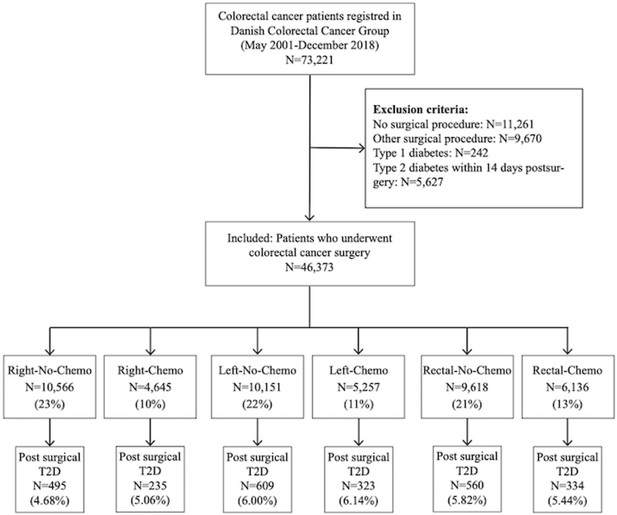
The impact of surgery and oncological treatment on risk of type 2 diabetes onset in patients with colorectal cancer: nationwide cohort study in Denmark
Figures
Tables
Baseline characteristics.
| Right-sided resection (Right)(N=15,211) | Left-sided resection (Left)(N=15,408) | Rectum resection (Rectal)(N=15,754) | ||||
|---|---|---|---|---|---|---|
| Right-No-Chemo | Right-Chemo | Left-No-Chemo | Left-Chemo | Rectal-No-Chemo | Rectal-Chemo | |
| All patients, n (%) | 10,566 (23%) | 4,645 (10%) | 10,151 (22%) | 5,257 (11%) | 9,618 (21%) | 6,136 (13%) |
| Sex, n (%) | ||||||
| Male | 4,338 (41%) | 2,126 (46%) | 5,450 (54%) | 2,834 (54%) | 5,743 (60%) | 3,745 (61%) |
| Female | 6,228 (59%) | 2,519 (54%) | 4,701 (46%) | 2,423 (46%) | 3,875 (40%) | 2,391 (39%) |
| Age, year, mean (SD) | 75.2 (10.0) | 66.9 (10.1) | 72.1 (10.7) | 64.8 (10.1) | 70.0 (10.7) | 64.3 (10.1) |
| BMI, mean (SD) | 25.0 (4.7) | 25.4 (4.7) | 25.7 (4.6) | 25.8 (4.5) | 25.6 (4.4) | 25.6 (4.4) |
| BMI subgroups | ||||||
| <18.5 | 482 (4.6%) | 114 (2.5%) | 287 (2.8%) | 97 (1.8%) | 225 (2.3%) | 143 (2.3%) |
| 18.5–24.9 | 4,183 (40%) | 1,907 (41%) | 3,638 (36%) | 2,004 (38%) | 3,693 (38%) | 2,570 (42%) |
| 25–29.9 | 2,671 (25%) | 1,347 (29%) | 2,945 (29%) | 1,641 (31%) | 3,021 (31%) | 1,993 (32%) |
| 30–34.9 | 814 (7.7%) | 404 (8.7%) | 961 (9%) | 545 (10%) | 889 (9.2%) | 611 (10%) |
| 35–39.9 | 194 (1.8%) | 90 (1.9%) | 214 (2.1%) | 135 (2.6%) | 171 (1.8%) | 132 (2.2%) |
| >40 | 62 (0.6%) | 34 (0.7%) | 69 (0.7%) | 39 (0.7%) | 60 (0.6%) | 30 (0.5%) |
| Missing | 2,160 (20%) | 749 (16%) | 2,037 (20%) | 796 (15%) | 1,559 (16%) | 657 (11%) |
| Smoking, n (%) | ||||||
| Never | 3,132 (30%) | 1,533 (33%) | 3,030 (30%) | 1,804 (34%) | 2,828 (29%) | 2,014 (33%) |
| Current | 1,671 (16%) | 791 (17%) | 1,486 (15%) | 821 (16%) | 1,679 (17%) | 1,305 (21%) |
| Former | 3,376 (32%) | 1,465 (32%) | 3,415 (34%) | 1,700 (32%) | 3,421 (36%) | 2,021 (33%) |
