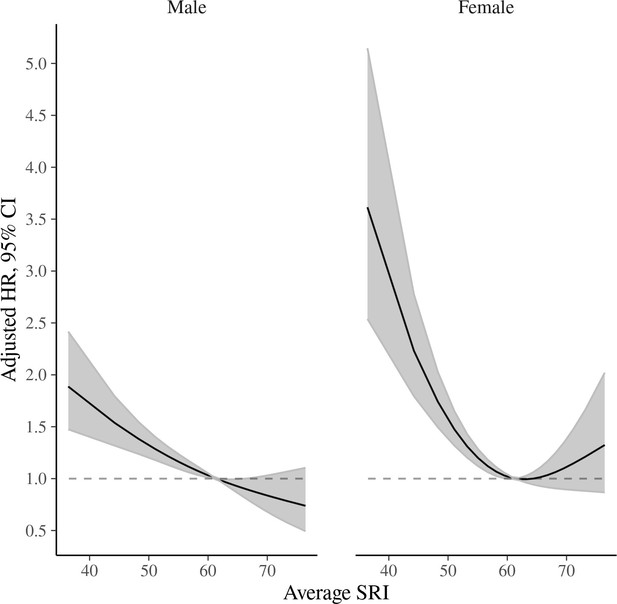
Sleep regularity index (SRI) and cardiovascular disease (CVD)-specific mortality by sex.
Adjusted for age, Townsend deprivation index, antidepressant, antipsychotic, and sedative medication, ethnicity, household income, education, smoking status (former, current, never), smoking pack years, shift work, retirement status, and sick or disabled (self-reported employment category). Hazard ratios are relative to the median SRI (SRI=60).

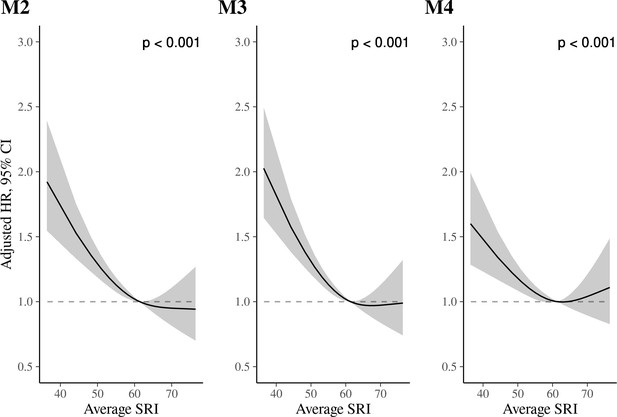
Sleep regularity index (SRI) and all-cause mortality in sensitivity analyses.
p-Values from global (2 degrees of freedom) test of spline term. Hazard ratios (HRs) are relative to the median SRI (SRI = 60). Model 2 (M2) adjustments: Adjusted for age, Townsend deprivation index, sex, antidepressant, antipsychotic, and sedative medication, ethnicity, household income, education, smoking status (former, current, never), smoking pack years, shift work, retirement status, and sick or disabled (self-reported employment category), average sleep time, and average wake after sleep onset time. M2 results: HRs, relative to the median SRI, were 1.42 (95% CI: 1.31, 1.55) and 0.90 (95% CI: 0.80, 1.00) for SRI at the 5th and 95th percentiles, respectively. Model 3 (M3) adjustments: Adjusted for age, Townsend deprivation index, sex, antidepressant, antipsychotic, and sedative medication, ethnicity, household income, education, smoking status (former, current, never), smoking pack years, shift work, retirement status, and sick or disabled (self-reported employment category), and history of diabetes, cancer, mental and behavioral disorder, neurological illness, and cardiovascular illness. M3 results: HRs, relative to the median SRI, were 1.46 (95% CI: 1.35, 1.58) and 0.93 (95% CI: 0.83, 1.03) for the 5th and 95th percentiles of SRI, respectively. Model 4 (M4) adjustments: Model 3 with additional adjustment for body mass index (BMI), moderate and vigorous physical activity, systolic blood pressure, and blood pressure medication. M4 results: HRs, relative to the median SRI, were 1.20 (95% CI: 1.11, 1.31) and 1.00 (95% CI: 0.90, 1.12) for the 5th and 95th percentiles, respectively.
Sleep regularity index (SRI) and cardiovascular disease (CVD) mortality in sensitivity analyses.
