Evaluating the effect of metabolic traits on oral and oropharyngeal cancer risk using Mendelian randomization
Figures
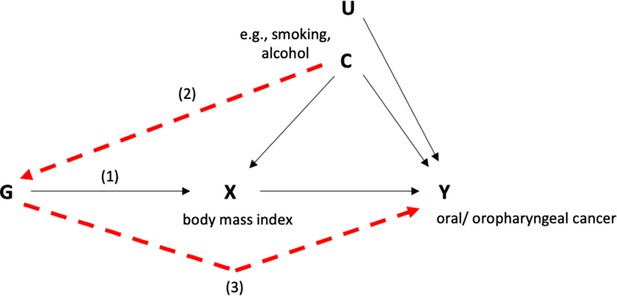
Directed acyclic graph (DAG) depicting Mendelian randomization applied to this study.
Genetic variants (G) can act as proxies or instruments to investigate if an exposure (X) is associated with a disease outcome (Y). Causal inference can be made between X and Y if the following conditions are upheld. (1) The genetic variants which make up the instrument are valid and reliably associated with the exposure (i.e., the ‘relevance assumption’); (2) There is no measured or unmeasured confounding of the association between the genetic instrument and the outcome (i.e., the ‘exchangeability’ assumption); (3) There is no independent pathway between the genetic instrument and the outcome, except through the exposure (i.e., the ‘exclusion restriction principle’).
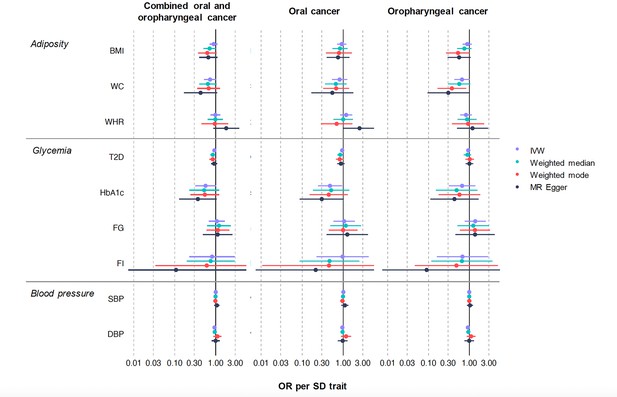
Mendelian randomization results of genetically proxied metabolic disorders with risk of oral and oropharyngeal cancer including sensitivity analyses in GAME-ON.
Oral and oropharyngeal cancer combined n = 6034, oral cancer n = 2990 and oropharyngeal cancer n = 2641. Abbreviations: IVW, inverse variance weighted; OR, odds ratio with 95% confidence intervals; BMI, body mass index; WC, waist circumference; WHR, waist–hip ratio; T2D, type 2 diabetes mellitus; FG, fasting glucose; FI, fasting insulin; HbA1c, glycated haemoglobin; SBP, systolic blood pressure; DBP, diastolic blood pressure. OR are expressed per 1 standard deviation (SD) increase in genetically predicted BMI (4.81 kg/m2), WC (0.09 unit), WHR (0.10 unit), T2D (1-log unit higher odds of T2D), FG (1-log unit increase in mmol/l fasting glucose), FI (1-log unit increase in mmol/L fasting insulin), HbA1c (1-log unit % higher glycated haemoglobin), SBP (1 unit mmHg increase), and DBP (1 unit mmHg increase).
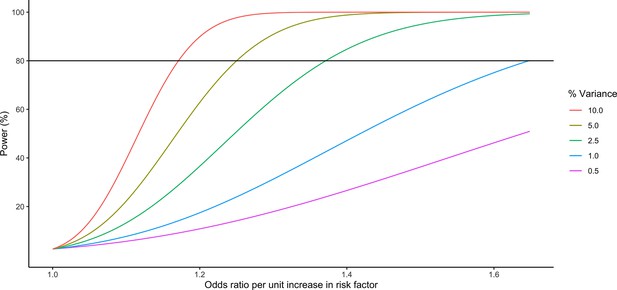
Power calculations for oral and oropharyngeal analyses in GAME-ON.
α set at 0.05.
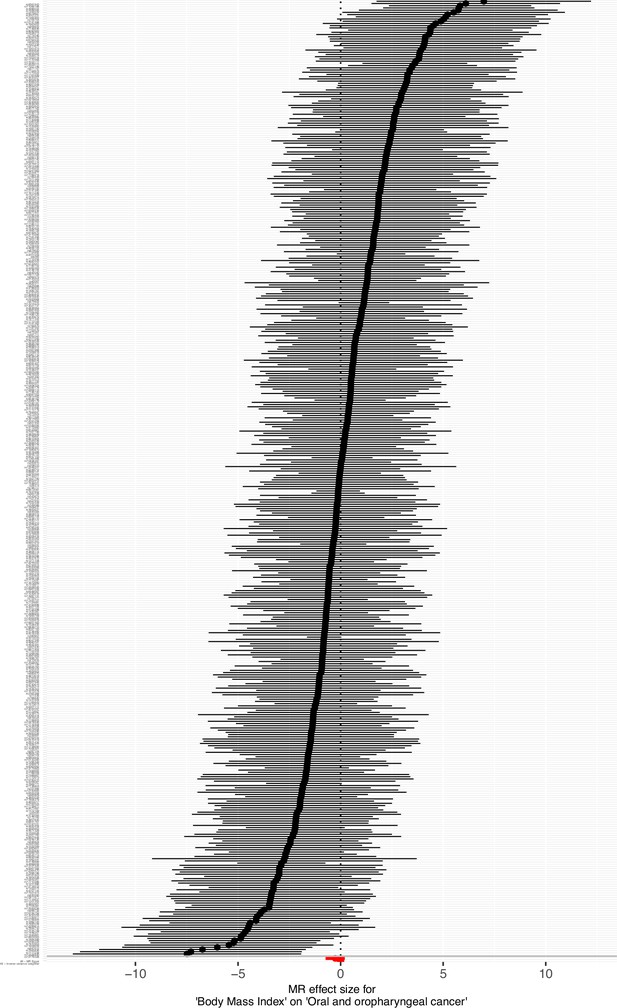
Forest plots showing Mendelian randomization results for genetically proxied body mass index (BMI) with risk of combined oral and oropharyngeal cancer in GAME-ON.
Effect estimates on oral and oropharyngeal cancer are reported on the log odds scale.