| Missing | 2,387 (22%) | 856 (18%) | 2,220 (21%) | 932 (18%) | 1,690 (18%) | 796 (13%) |
| Alcohol*, n (%) | ||||||
| 1–14 | 4,819 (46%) | 2,342 (51%) | 4,803 (47%) | 2,771 (53%) | 4,886 (51%) | 3,399 (55%) |
| 14–21 | 478 (5%) | 254 (5%) | 618 (6%) | 333 (6%) | 711 (7%) | 494 (8%) |
| >21 | 433 (4%) | 256 (6%) | 593 (6%) | 323 (6%) | 671 (7%) | 412 (7%) |
| None | 2,269 (21%) | 889 (19%) | 1,722 (17%) | 872 (17%) | 1,446 (15%) | 1,006 (16%) |
| Missing | 2,567 (24%) | 895 (19%) | 2,415 (24%) | 958 (18%) | 1,904 (20%) | 825 (13%) |
| ASA score†, n (%) | ||||||
| Healthy (=I) | 1,633 (15%) | 1,331 (29%) | 2,185 (22%) | 1,735 (33%) | 2,541 (26%) | 2,082 (34%) |
| Mild (=II) | 5,457 (52%) | 2,596 (56%) | 5,299 (51%) | 2,857 (54%) | 5,265 (55%) | 3,415 (56%) |
| Sick (=>II) | 3,160 (30%) | 613 (13%) | 2,442 (24%) | 548 (11%) | 1,653 (17%) | 557 (9%) |
| Missing | 316 (3%) | 105 (2%) | 295 (3%) | 117 (2%) | 159 (2%) | 82 (1%) |
| Screening detected tumor, n (%) | 770 (7%) | 299 (6%) | 1,077 (11%) | 457 (9%) | 664 (7%) | 394 (6%) |
| UICC stage‡, n (%) | ||||||
| I/II | 7,002 (66%) | 674 (15%) | 7,339 (72%) | 745 (14%) | 5,940 (62%) | 420 (7%) |
| III/IV | 3,330 (32%) | 3,504 (75%) | 2,506 (25%) | 3,989 (76%) | 2,246 (23%) | 2,471 (40%) |
| Unknown | 234 (2%) | 467 (10%) | 306 (3%) | 523 (10%) | 1,432 (15%) | 3,245 (53%) |
| Radiation, n (%) | - | - | - | - | 1,157 (12%) | 2,983 (49%) |
-
Chemo: chemotherapy.
-
*
Alcohol items per week.
-
†
The American Society of Anesthesiologist score: I: healthy, but with CRC; III: mild systemic disease without substantial functional limitations; >II: severe systemic disease, includes ASA stages III, IV, V, VI.
-
‡
UICC stage, Union of International Cancer Control; stage I: T1 or T2; stage II: T3 or T4; stage III: N1 or N2; stage IV: Disseminated disease at time of diagnosis.
Absolute incidence rates of type 2 diabetes (T2D) per 1000 person-years (95% CI) among colorectal cancer patients treated with different types of colorectal cancer surgery with and without chemotherapy.