p-Values from global (2 degrees of freedom) test of spline term. Hazard ratios (HRs) are relative to the median SRI (SRI = 60). Model 2 (M2) adjustments: Adjusted for age, Townsend deprivation index, sex, antidepressant, antipsychotic, and sedative medication, ethnicity, household income, education, smoking status (former, current, never), smoking pack years, shift work, retirement status, and sick or disabled (self-reported employment category), average sleep time, and average wake after sleep onset time. M2 results: HRs were 1.66 (95% CI: 1.40, 1.96) and 0.95 (95% CI: 0.73, 1.22) for the 5th and 95th percentile vs. the median SRI, respectively. Model (M3) adjustments: Adjusted for age, Townsend deprivation index, sex, antidepressant, antipsychotic, and sedative medication, ethnicity, household income, education, smoking status (former, current, never), smoking pack years, shift work, retirement status, and sick or disabled (self-reported employment category), and history of diabetes, cancer, mental and behavioral disorder, neurological illness, and cardiovascular illness. M3 results: HRs were 1.73 (95% CI: 1.47, 2.02) and 0.99 (95% CI: 0.77, 1.26) for the 5th and 95th percentiles, respectively. Model 4 (M4) adjustments: Model 3 with additional adjustment for body mass index (BMI), moderate and vigorous physical activity, systolic blood pressure, and blood pressure medication. M4 results: HRs were somewhat attenuated: 1.43 (95% CI: 1.21, 1.69) and 1.09 (95% CI: 0.85, 1.40), for the 5th and 95th percentiles, respectively.

Sleep regularity index (SRI) and cancer mortality in sensitivity analyses.
p-Values from global (2 degrees of freedom) test of spline term. Hazard ratios (HRs) are relative to the median SRI (SRI = 60). Model 2 (M2) adjustments: Adjusted for age, Townsend deprivation index, sex, antidepressant, antipsychotic, and sedative medication, ethnicity, household income, education, smoking status (former, current, never), smoking pack years, shift work, retirement status, and sick or disabled (self-reported employment category), average sleep time, and average wake after sleep onset time. M2 results: HRs were 1.35 (95% CI: 1.20, 1.52) and 0.88 (95% CI: 0.76, 1.02) for the 5th and 95th percentile vs. the median SRI, respectively. Model 3 (M3) adjustments: Adjusted for age, Townsend deprivation index, sex, antidepressant, antipsychotic, and sedative medication, ethnicity, household income, education, smoking status (former, current, never), smoking pack years, shift work, retirement status, and sick or disabled (self-reported employment category), and history of diabetes, cancer, mental and behavioral disorder, neurological illness, and cardiovascular illness. M3 results: HRs were 1.33 (95% CI: 1.19, 1.49) and 0.90 (95% CI: 0.78, 1.04) for the 5th and 95th percentiles, respectively. Model 4 (M4) adjustments: Model 3 with additional adjustment for body mass index (BMI), moderate and vigorous physical activity, systolic blood pressure, and blood pressure medication. M4 results: HRs were 1.15 (95% CI: 1.02, 1.30) and 0.97 (95% CI: 0.84, 1.12) for the 5th and 95th percentiles, respectively.
Tables
Sample characteristics (n=88,975).
| SRI tertile | |||
|---|---|---|---|
| Characteristic | <56.8n=29,361 | 56.8–65.2n=29,361 | >65.2n=30,252 |
| Sex (male), n (%) | 16,429 (56%) | 12,747 (43%) | 9691 (32%) |
| Age (years) | 62.3 (7.8) | 61.8 (7.8) | 61.6 (7.9) |
| BMI | 27.8 (4.9) | 26.6 (4.3) | 25.8 (4.1) |
| Ethnicity, n (%) | |||
| Asian | 1199 (4.1%) | 1110 (3.8%) | 1114 (3.7%) |
| Black | 159 (0.5%) | 107 (0.4%) | 76 (0.3%) |
| Mixed race | 1024 (3.5%) | 831 (2.8%) | 658 (2.2%) |
| White | 26,621 (91%) | 27,070 (93%) | 28,210 (93%) |
| Other | 233 (0.8%) | 145 (0.5%) | 129 (0.4%) |
| Townsend deprivation index (score units) | –1.36 (3.01) | –1.79 (2.76) | –2.01 (2.63) |
| Household income* (thousands), n (%) | |||
| <18 | 4917 (19%) | 3601 (14%) | 3266 (12%) |
| 18–30 | 6665 (25%) | 6225 (24%) | 6450 (24%) |
| 31–50 | 7352 (28%) | 7741 (29%) | 7843 (29%) |
| 51–100 | 5888 (22%) | 6816 (26%) | 7280 (27%) |
| >100 | 1633 (6.2%) | 1994 (7.6%) | 2159 (8.0%) |
| Retired, n (%) | 9467 (32%) | 8984 (31%) | 9442 (31%) |
| Shift worker, n (%) | 1869 (6.4%) | 1146 (3.9%) | 912 (3.0%) |
| Smoking status, n (%) | |||
| Current | 2790 (9.5%) | 1863 (6.4%) | 1451 (4.8%) |
| Former | 10,956 (37%) | 10,587 (36%) | 10,367 (34%) |
| Never | 15,526 (53%) | 16,830 (57%) | 18,361 (61%) |
| Sedative medication, n (%) | 334 (1.1%) | 231 (0.8%) | 216 (0.7%) |
| Antidepressant medication, n (%) | 2217 (7.6%) | 1543 (5.3%) | 1385 (4.6%) |
| History of cancer, n (%) | 3941 (13%) | 3800 (13%) | 3897 (13%) |
| History of CVD, n (%) | 13,949 (48%) | 11,602 (40%) | 10,727 (35%) |
| History of diabetes, n (%) | 1976 (6.7%) | 1059 (3.6%) | 724 (2.4%) |
| History of neurological disease, n (%) | 3946 (13%) | 3380 (12%) | 3467 (11%) |
| History of mental/behavioral disorder, n (%) | 3521 (12%) | 2482 (8.5%) | 2184 (7.2%) |
| Average night time sleep duration (hours; actigraphy-derived) | 6.33 (0.97) | 6.59 (0.78) | 6.79 (0.66) |
| Average night time wake after sleep onset (hours; actigraphy-derived) | 0.86 (0.30) | 0.80 (0.26) | 0.70 (0.23) |
| Sleep duration SD, hours | 1.33 (0.64) | 1.11 (0.52) | 0.94 (0.48) |
| Sleep onset time SD, hours | 1.41 (1.12) | 0.96 (0.64) | 0.72 (0.51) |
| SRI, score units | 48.5 (7.3) | 61.2 (2.4) | 70.3 (3.7) |
-
Data are mean (SD), unless specified otherwise. *pounds. SRI = sleep regularity index; CVD = cardiovascular disease.