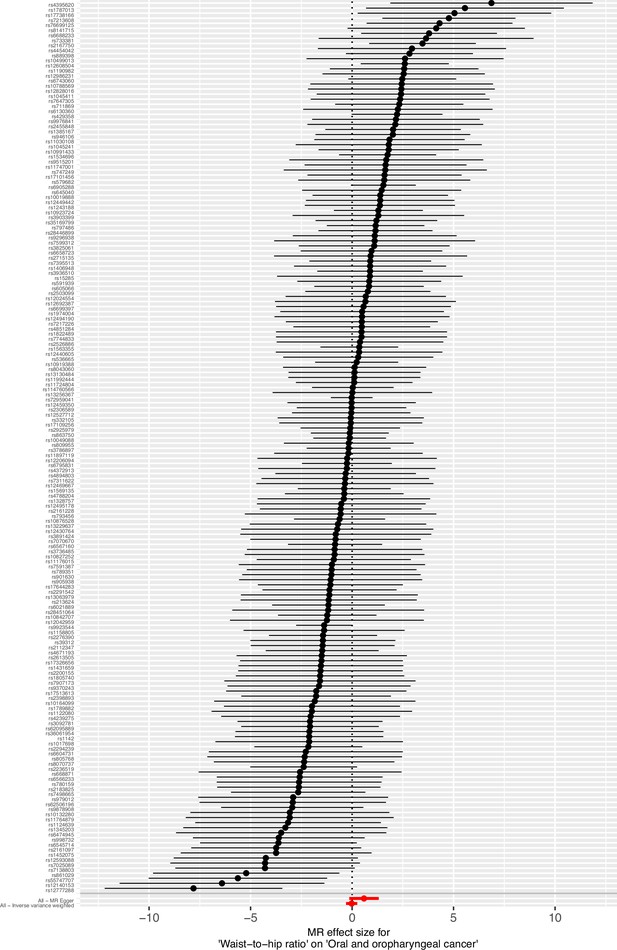
Forest plots showing Mendelian randomization results for genetically proxied waist–hip ratio (WHR) with risk of combined oral and oropharyngeal cancer in GAME-ON.
Effect estimates on oral and oropharyngeal cancer are reported on the log odds scale.
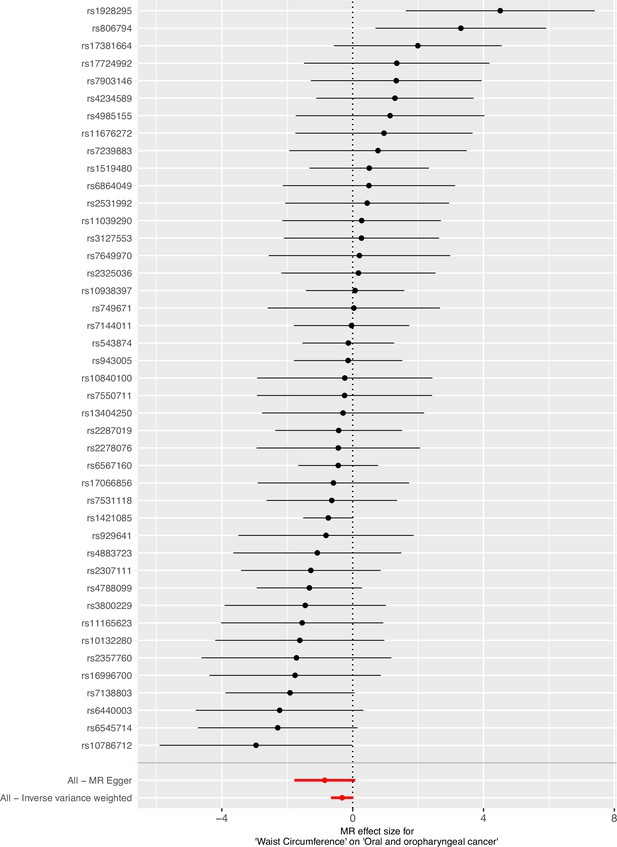
Forest plots showing Mendelian randomization results for genetically proxied waist circumference (WC) with risk of combined oral and oropharyngeal cancer in GAME-ON.
Effect estimates on oral and oropharyngeal cancer are reported on the log odds scale.
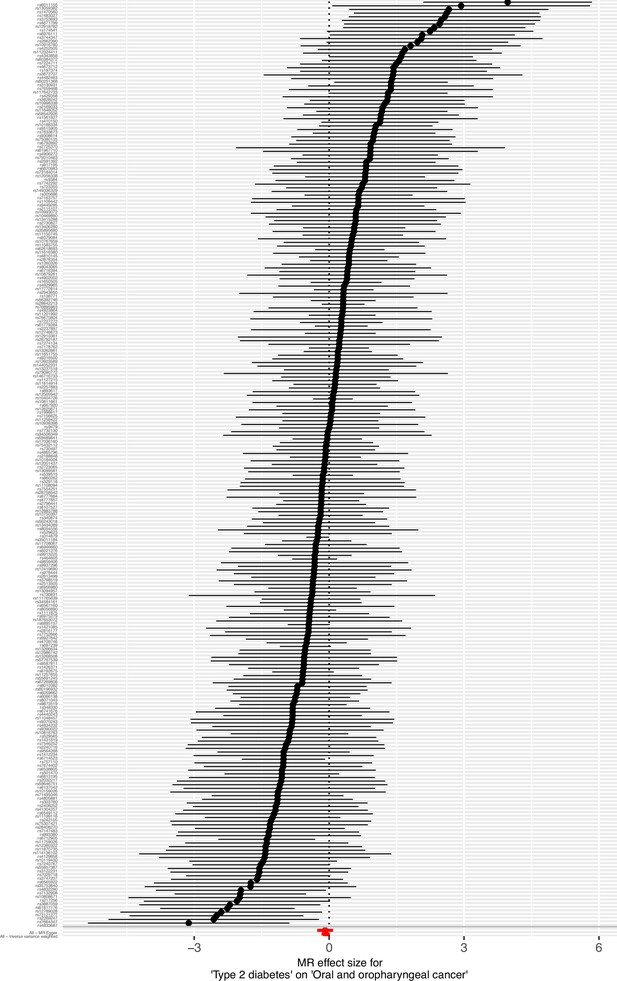
Forest plots showing Mendelian randomization results for genetically proxied type 2 diabetes mellitus (T2D) with risk of combined oral and oropharyngeal cancer in GAME-ON.
Effect estimates on oral and oropharyngeal cancer are reported on the log odds scale.