| Right-sided resection (Right)(N=15,211) | Left-sided resection (Left)(N=15,408) | Rectum resection (Rectal)(N=15,754) | ||||
|---|---|---|---|---|---|---|
| Right-No-Chemo | Right-Chemo | Left-No-Chemo | Left-Chemo | Rectal-No-Chemo | Rectal-Chemo | |
| All patients, n | 10,566 | 4,645 | 10,151 | 5,257 | 9,618 | 6,136 |
| T2D development | ||||||
| Numbers | 495 | 235 | 609 | 323 | 560 | 334 |
| Mean time, year (SD) | 4.1 (3.4) | 4.1 (3.6) | 4.1 (3.5) | 4.4 (3.6) | 4.7 (3.7) | 4.3 (3.5) |
| Person-years | 48,039 | 22,317 | 53,935 | 29,301 | 58,448 | 33,422 |
| Incidence rates | 10.3 (9.4–11.2) | 10.5 (9.3–12.0) | 11.3 (10.4–12.2) | 11.0 (9.9–12.3) | 9.6 (8.8–10.4) | 10.0 (9.0–11.1) |
| Sex | ||||||
| Male | 13 (11–15) | 14 (12–16) | 14 (12–15) | 14 (12–16) | 11 (10–12) | 12 (11–14) |
| Female | 9 (8-10) | 8 (7-10) | 9 (8-10) | 8 (7-10) | 8 (7-9) | 7 (6-8) |
| Age | ||||||
| <50 | 3 (1-8) | 6 (3-11) | 7 (5-12) | 8 (5-12) | 5 (3-8) | 6 (4-10) |
| 50–64.9 | 12 (10–14) | 13 (11–16) | 11 (9–12) | 10 (8–12) | 10 (8–12) | 10 (9–12) |
| 65–74.9 | 12 (11–14) | 11 (9–14) | 12 (11–14) | 14 (12–17) | 14 (12–17) | 11 (10–13) |
| ≥75 | 9 (8-10) | 6 (4-9) | 11 (10–13) | 8 (6-12) | 8 (6-12) | 8 (5-11) |
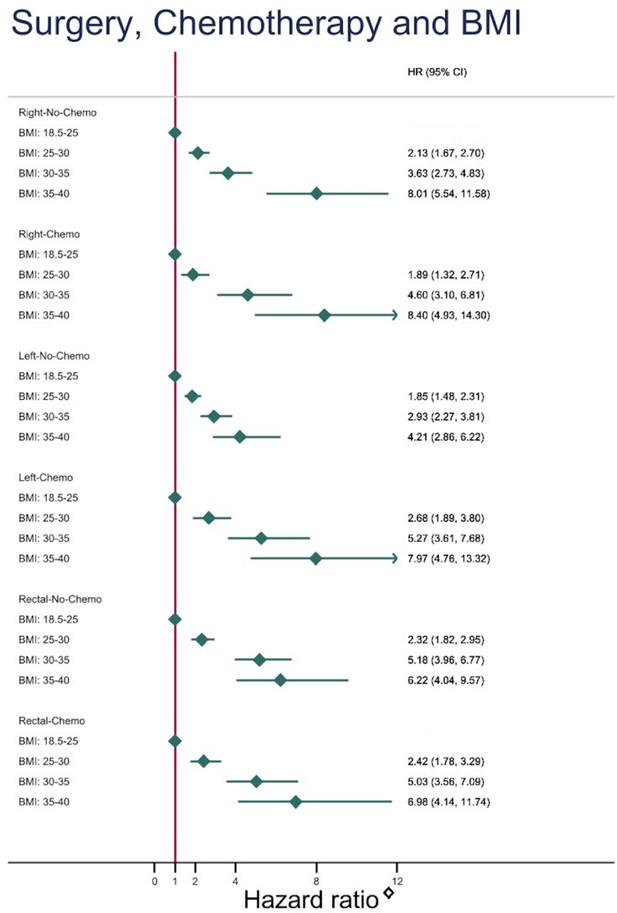
| BMI subgroups | ||||||
| 18.5–24.9 | 6 (5-7) | 5 (4-7) | 6 (5-8) | 4 (3-5) | 4 (4-5) | 4 (3-6) |
| 25–29.9 | 13 (11–16) | 11 (9–14) | 13 (11–15) | 12 (10–15) | 11 (9–12) | 12 (10–14) |
| 30–34.9 | 23 (18–28) | 30 (23–40) | 21 (17–25) | 24 (19–30) | 25 (21–30) | 24 (19–30) |
| 35–39.9 | 51 (38–70) | 53 (34–84) | 32 (23–45) | 34 (23–52) | 30 (21–44) | 31 (20–48) |
| Missing | 7 (6-9) | 9 (6-12) | 11 (9–12) | 12 (10–16) | 9 (8-12) | 10 (8–14) |
| Smoking | ||||||
| Never | 9 (8-11) | 11 (9–14) | 9 (8-11) | 8 (7-10) | 8 (7-10) | 9 (7-11) |
| Current | 13 (10–15) | 9 (7-13) | 11 (9–14) | 12 (10–16) | 10 (8–12) | 10 (7–12) |
| Former | 11 (10–13) | 12 (10–15) | 13 (11–15) | 13 (11–15) | 11 (9–12) | 11 (9–13) |
| Missing | 8 (7-10) | 9 (6-12) | 11 (10–14) | 12 (9–15) | 9 (8-11) | 11 (8–14) |
| Alcohol** | ||||||
| 1–14 | 11 (9–12) | 10 (8–12) | 10 (9–12) | 10 (9–12) | 9 (8-10) | 10 (8–11) |
| 14–21 | 9 (6-14) | 7 (3-14) | 9 (6-13) | 10 (7–16) | 8 (6-11) | 9 (6-14) |
| >21 | 10 (7–16) | 16 (11–25) | 14 (11–19) | 12 (8–18) | 11 (9–15) | 13 (9–18) |
| None | 12 (10–14) | 14 (10–18) | 13 (11–16) | 12 (9–16) | 13 (11–15) | 10 (7–13) |