STROBE statement—checklist of items that should be included in reports of cohort studies.
| Item No | Recommendation | |
|---|---|---|
| Title and abstract | 1 | (a) Indicate the study’s design with a commonly used term in the title or the abstract (see title) |
| (b) Provide in the abstract an informative and balanced summary of what was done and what was found (see pg 2) | ||
| Introduction | ||
| Background/rationale | 2 | Explain the scientific background and rationale for the investigation being reported (pg 3) |
| Objectives | 3 | State-specific objectives, including any prespecified hypotheses (pg 3) |
| Methods | ||
| Study design | 4 | Present key elements of study design early in the paper (pg 3) |
| Setting | 5 | Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection (pg 3) |
| Participants | 6 | (a) Give the eligibility criteria, and the sources and methods of selection of participants. Describe methods of follow-up (pg 3–4) |
| (b) For matched studies, give matching criteria and number of exposed and unexposed NA | ||
| Variables | 7 | Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers. Give diagnostic criteria, if applicable (pg 4) |
| Data sources/measurement | 8* | For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group (pg 3–4) |
| Bias | 9 | Describe any efforts to address potential sources of bias (pg 5) |
| Study size | 10 | Explain how the study size was arrived at (pg 3 and appendix) |
| Quantitative variables | 11 | Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why (pg 5) |
| Statistical methods | 12 | (a) Describe all statistical methods, including those used to control for confounding (pg 4–5, Appendix 3—figure 1) |
| (b) Describe any methods used to examine subgroups and interactions NA | ||
| (c) Explain how missing data were addressed (pg 4–5) | ||
| (d) If applicable, explain how loss to follow-up was addressed | ||
| (e) Describe any sensitivity analyses (pg 5) | ||
| Results | ||
| Participants | 13* | (a) Report numbers of individuals at each stage of study—e.g., numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up, and analyzed (pg 3) |
| (b) Give reasons for non-participation at each stage | ||
| (c) Consider use of a flow diagram. Not considered necessary but can be created upon request | ||
| Descriptive data | 14* | (a) Give characteristics of study participants (e.g., demographic, clinical, social) and information on exposures and potential confounders (Table 1) |
| (b) Indicate number of participants with missing data for each variable of interest. Missing data were infrequent, as described in Methods | ||
| (c) Summarize follow-up time (e.g., average and total amount) (pg 5) | ||
| Outcome data | 15* | Report numbers of outcome events or summary measures over time (pg 5) |
| Main results | 16 | (a) Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (eg, 95% confidence interval). Make clear which confounders were adjusted for and why they were included (Figures and Appendix figures) |
| (b) Report category boundaries when continuous variables were categorized NA | ||
| (c) If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time period (Figure 2) | ||
| Other analyses | 17 | Report other analyses done—e.g., analyses of subgroups and interactions, and sensitivity analyses (pg 6) |
| Discussion | ||
| Key results | 18 | Summarize key results with reference to study objectives (pg 7) |
| Limitations | 19 | Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias (pg 8) |
| Interpretation | 20 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence (pg 8) |
| Generalizability | 21 | Discuss the generalizability (external validity) of the study results (pg 7–8) |
| Other information | ||
| Funding | 22 | Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based (pg 8) |
-
Note: An Explanation and Elaboration article discusses each checklist item and gives methodological background and published examples of transparent reporting. The STROBE checklist is best used in conjunction with this article (freely available on the Web sites of PLoS Medicine at http://www.plosmedicine.org/, Annals of Internal Medicine at http://www.annals.org/, and Epidemiology at http://www.epidem.com/). Information on the STROBE Initiative is available at http://www.strobe-statement.org.
-
*
Give information separately for exposed and unexposed groups.
Correlation between sleep regularity index and standard deviation-based regularity metrics.
| Regularity measure | Sleep regularity index | Sleep duration SD | Sleep onset SD |
|---|---|---|---|
| Sleep regularity index | 1 | –0.32 | –0.42 |
| Sleep duration SD | –0.32 | 1 | 0.55 |
| Sleep onset SD | –0.42 | 0.55 | 1 |