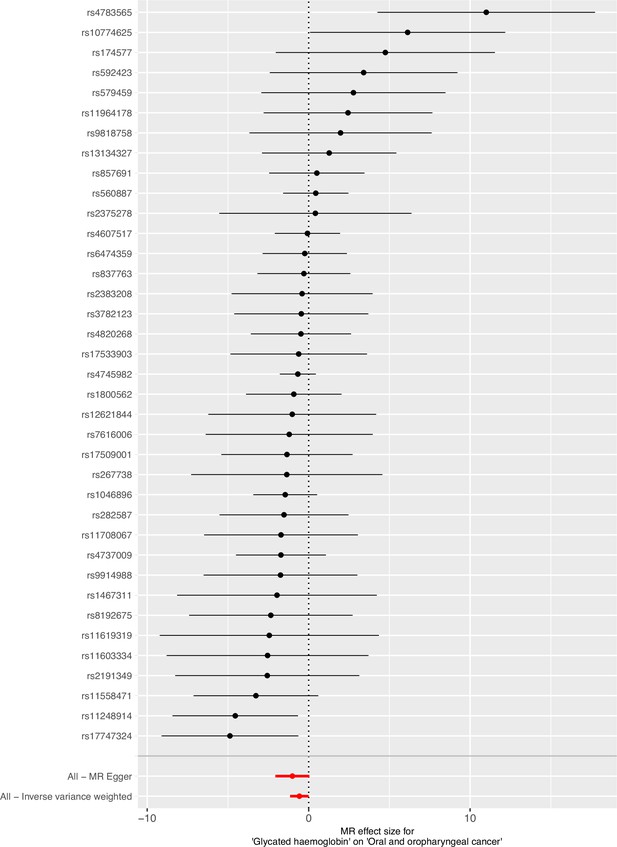
Forest plots showing Mendelian randomization results for genetically proxied glycated haemoglobin (HbA1c) with risk of combined oral and oropharyngeal cancer in GAME-ON.
Effect estimates on oral and oropharyngeal cancer are reported on the log odds scale.
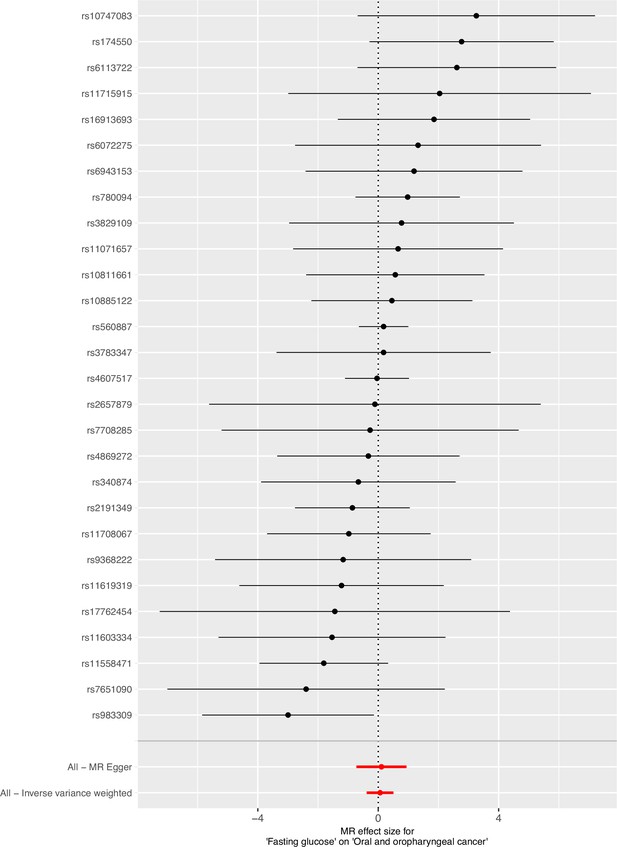
Forest plots showing Mendelian randomization results for genetically proxied fasting glucose (FG) with risk of combined oral and oropharyngeal cancer in GAME-ON.
Effect estimates on oral and oropharyngeal cancer are reported on the log odds scale.
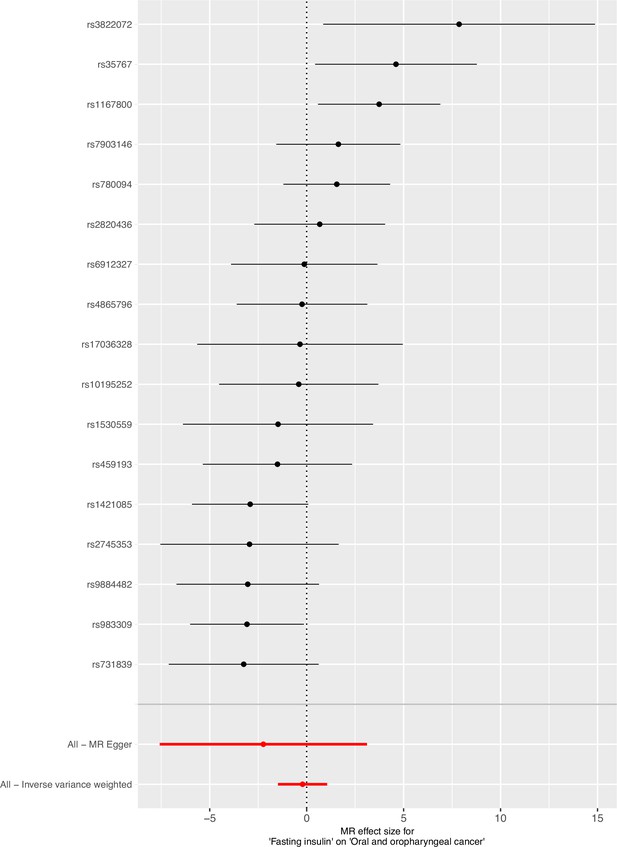
Forest plots showing Mendelian randomization results for genetically proxied fasting insulin (FI) with risk of combined oral and oropharyngeal cancer in GAME-ON.
Effect estimates on oral and oropharyngeal cancer are reported on the log odds scale.
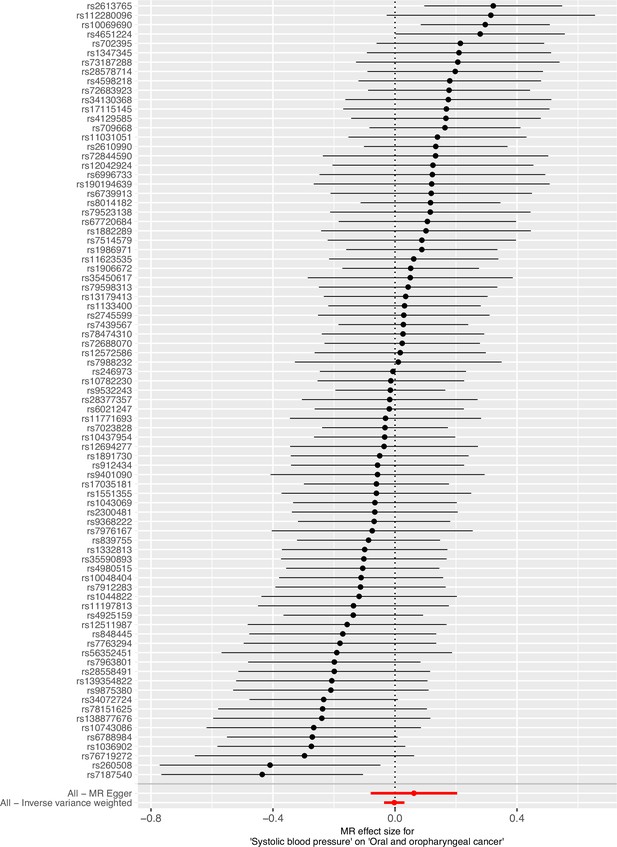
Forest plots showing Mendelian randomization results for genetically proxied systolic blood pressure (SBP) with risk of combined oral and oropharyngeal cancer in GAME-ON.
