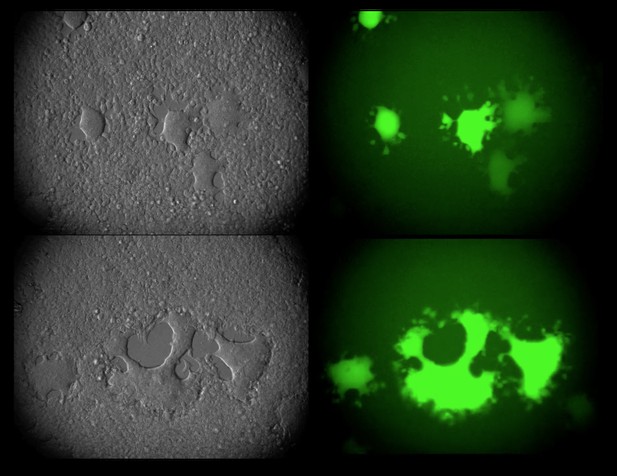
RhIV virus replicating in the cells of mice. On the left the cells can be seen in grey, and on the right the virus can be seen in green. Image credit: Rachel Liberatore and Emily Mastrocola (CC BY 4.0)
One of the main obstacles to developing a vaccine against HIV-1 is teaching the immune system to recognize the envelope proteins on the surface of the virus, which are also found on infected cells. Envelope proteins allow HIV-1 to attach to and infect a type of human immune cell known as a T-cell, by interacting with proteins on its membrane called CD4 and CCR5.
Antibodies are proteins produced by the immune system that can stop HIV-1 from spreading. They can recognize and attach to envelope proteins, thus tagging infected cells so the immune system can attack them, and ‘neutralizing’ viral particles to prevent them from infecting more cells. To make a vaccine against HIV-1, scientists need to teach the immune system how to make neutralizing antibodies. Unfortunately, HIV-1 only replicates in humans and chimpanzees, making it difficult to study how these antibodies are generated.
Now, Liberatore et al. have developed a hybrid virus that recreates key features of HIV-1 infection in mice. The interior of these viruses is made up of components from a rhabdovirus, which replicates well in mice, with envelope proteins from HIV-1 incorporated into the viruses’ exterior. Therefore, despite having different replication machinery, these hybrid viruses – nicknamed ‘RhIV’ – are able to infect the cells of mice using the same attachment mechanism as HIV-1.
Next, Liberatore et al. genetically modified mice to produce human CD4 and CCR5 proteins, so RhIV could attach to their T-cells and get inside. The virus rapidly killed the cells it infected, similar to early HIV-1 infection in humans. But, unlike HIV-1 infection in humans, the mice were able to get rid of the virus within a couple of weeks. When the mice were exposed to RhIV a second time, they were partially protected against re-infection. This ‘vaccine effect’ was even stronger if the mice were exposed a third time, making them almost immune to the virus. However, the effect could not be attributed exclusively to antibodies, since mice unable to make antibodies still gained some immune protection after infection with RhIV.
The results showed that antibodies produced by the infected mice could recognize HIV-1 envelope proteins, but were unable to neutralize viral particles. Nevertheless, transferring antibodies from infected mice after recovery into healthy mice that had never been exposed to the virus partially protected the healthy mice from infection.
This new model system for HIV-1 infection should make it easier to test new types of vaccines in a context where the vaccinated animal can be challenged with RhIV. Additionally, the ability to genetically engineer both the virus and the mouse host – for example by making mice that produce human antibodies – allows further studies into the development of antibodies that recognize the HIV-1 envelope.




