Microscopic colitis: Etiopathology, diagnosis, and rational management
Figures
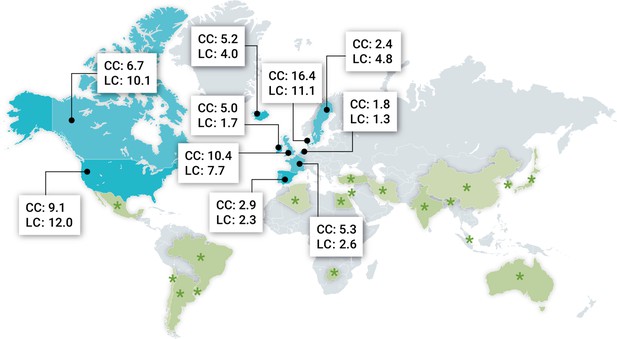
Geographic distribution of microscopic colitis in different parts of the world.
Most recent incidence rates (× 105 inhabitants per year) of both collagenous colitis (CC) and lymphocytic colitis (LC) from Europe and North America where population-based studies have been performed. Moreover, green asterisks indicate countries where microscopic colitis has been described outside Europe and North America but without incidence data. Data retrieved from Miehlke et al., 2021; Davidson et al., 2018.
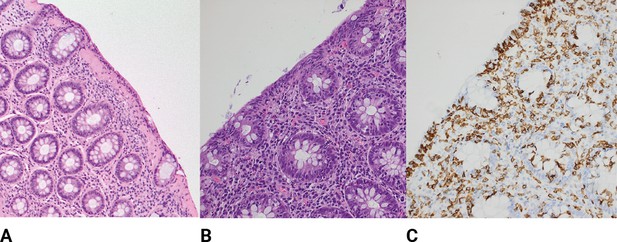
Histological findings of microscopic colitis.
(A) Typical colonic biopsy from a patient with collagenous colitis with a subepithelial collagenous band of more than 10 μM. The surface epithelium is flattened, and mucin depleted, and a mixed inflammatory infiltrate is present in the lamia propria. H&E ×20. (B) Typical colonic biopsy from a patient with lymphocytic colitis with 20 or more intraepithelial lymphocytes per 100 surface epithelial cells. A mixed inflammatory infiltrate is present in the lamia propria. H&E ×20. (C) Lymphocytic colitis, immunohistochemistry stain for CD3 high-lighting lymphocytic infiltration of the epithelium.
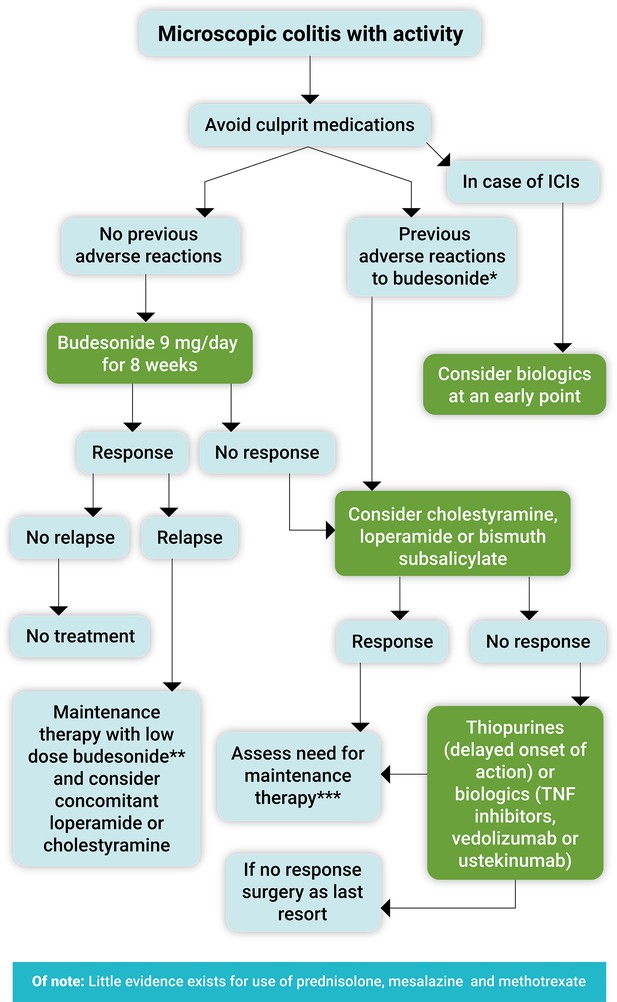
Proposed treatment algorithm for the clinical management of symptomatic microscopic colitis.
Immune checkpoint inhibitors (ICIs). *Loperamide or bismuth subsalicylate in mild cases, cholestyramine mainly if there is associated bile acid malabsorption. **Use the lowest effective dose as maintenance treatment (3–6 mg/day or 3 mg every other day). ***Long-term use of bismuth subsalicylate is not recommended due to potential neurotoxicity. Note: celiac disease should each time be excluded at least with anti-tissue transglutaminase antibody levels, and bile acid diarrhea always kept in mind.
Tables
Key histological findings in microscopic colitis: differences between collagenous and lymphocytic colitis.
| Parameter | Collagenous colitis | Lymphocytic colitis |
|---|---|---|
| Intraepithelial lymphocytes | Normal or increased number | >20 per 100 epithelial cells |
| Surface epithelium | Marked change (flattening, detachment) | Slight change (vacuolization, flattening, mucin depletion) |
| Subepithelial collagenous band | Thickening (≥10 μm) | Normal or slightly increased (<10 μm) |
| Inflammatory infiltrate in the lamina propria | Increased infiltrate (lymphocytes and plasma cells) with homogenous distribution throughout the colon | |
| Crypt architecture | Little or no distortion | |
| Inflammatory bowel disease-type focal changes | Occasional cryptitis and Paneth cell metaplasia | |