Effect estimates on oral and oropharyngeal cancer are reported on the log odds scale.
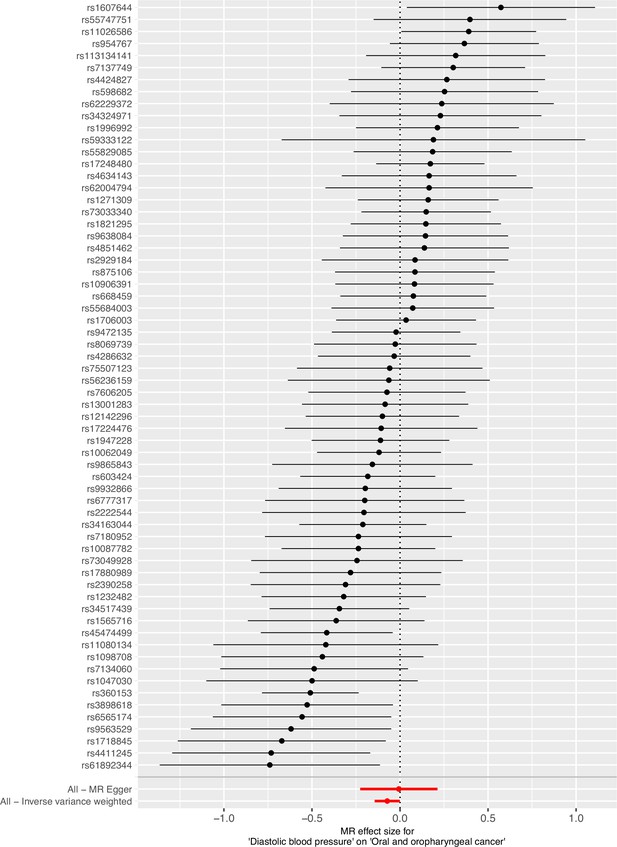
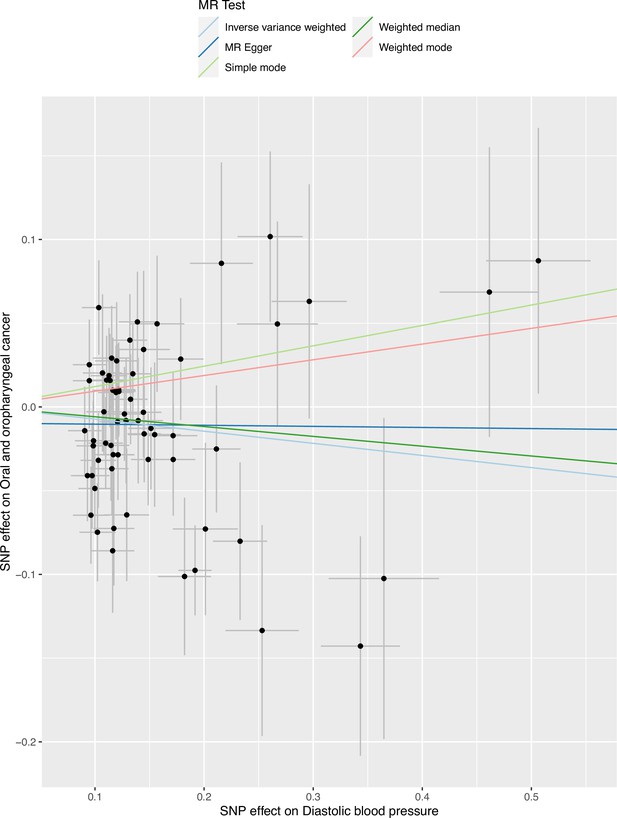
Forest plots showing Mendelian randomization results for genetically proxied diastolic blood pressure (DBP) with risk of combined oral and oropharyngeal cancer in GAME-ON.
Effect estimates on oral and oropharyngeal cancer are reported on the log odds scale.
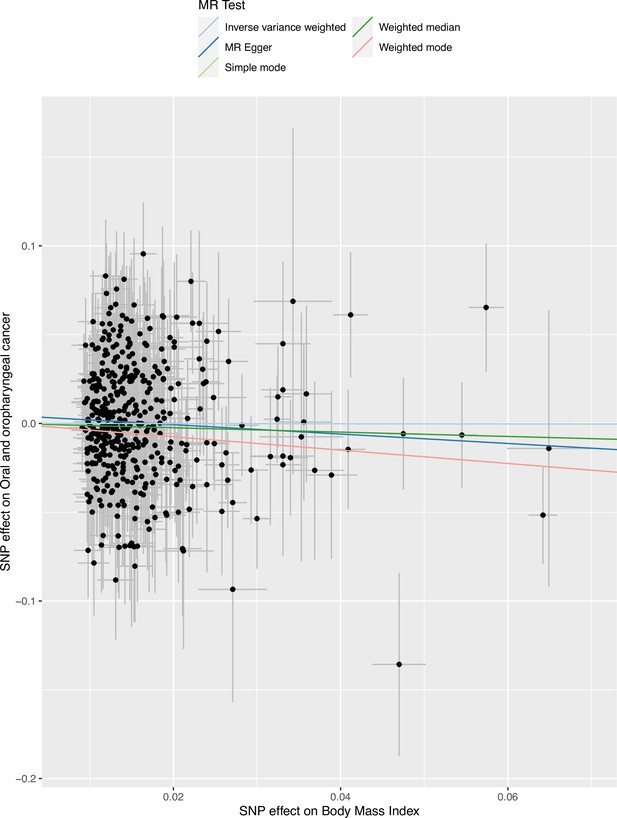
Scatter plot for body mass index (BMI) with risk of combined oral and oropharyngeal cancer in GAME-ON.
