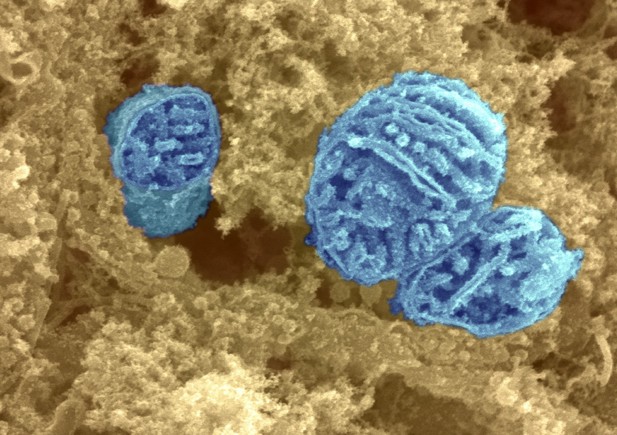
Three mitochondria (blue) in the cytoplasm (orange). Image credit: Dr David Furness (CC BY-NC 4.0)
Mitochondria are often described as the power plants of cells because they generate most of the energy that a cell needs to survive. But one in every 5,000 children is born with a mutation that leads to faulty mitochondria, which generate less energy than their healthy counterparts. This is particularly problematic for tissues with high energy demands, such as the brain and muscles. Children with such mutations are said to have mitochondrial disease, and one of the most common and severe forms is Leigh syndrome.
Children with Leigh syndrome suffer from epilepsy, and have difficulties with movement and breathing. There is no treatment for Leigh syndrome, and most of those affected will die in childhood. The brains of children with Leigh syndrome show a characteristic pattern of damage and inflammation, symmetrical across both hemispheres, with two areas of the brain affected the most. First, the brainstem, which connects the brain with the spinal cord and is responsible for many vital functions such as breathing, maintaining the heart rate or swallowing. Secondly, a group of neurons deep within the brain called the basal ganglia, which has a role in voluntary movement.
But although all of a patient’s neurons carry the mutation responsible for their Leigh syndrome, not every neuron is harmed by it. Knowing which neurons are affected, and why, could help develop treatments. Bolea, Gella, Sanz et al. therefore introduced the same Leigh syndrome mutation into different groups of neurons in three groups of mice. The first group had the mutation in the neurons that activate other cells, called glutamatergic or 'go' neurons. The second group had the mutation in the neurons that inhibit other cells, known as GABAergic, or 'stop', neurons. The third had the mutation in cholinergic neurons, which carry information from the brain to the organs.
Examining the mice revealed that having faulty mitochondria in GABAergic neurons from the basal ganglia and in glutamatergic neurons of the brainstem, but not in cholinergic neurons, leads to the symptoms of Leigh syndrome. The fault in the GABAergic neurons causes the epilepsy associated with the syndrome, while faulty mitochondria in the glutamatergic neurons give rise to the observed impairments in movement and breathing. This work could help researchers identify the cellular mechanisms that make neurons more or less resistant to the effects of faulty mitochondria. This in turn will provide a stepping stone to developing new treatments, which can then be tested on the mice developed for these experiments.