| Missing | 9 (7-10) | 10 (7–13) | 12 (10–14) | 12 (10–16) | 10 (9–10) | 10 (8–13) |
| ASA score†† | ||||||
| Healthy (=I) | 7 (6-9) | 5 (3-7) | 7 (6-9) | 7 (5-9) | 5 (4-6) | 6 (4-7) |
| Mild (=II) | 10 (9–12) | 12 (11–15) | 12 (11–13) | 13 (11–15) | 11 (10–12) | 13 (11–14) |
| Sick (=>II) | 14 (12–17) | 17 (13–24) | 17 (12–17) | 18 (14–25) | 15 (12–18) | 12 (8–17) |
| Missing | 6 (3-11) | 15 (7–31) | 13 (8–20) | 11 (5–23) | 9 (5-17) | 10 (4–25) |
| Radiation | ||||||
| Yes | - | - | - | - | 11 (9–13) | 11 (9–13) |
| No | - | - | - | - | 9 (9-10) | 10 (9–12) |
-
Chemo: chemotherapy.
-
*
Alcohol items per week.
-
†
The American Society of Anesthesiologist score: I: healthy, but with CRC; III: mild systemic disease without substantial functional limitations; >II: severe systemic disease, includes ASA stages III, IV, V, VI.
Risk of developing type 2 diabetes after different types of colorectal cancer surgery with and without oncological treatment, unadjusted and adjusted analysis.
| Unadjusted | Model 1 | Model 2(a/b) | ||||
|---|---|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Surgery and chemotherapy | ||||||
| Right-No-Chemo | ref | |||||
| Right-Chemo | 1.02 (0.87;1.19) | 0.799 | 0.99 (0.83;1.17) | 0.880 | 1.01 (0.85;1.20)a | 0.884 |
| Left-No-Chemo | 1.10 (0.98;1.24) | 0.112 | 0.92 (0.81;1.05) | 0.228 | 0.94 (0.82;1.07)a | 0.333 |
| Left-Chemo | 1.07 (0.93;1.23) | 0.339 | 0.93 (0.79;1.09) | 0.366 | 0.97 (0.83;1.14)a | 0.708 |
| Rectal-No-Chemo | 0.94 (0.83;1.06) | 0.317 | 0.82 (0.72;0.94) | 0.004 | 0.86 (0.75;0.98)a | 0.028 |
| Rectal-Chemo | 0.96 (0.84;1.11) | 0.610 | 0.84 (0.72;0.99) | 0.031 | 0.89 (0.76;1.03)a | 0.126 |
| Surgery and radiation therapy | ||||||
| Rectal-No-Radiation | ref | |||||
| Rectal-Radiation | 1.07 (0.93;1.24) | 0.336 | 0.98 (0.85;1.13) | 0.804 | 0.97 (0.84;1.12)b | 0.691 |
| Surgery | ||||||
| All Colon | ref | |||||
| All Rectal | 0.90 (0.83;0.98) | 0.013 | 0.87 (0.79;0.95) | 0.002 | 0.89 (0.82;0.98)b | 0.015 |
Additional files
-
Supplementary file 1
Risk of developing T2D after different types of colorectal cancer surgery with and without chemotherapy – adjusted for cancer stage, Model 1 and Model 2.
- https://cdn.elifesciences.org/articles/89354/elife-89354-supp1-v1.pdf
-
MDAR checklist
- https://cdn.elifesciences.org/articles/89354/elife-89354-mdarchecklist1-v1.docx