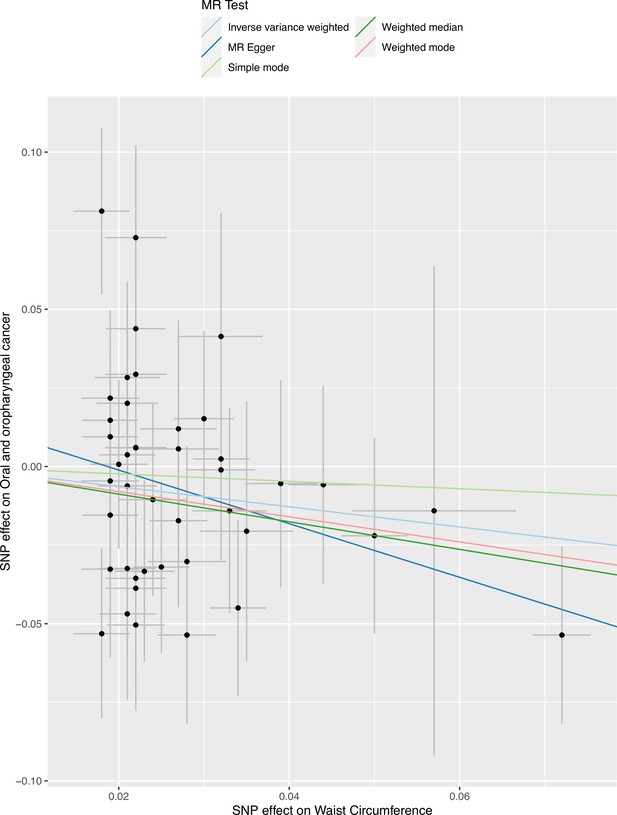
Scatter plot for waist circumference (WC) with risk of combined oral and oropharyngeal cancer in GAME-ON.
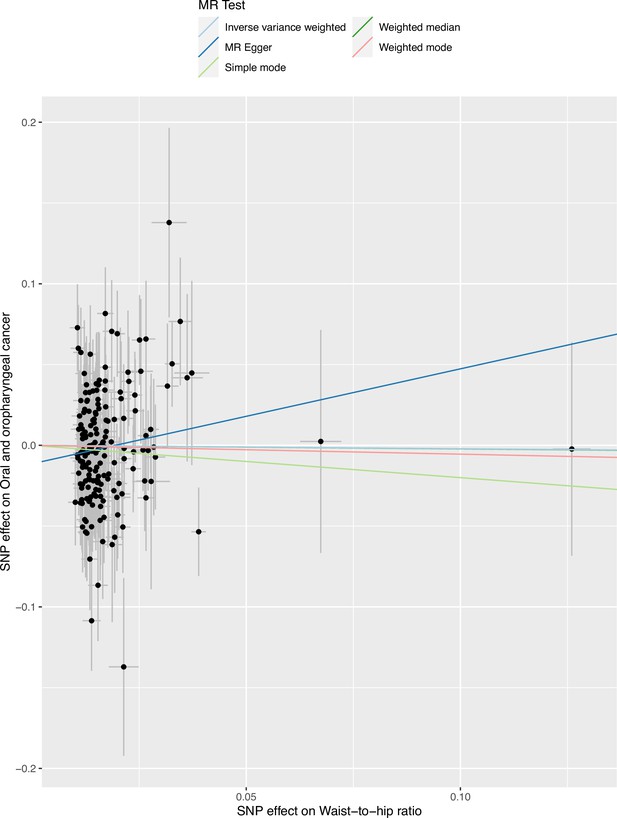
Scatter plot for waist–hip ratio (WHR) with risk of combined oral and oropharyngeal cancer in GAME-ON.
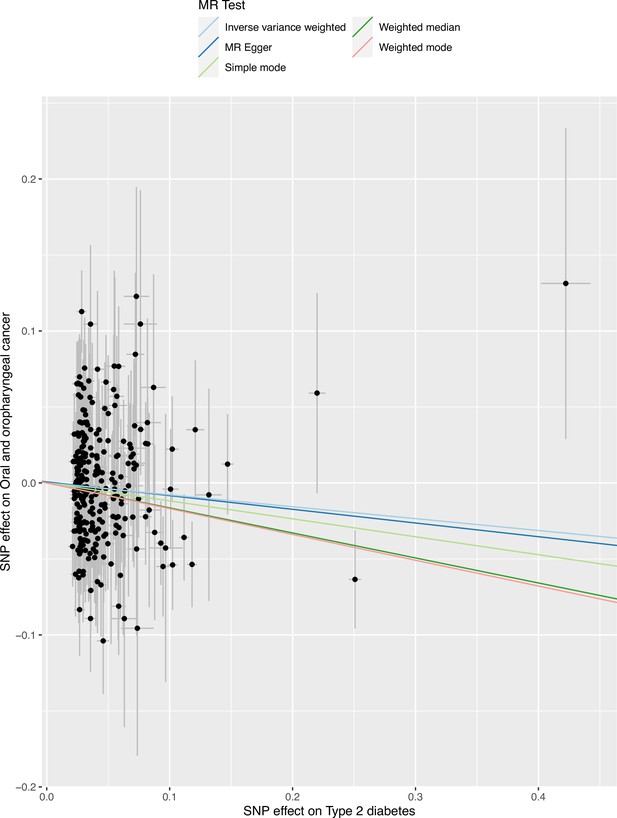
Scatter plot for type 2 diabetes mellitus (T2D) with risk of combined oral and oropharyngeal cancer in GAME-ON.
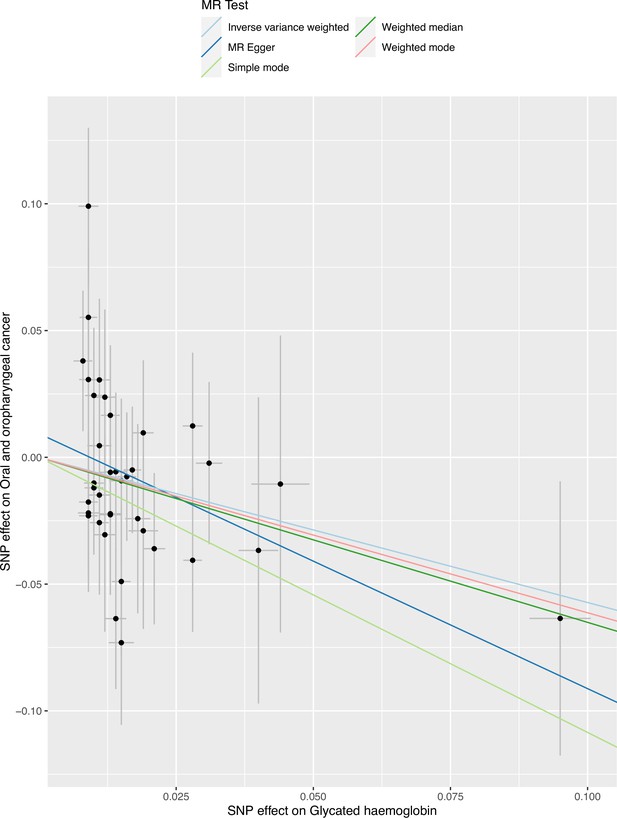
Scatter plot for glycated haemoglobin (HBA1c) with risk of combined oral and oropharyngeal cancer in GAME-ON.
