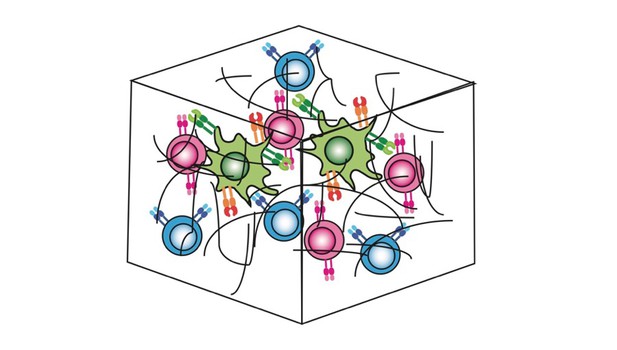
Schematic showing different types of T-cells incorporated into a three-dimensional gel matrix where they can move and interact. Image credit: Enas Abu-Shah (CC BY 4.0)
The human immune system protects the body from infection or cancer by detecting foreign and abnormal elements, known as antigens, and initiating a response to clear them. It relies on a type of white blood cell called a T-cell to distinguish which substances are the body’s own, and which are infectious. Each T-cell is designed to attack a specific antigen, which they recognise using a unique 'T-cell receptor'. During an infection, immune cells called 'antigen presenting cells' hold out antigens for the T-cells to look at. Only when an antigen matches the T-cell's receptor can the T-cell get activated and trigger an immune response.
There are still gaps in our understanding about how human T-cells interact with antigen presenting cells. Since only a small number of T-cells in the human blood have the same receptor, it is difficult to collect the large number of identical T-cells needed to study this interaction. In addition, it is impractical to image how these interactions occur in a living human body.
Now, Abu-Shah et al. have developed a new system that engineers human T-cells to have the same specific receptor. T-cells collected from human blood received the genetic information for identical receptors via a technique called electroporation. This involves mixing the cells with a single-strand copy of the receptor gene and then applying electric pulses to make the cell membranes leaky so the code for the receptor can get inside the cells.
To study the interaction between these genetically engineered T-cells and antigen presenting cells, Abu-Shah et al. created a three-dimensional system that mimics the environment T-cells normally experience inside the body. T-cells cultured using this system behaved similarly to immune cells in the human body, and displayed the characteristics needed to trigger an immune response.
With this new system, researchers could recreate other aspects of the human immune response outside of the body, incorporating different types of immune cells and different genetic modifications. Not only could this improve our understanding of the human immune system, it could also be used as a way to screen specific drugs during pre-clinical studies.




