Peer review process
Revised: This Reviewed Preprint has been revised by the authors in response to the previous round of peer review; the eLife assessment and the public reviews have been updated where necessary by the editors and peer reviewers.
Read more about eLife’s peer review process.Editors
- Reviewing EditorYongliang YangShanghai University of Medicine and Health Sciences, Shanghai, China
- Senior EditorCaigang LiuShengjing Hospital of China Medical University, Shenyang, China
Reviewer #1 (Public Review):
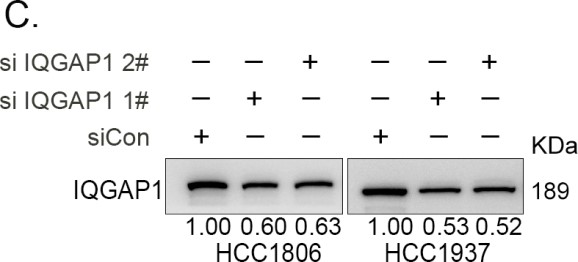
In this study, Fang H et al. describe a potential pathway, ITGB4-TNFAIP2-IQGAP1-Rac1, that may involve in the drug resistance in triple negative breast cancer (TNBC). Mechanistically, it was demonstrated that TNFAIP2 bind with IQGAP1 and ITGB4 activating Rac1 and the following drug resistance. The present study focused on breast cancer cell lines with supporting data from mouse model and patient breast cancer tissues. The study is interesting. The experiments were well controlled and carefully carried out. The conclusion is supported by strong evidence provided in the manuscript. The authors may want to discuss the link between ITGB4 and Rac 1, between IQGAP1 and Rac1, and between TNFAIP2 and Rac1 as compared with the current results obtained. This is important considering some recent publications in this area (Cancer Sci 2021, J Biol Chem 2008, Cancer Res 2023). In addition, some key points need to be addressed in order to support their conclusion in full.
Reviewer #2 (Public Review):
Breast cancer is the most common malignant tumor in women. One of subtypes in breast cancer is so called triple-negative breast cancer (TNBC), which represents the most difficult subtype to treat and cure in the clinic. Chemotherapy drugs including epirubicin and cisplatin are widely used for TNBC treatment. However, drug resistance remains as a challenge in the clinic. The authors uncovered a molecular pathway involved in chemotherapy drug resistance, and molecular players in this pathway represent as potential drug targets to overcome drug resistance. The experiments are well designed and the conclusions drawn mostly were supported by the data. The findings have potential to be translated into the clinic.
Reviewer #3 (Public Review):
A summary of what the authors were trying to achieve:
- TNFAIP2 promotes TNBC drug resistance and DNA damage repair.
- Mechanistically, TNFAIP2 interacts with IQGAP1 and Integrin β4 to mediate RAC1 activation and thus promotes TNBC drug resistance.
- Clinically, TNFAIP2 expression levels positively correlated with ITGB4 in TNBC tissues.
- ITGB4 and TNFAIP2 might serve as promising therapeutic targets for TNBC.
-An account of the major strengths and weaknesses of the methods and results.
The authors performed numerous rescue experiments in vitro to confirm the relationship among ITGB4, TNFAIP2, IQGAP1 and Rac1. However, clinical relevance is somehow limited. Additional experiments are needed to demonstrate the above conclusions in clinical samples.
-An appraisal of whether the authors achieved their aims, and whether the results support their conclusions.
To most extent, the authors achieved their aims, and the results demonstrate their conclusions "TNFAIP2 interacts with IQGAP1 and ITGB4. ITGB4 promotes TNBC drug resistance via the TNFAIP2/IQGAP1/RAC1 axis by promoting DNA damage repair".
-A discussion of the likely impact of the work on the field, and the utility of the methods and data to the community.
Drug resistance is always a challenge for TNBC treatment. This paper found that TNFAIP2 interacts with IQGAP1 and ITGB4 to activate Rac1, thus conferring DNA chemo-resistance to TNBC cells. In addition, positive correlation between the expression of TNFAIP2 and ITGB4 in TNBC tissues were presented. This paper suggests that the ITGB4/TNFAIP2/IQGAP1/Rac1 axis provides potential therapeutic targets to overcome chemo-resistance (DNA damage drugs) in fighting with TNBC.
Additional context to help readers interpret or understand the significance of the work:
This work reported a new mechanism related to TNBC chemo-resistance, which mainly depends on ordered interactions among ITGB4/TNFAIP2/IQGAP1/Rac1 and the following activation of pathways. Thus micro-peptide targeting technique, which is widely used to develop targeted drugs for protein-protein interactions, could show extraordinary potentials and application significance.
At present, cell penetrating peptide, a type of micro-peptide targeting technique, makes functional micro-peptides more stable by cross-linking some amino acid side chains. In recent years, it has been found that binding peptides can not only stabilize peptides, make them easier to enter cells, but also not easy to be hydrolyzed by proteases. At the same time, they have high affinity for targets and can target protein interactions, thus becoming a new way to develop protein interaction targeting inhibitors. To make it easier to enter cells, cell-penetrating peptides can be used in combination, such as HIV TAT. Cell-penetrating peptides can carry a variety of biologically active substances into the cell, is a good targeting drug carrier, with low toxicity, not limited by cell type, into the cell speed and high transduction efficiency. Based on the mechanism reported here, researchers can explore new micro-peptides targeting the interactions between ITGB4 and TNFAIP2 or TNFAIP2 and IQGAP1 to enhance the sensitivity of TNBC cells to drugs by cell-penetrating peptide technology.