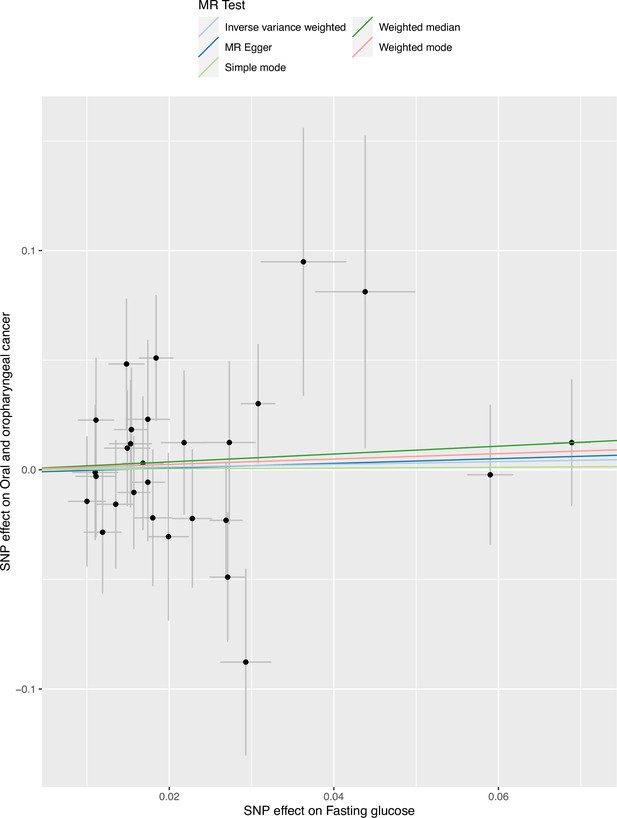
Scatter plot for fasting glucose (FG) with risk of combined oral and oropharyngeal cancer in GAME-ON.
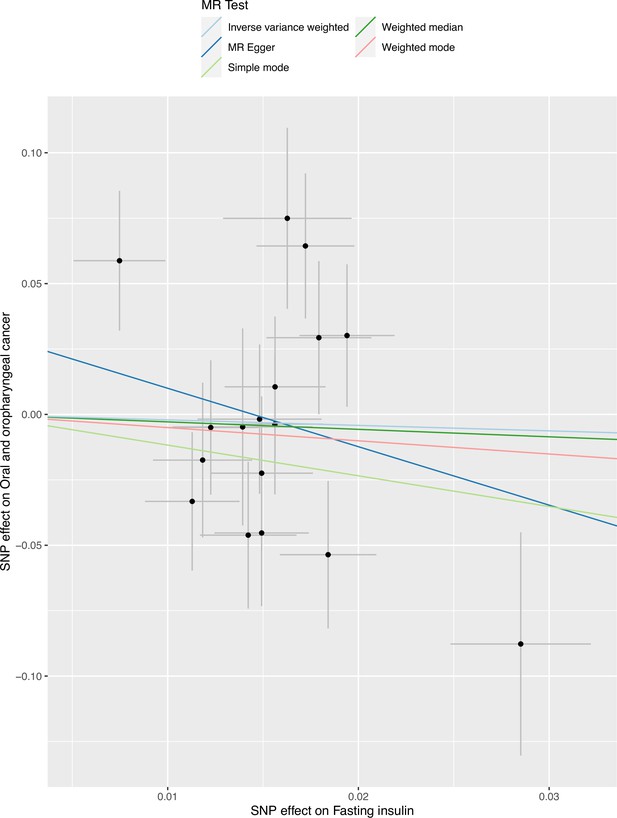
Scatter plot for fasting insulin (FI) with risk of combined oral and oropharyngeal cancer in GAME-ON.
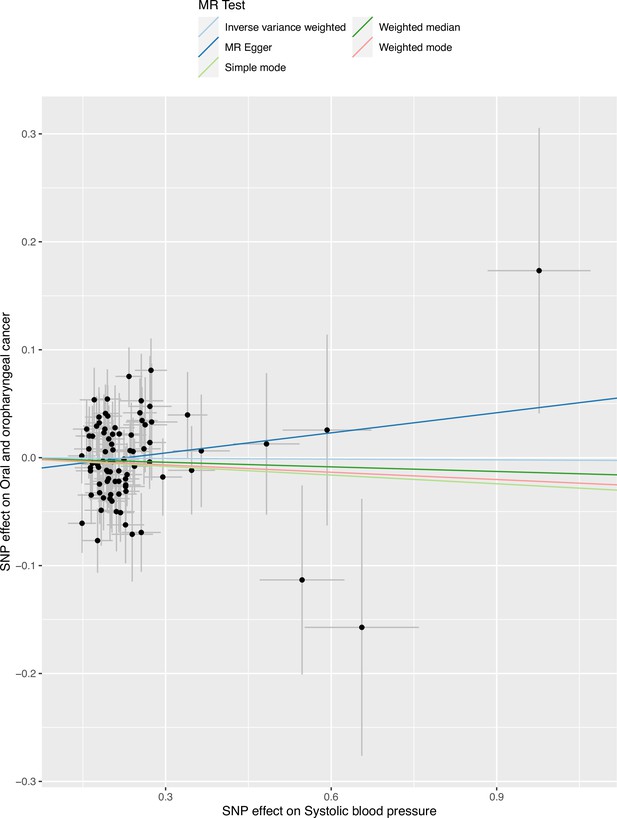
Scatter plot for systolic blood pressure (SBP) with risk of combined oral and oropharyngeal cancer in GAME-ON.
Tables
Mendelian randomization results of genetically proxied metabolic traits with risk of oral and oropharyngeal cancer in GAME-ON.
