Peer review process
Revised: This Reviewed Preprint has been revised by the authors in response to the previous round of peer review; the eLife assessment and the public reviews have been updated where necessary by the editors and peer reviewers.
Read more about eLife’s peer review process.Editors
- Reviewing EditorDaniel HenrionUniversité d'Angers, Angers, France
- Senior EditorMatthias BartonUniversity of Zurich, Zurich, Switzerland
Reviewer #1 (Public review):
Summary:
Assessment of cardiac LEC transcriptomes post-MI may yield new targets to improve lymphatic function. scRNAseq is a valid approach as cardiac LECs are rare compared to blood vessel endothelial cells.
Strengths:
Extensive bioinformatics approaches employed by the group
Weaknesses:
Too few cells included in scRNAseq data set and the spatial transcriptomics data that was exploited has little relevance, or rather specificity, for cardiac lymphatics. This study seems more a collection of preliminary transcriptomic data than a true scientific report to help advance the field.
Comments on revisions:
Thank you for the revision that helps clarify some outstanding questions.
(1) I still have questions relating to the relevance of the spatial maps generated and shown in fig 3C. They are supposedly generated using a 'molecular finger print' specific to each sub-cluster of LECs. However, given that at early stages postMI most populations are exceedingly rare in your analyses, could you please explain or comment on the relevance of the spatial maps?
(2) Fig 3 s1 would indicate that the population CaII is the majoritarian one in healthy hearts, while quantifications in Fig 3A show that rather the LEC Co subpopulation is majoritarian. Further, in mouse hearts histological analyses have demonstrated that cardiac lymphatics are restricted to the outer layers of the heart. This is not seen in your spatial maps. This seems to be the case only for the LEc Co population in healthy hearts, but not for other subpopulation signatures. Please explain.
(3) Further, the population of CaI, with 1 cell analysed in d3, but appears very prevalent in the spatial maps at d3. Please explain.
(4) In your list of 12 genes used as matrix anchors to identify LEC subpopulations in your screens, it is not apparent how LEC CaI, II and III differ so much as to allow selective detection of subpopulations. This similitude of profiles is supported by Fig 2F, and further explanations are needed to explain how the spatial maps of LEC ca subpopulations appear as distinct as shown in fig 3 S1 and Fig 3C.
Reviewer #2 (Public review):
Summary:
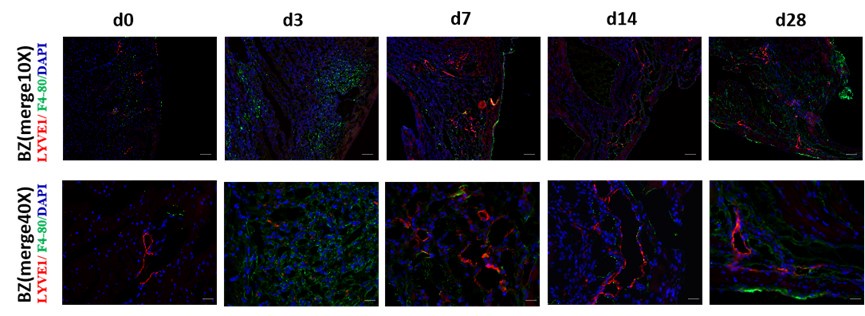
This study integrated single-cell sequencing and spatial transcriptome data from mouse heart tissue at different time points post-MI. They identified four transcriptionally distinct subtypes of lymphatic endothelial cells and localized them in space. They observed that LECs subgroups are localized in different zones of infarcted heart with functions. Specifically, they demonstrated that LEC ca III may be involved in directly regulating myocardial injuries in the infarcted zone concerning metabolic stress, while LEC ca II may be related to the rapid immune inflammatory responses of the border zone in the early stage of MI. LEC ca I and LEC collection mainly participate in regulating myocardial tissue edema resolution in the middle and late stages post-MI. Finally, cell trajectory and Cell-Chat analyses further identified that LECs may regulate myocardial edema through Aqp1, and likely affect macrophage infiltration through the galectin9-CD44 pathway. The authors concluded that their study revealed the dynamic transcriptional heterogeneity distribution of LECs in different regions of the infarcted heart and that LECs formed different functional subgroups that may exert different bioeffects in myocardial tissue post-MI.
Strengths:
The study addresses a significant clinical challenge, and the results are of great translational value. All experiments were carefully performed, and their data support the conclusion.
Editors' comments (Public review):
Weaknesses:
(1) Figure 7C, 7E, 7I, and "Figure7-figure supplement 1 ": All data in these data panels are based on only n=3, which is insufficient. Sample sizes of n=3 are too low to correctly assess normality of distribution and, as a consequence, do not allow to select the appropriate parametric/non-parametric tests. Accordingly, no statistical comparison can be performed and all p values and symbols currently indicating statistically significant differences between groups must be removed.
(2) Figure 3A, 3B, or 3C: No information about n numbers per group. Should n numbers per group be n=4 or less, no statistical comparison can be performed and all p values and symbols indicating statistically significant differences between groups must be removed.
(3) Figure 4 E and 4F: No information about n numbers per group. Should n numbers per group be n=4 or less, no statistical comparison can be performed and all p values and symbols indicating statistically significant differences between groups must be removed.
(4) Figure 5: No information about n numbers per group is provided. Should n numbers per group be n=4 or less, no statistical comparison can be performed and all p values and symbols indicating statistically significant differences between groups must be removed.