Peer review process
Revised: This Reviewed Preprint has been revised by the authors in response to the previous round of peer review; the eLife assessment and the public reviews have been updated where necessary by the editors and peer reviewers.
Read more about eLife’s peer review process.Editors
- Reviewing EditorIlse DaehnIcahn School of Medicine at Mount Sinai, New York, United States of America
- Senior EditorDavid RonUniversity of Cambridge, Cambridge, United Kingdom
Reviewer #1 (Public review):
Summary:
The authors used an in vitro microfluidic system where HUVECs are exposed to high, low or physiologic (normal) shear stress to demonstrate that both high and low shear stress for 24 hours resulted in decreased KLF6 expression, decreased lipid peroxidation and increased cell death which was reversible upon treatment with Fer-1, the ferroptosis inhibitor. RNA sequencing (LSS vs normal SS) revealed decreased steroid synthesis and UPR signaling in low shear stress conditions, which they confirmed by showing reduced expression of proteins that mitigate ER stress under both LSS and HSS. Decreased KLF6 expression after exposure to HSS/LSS was associated with decreased expression of regulators of ER stress (PERK, BiP, MVD) which was restored with KLF6 overexpression. Overexpression of KLF6 also restored SLC7A11 expression, Coq10 and reduced c11 bodipy oxidation state- all markers of lipid peroxidation and ferroptosis. The authors then used vascular smooth muscle cells (atherosclerotic model) with HUVECs and monocytes to show that KLF6 overexpression reduces the adhesion of monocytes and lipid accumulation in conditions of low shear stress.
Strengths:
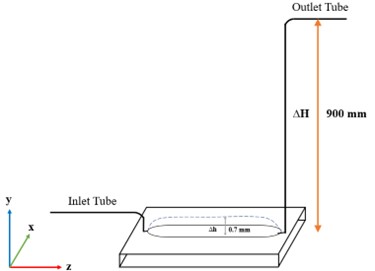
(1) The use of a microfluidic device used to simulate shear stress while keeping the pressure constant when varying shear stress applied is improved and more physiologic compared to traditional cone and shearing devices. Similarly, the utilization of both low and high shear stress in most experiments is a strength.
(2) This study provides a link between disturbed shear stress and ferroptosis, which is novel, and fits nicely with existing knowledge that endothelial cell ferroptosis promote atherosclerosis. This concept was also recently reported Sept 2025 when a publication also demonstrated that LSS trigger ferroptosis in vascular endothelial cells (PMID: 40939914), which partly validates these findings.
Weaknesses:
(1) While HUVECs are commonly used in endothelial in vitro studies, it would be preferable to confirm the findings using an arterial cell line such as human coronary artery cells when studying mechanisms of early atherosclerosis. Furthermore, physiologic arterial shear stress is higher than venous shear stress, and different vascular beds have varying responses to altered shear stress and as such, the up and downregulated pathways in HUVECs should be confirmed in an arterial system.
(2) The authors provide convincing evidence of disturbances in shear stress inducing endothelial ferroptosis with assays for impaired lipid peroxidation and increased cell death that was reversed with a ferroptosis inhibitor. However more detailed characterization of ferroptosis with iron accumulation assays, as well as evaluating GPX4 activity as a consequence of the impaired mevalonate pathway, and testing for concomitant apoptosis in addition to ferroptosis would add to the data.
(3) The authors state that KLF2 and KLF4 are not amongst the differentially expressed genes downregulated by reduced shear stress, which is contrary to previous data, where both KLF2 and KLF4 are well studied to be upregulated by physiologic laminar shear stress. While this might be due to the added pressure in their microfluidic system, it also might be due to changes in gene expression over time. In this case, a time course experiment would be needed. It is possible that KLF2, KLF4 and KLF6 are all reduced in low (and high) shear stress and cooperatively regulate the endothelial cell phenotype. Both KLF2 and KLF4 have been shown to be protective against atherosclerosis.
Comments on revisions:
The authors have failed to respond to all the preceding critiques with supporting experimental data. Recommend a reassessment of the initial critiques.