| IVW | Weighted median | Weighted mode | MR-Egger | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exposure | Outcome | Exposure/outcome source | Outcome N | Number of SNPs | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p |
| BMI | Oral and oropharyngeal cancer combined | Pulit et al. GWAS/GAME-ON | 6034 | 272 | 0.89 (0.72, 1.09) | 0.26 | 0.71 (0.50, 1.00) | 0.05 | 0.63 (0.37, 1.04) | 0.07 | 0.66 (0.40, 1.10) | 0.11 |
| Oral cancer | 2990 | 272 | 0.92 (0.71, 1.19) | 0.53 | 0.83 (0.55, 1.28) | 0.40 | 0.79 (0.38, 1.62) | 0.52 | 0.75 (0.39, 1.41) | 0.37 | ||
| Oropharyngeal cancer | 2641 | 272 | 0.89 (0.68, 1.15) | 0.36 | 0.75 (0.50, 1.13) | 0.17 | 0.53 (0.27, 1.03) | 0.06 | 0.56 (0.29, 1.07) | 0.08 | ||
| WC | Oral and oropharyngeal cancer combined | Shungin et al. GWAS/GAME-ON | 6034 | 43 | 0.73 (0.52, 1.02) | 0.07 | 0.64 (0.40, 1.05) | 0.08 | 0.67 (0.36, 1.26) | 0.22 | 0.43 (0.17, 1.08) | 0.08 |
| Oral cancer | 2990 | 43 | 0.82 (0.53, 1.26) | 0.36 | 0.66 (0.36, 1.21) | 0.18 | 0.67 (0.32, 1.39) | 0.29 | 0.54 (0.17, 1.76) | 0.31 | ||
| Oropharyngeal cancer | 2641 | 43 | 0.66 (0.43, 1.01) | 0.06 | 0.56 (0.30, 1.05) | 0.07 | 0.37 (0.17, 0.83) | 0.02 | 0.30 (0.09, 0.98) | 0.05 | ||
| WHR | Oral and oropharyngeal cancer combined | Pulit et al. GWAS/GAME-ON | 6034 | 176 | 0.98 (0.74, 1.29) | 0.88 | 0.98 (0.64, 1.49) | 0.92 | 0.95 (0.45, 2.00) | 0.89 | 1.80 (0.87, 3.71) | 0.11 |
| Oral cancer | 2990 | 176 | 1.18 (0.84, 1.65) | 0.35 | 1.00 (0.58, 1.73) | 0.99 | 0.69 (0.29, 1.67) | 0.41 | 2.49 (1.02, 6.12) | 0.05 | ||
| Oropharyngeal cancer | 2641 | 176 | 0.83 (0.59, 1.14) | 0.25 | 0.88 (0.51, 1.50) | 0.63 | 0.93 (0.37, 2.30) | 0.87 | 1.19 (0.50, 2.86) | 0.70 | ||
| T2D | Oral and oropharyngeal cancer combined | Vujkovic et al. GWAS/GAME-ON | 6034 | 254 | 0.92 (0.84, 1.01) | 0.09 | 0.85 (0.74, 0.97) | 0.02 | 0.84 (0.71, 1.01) | 0.06 | 0.91 (0.77, 1.09) | 0.31 |
| Oral cancer | 2990 | 254 | 0.94 (0.84, 1.05) | 0.27 | 0.84 (0.72, 0.99) | 0.04 | 0.82 (0.66, 1.02) | 0.08 | 0.88 (0.71, 1.08) | 0.22 | ||
| Oropharyngeal cancer | 2641 | 254 | 0.94 (0.84, 1.05) | 0.27 | 0.89 (0.73, 1.10) | 0.29 | 1.02 (0.80, 1.30) | 0.88 | 1.00 (0.81, 1.24) | 0.99 | ||
| HbA1c | Oral and oropharyngeal cancer combined | Wheeler et al. GWAS/GAME-ON (Lesseur et al., 2016) | 6034 | 37 | 0.56 (0.32, 1.00) | 0.05 | 0.52 (0.23, 1.20) | 0.12 | 0.54 (0.24, 1.21) | 0.14 | 0.37 (0.13, 1.05) | 0.07 |
| Oral cancer | 2990 | 37 | 0.48 (0.24, 0.93) | 0.03 | 0.51 (0.18, 1.41) | 0.19 | 0.44 (0.15, 1.29) | 0.14 | 0.30 (0.09, 1.03) | 0.06 | ||
| Oropharyngeal cancer | 2641 | 37 | 0.66 (0.31, 1.40) | 0.28 | 0.49 (0.15, 1.57) | 0.23 | 0.57 (0.18, 1.85) | 0.35 | 0.43 (0.11, 1.68) | 0.23 | ||
| FG | Oral and oropharyngeal cancer combined | Lagou et al. GWAS/ GAME-ON (Lesseur et al., 2016) | 6034 | 28 | 1.06 (0.68, 1.66) | 0.79 | 1.20 (0.62, 2.30) | 0.59 | 1.13 (0.60, 2.12) | 0.71 | 1.11 (0.48, 2.56) | 0.80 |
| Oral cancer | 2990 | 28 | 1.05 (0.58, 1.92) | 0.87 | 1.15 (0.48, 2.72) | 0.75 | 0.99 (0.44, 2.23) | 0.99 | 1.25 (0.39, 4.01) | 0.70 | ||
| Oropharyngeal cancer | 2641 | 28 | 1.39 (0.77, 2.51) | 0.28 | 1.24 (0.51, 3.03) | 0.63 | 1.36 (0.59, 3.18) | 0.48 | 1.38 (0.45, 4.18) | 0.58 | ||
| FI | Oral and oropharyngeal cancer combined | Lagou et al. GWAS/GAME-ON | 6034 | 17 | 0.81 (0.23, 2.89) | 0.75 | 0.75 (0.20, 2.87) | 0.68 | 0.60 (0.03, 10.79) | 0.74 | 0.11 (0.001, 22.47) | 0.43 |
| Oral cancer | 2990 | 17 | 0.96 (0.22, 4.16) | 0.96 | 0.46 (0.08, 2.47) | 0.37 | 0.45 (0.01, 19.02) | 0.68 | 0.21 (0.0004, 107.21) | 0.63 | ||
| Oropharyngeal cancer | 2641 | 17 | 0.68 (0.16, 2.87) | 0.59 | 0.66 (0.12, 3.67) | 0.63 | 0.48 (0.05, 4.99) | 0.55 | 0.09 (0.0002, 40.04) | 0.45 | ||
| SBP | Oral and oropharyngeal cancer combined | Evangelou et al., 2018 GWAS/GAME-ON (Lesseur et al., 2016) | 6034 | 83 | 1.00 (0.97, 1.03) | 0.89 | 0.99 (0.94, 1.03) | 0.55 | 0.98 (0.88, 1.09) | 0.66 | 1.06 (0.92, 1.23) | 0.39 |
| Oral cancer | 2990 | 83 | 1.01 (0.96, 1.06) | 0.74 | 0.99 (0.93, 1.04) | 0.65 | 0.95 (0.84, 1.08) | 0.48 | 1.09 (0.90, 1.33) | 0.37 | ||
| Oropharyngeal cancer | 2641 | 83 | 0.99 (0.95, 1.03) | 0.65 | 0.99 (0.94, 1.05) | 0.77 | 1.00 (0.88, 1.13) | 0.94 | 1.03 (0.87, 1.23) | 0.71 | ||
| DBP | Oral and oropharyngeal cancer combined | Evangelou et al., 2018 GWAS/GAME-ON | 6034 | 64 | 0.93 (0.87, 1.00) | 0.05 | 0.94 (0.86, 1.04) | 0.22 | 1.10 (0.88, 1.38) | 0.42 | 0.99 (0.80, 1.24) | 0.95 |
| Oral cancer | 2990 | 64 | 0.95 (0.87, 1.04) | 0.26 | 0.96 (0.86, 1.07) | 0.45 | 1.17 (0.88, 1.56) | 0.28 | 0.97 (0.74, 1.27) | 0.81 | ||
| Oropharyngeal cancer | 2641 | 64 | 0.92 (0.84, 1.00) | 0.05 | 0.94 (0.84, 1.05) | 0.29 | 1.10 (0.86, 1.41) | 0.45 | 1.00 (0.75, 1.30) | 0.93 | ||
-
OR are expressed per 1 standard deviation (SD) increase in genetically predicted BMI (4.81 kg/m2), WC (0.09 unit), WHR (0.10 unit), T2D (1-log unit higher odds of T2D), FG (1-log unit increase in mmol/L fasting glucose), FI (1-log unit increase in mmol/L fasting insulin), HbA1c (1-log unit % higher glycated haemoglobin), SBP (1 unit mmHg increase), and DBP (1 unit mmHg increase).
-
IVW, inverse variance weighted; OR, odds ratio; CI, confidence intervals; p, p-value; BMI, body mass index; WC, waist circumference; WHR, waist–hip ratio; T2D, type 2 diabetes mellitus; FG, fasting glucose; FI, fasting insulin; HbA1c, glycated haemoglobin; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Additional files
-
Supplementary file 1
Genetic variants associated with metabolic traits of interest.
- https://cdn.elifesciences.org/articles/82674/elife-82674-supp1-v2.xlsx
-
Supplementary file 2
Showing tables 2A through 2L.
Supplementary file 2, Table 2A. Assessing weak instrument bias (F-statistic) and proportion of variance in the phenotype (R2) explained by metabolic phenotype instruments. Abbreviations: BMI, body mass index; WC, waist circumference; WHR, waist–hip ratio; T2D, type 2 diabetes mellitus; HbA1c, glycated haemoglobin; FG, fasting glucose; FI, fasting insulin; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Supplementary file 2, Table 2B. Assessing heterogeneity of single nucleotide polymorphism effect estimates in inverse variance weighted (IVW) and MR-Egger regression for metabolic disorder analysis. Abbreviations: Q, Q-statistic; df, degrees of freedom; p, p-value; BMI, body mass index; WC, waist circumference; WHR, waist–hip ratio; T2D, type 2 diabetes mellitus; HbA1c, glycated haemoglobin; FG, fasting glucose; FI, fasting insulin; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Supplementary file 2, Table 2C. Assessing directional pleiotropy through MR-Egger intercept for metabolic disorder analysis. Abbreviations: SE, standard error; p, p-value; BMI, body mass index; WC, waist circumference; WHR, waist–hip ratio; T2D, type 2 diabetes mellitus; HbA1c, glycated haemoglobin; FG, fasting glucose; FI, fasting insulin; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Supplementary file 2, Table 2D. MR-PRESSO outliers detected results in the analysis of metabolic disorders on combined oral and oropharyngeal cancer risk. Abbreviations: Q-stat, Cochran’s Q-statistic; BMI, body mass index; WC, waist circumference; WHR, waist–hip ratio; T2D, type 2 diabetes mellitus; HbA1c, glycated haemoglobin; FG, fasting glucose; FI, fasting insulin; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Supplementary file 2, Table 2E. MR-PRESSO results for metabolic disorders on combined oral and oropharyngeal cancer. Abbreviations: SE, standard error; p, p-value; BMI, body mass index; WC, waist circumference; WHR, waist–hip ratio; T2D, type 2 diabetes mellitus; HbA1c, glycated haemoglobin; FG, fasting glucose; FI, fasting insulin; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Supplementary file 2, Table 2F. Outlier corrected results in the analysis of metabolic disorders on combined oral and oropharyngeal cancer risk. Abbreviations: SE, standard error; OR, odds ratio; CI, confidence intervals; IVW, inverse variance weighted; BMI, body mass index; WC, waist circumference; WHR, waist–hip ratio; T2D, type 2 diabetes mellitus; HbA1c, glycated haemoglobin; FG, fasting glucose; FI, fasting insulin; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Supplementary file 2, Table 2G. Assessing violation of the NO measurement error (NOME) assumption for instruments used in MR-Egger regression. Abbreviations: I2, I-squared statistic; BMI, body mass index; WC, waist circumference; WHR, waist–hip ratio; T2D, type 2 diabetes mellitus; HbA1c, glycated haemoglobin; FG, fasting glucose; FI, fasting insulin; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Supplementary file 2, Table 2H. SIMEX correction MR-Egger regression results for where NO measurement error (NOME) assumption may have been violated (I2 < 0.90). Abbreviations: OR, odds ratio; CI, confidence intervals; WC, waist circumference; FI, fasting insulin; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Supplementary file 2, Table 2I. Mendelian randomization results evaluating instrument-risk factor effects. Abbreviations: IVW, inverse variance weighted; OR, odds ratio; CI, confidence intervals; p, p-value; BMI, body mass index; WC, waist circumference; WHR, waist–hip ratio; T2D, type 2 diabetes mellitus; HbA1c, glycated haemoglobin; DBP, diastolic blood pressure. OR are expressed per 1 standard deviation (SD) increase in genetically predicted BMI (4.81 kg/m2), WC (0.09 unit), WHR (0.10 unit), T2D (1-log unit higher odds of T2D), HbA1c (1-log unit % higher glycated haemoglobin), and DBP (1 unit mmHg increase). Outcome beta estimates reflect the standard deviation of the phenotype.
Supplementary file 2, Table 2J. Assessing heterogeneity in Mendelian randomization results evaluating instrument-risk factor effects. Abbreviations: Q, Q-statistic; df, degrees of freedom; p, p-value; BMI, body mass index; WC, waist circumference; WHR, waist–hip ratio; T2D, type 2 diabetes mellitus; HbA1c, glycated haemoglobin; DBP, diastolic blood pressure.
Supplementary file 2, Table 2K. Assessing directional pleiotropy in Mendelian randomization results evaluating instrument-risk factor effects. Abbreviations: SE, standard error; p, p-value; BMI, body mass index; WC, waist circumference; WHR, waist–hip ratio; T2D, type 2 diabetes mellitus; HbA1c, glycated haemoglobin; DBP, diastolic blood pressure.
Supplementary file 2, Table 2L. Outlier corrected Mendelian randomization results evaluating instrument-risk factor effects. Abbreviations: IVW, inverse variance weighted; OR, odds ratio; CI, confidence intervals; p, p-value; BMI, body mass index; WC, waist circumference; WHR, waist–hip ratio; T2D, type 2 diabetes mellitus; HbA1c, glycated haemoglobin; DBP, diastolic blood pressure. OR are expressed per 1 standard deviation (SD) increase in genetically predicted BMI (4.81 kg/m2), WC (0.09 unit), WHR (0.10 unit), T2D (1-log unit higher odds of T2D), HbA1c (1-log unit % higher glycated haemoglobin), and DBP (1 unit mmHg increase). Outcome beta estimates reflect the standard deviation of the phenotype.
- https://cdn.elifesciences.org/articles/82674/elife-82674-supp2-v2.docx
-
Transparent reporting form
- https://cdn.elifesciences.org/articles/82674/elife-82674-transrepform1-v2.pdf