A modelled analysis of the impact of COVID-19-related disruptions to HPV vaccination
Figures
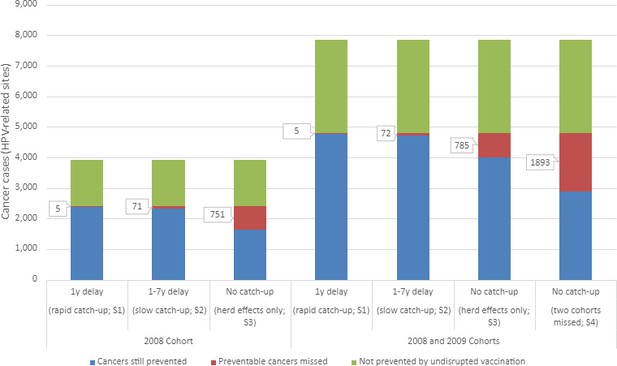
Estimated lifetime human papillomavirus (HPV)-related cancer cases from four modelled scenarios.
Scenarios include two HPV vaccination catch-up scenarios [S1: 1-year delay in vaccination (rapid); S2: 1- to 7-year delay in vaccination (slow)] and two scenarios modelling the absence of vaccination catch-up, varying in the cohort affected (S3: scenario 3 affecting the 2008 birth cohort; S4: scenario 4 affectioning the 2008 and 2009 birth cohorts).
Tables
Estimated number of human papillomavirus (HPV)-related cancer cases and cases prevented for vaccinated and unvaccinated cohorts, and four vaccination disruption scenarios.
| Modelled scenarios | Outcomes in 2008 birth cohort* | Outcomes in 2008 and 2009 birth cohorts† | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total cases | Prevented cases (unvax comparator) | Additional cases (compared to no disruption) | % Prevented (unvax comparator) | % Additional(compared to no disruption) | Total cases | Prevented cases (unvax comparator) | Additional cases(compared to no disruption) | % Prevented (unvax comparator) | % Additional(compared to no disruption) | |
| Unvaxed | 3923 | 7847 | ||||||||
| No disruption | 1532 | 2583 | 63 | 3061 | 4876 | 63 | ||||
| S1: 1-year delay | 1537 | 2579 | 4 | 63 | 0.3 | 3066 | 4781 | 5‡ | 63 | 0.2 |
| S2: 1- to 7-year delay | 1603 | 2513 | 70 | 61 | 5 | 3133 | 4714 | 72‡ | 62 | 2 |
| S3: no catch-up | 2282 | 1833 | 750 | 45 | 49 | 3846 | 4001 | 785‡ | 53 | 26 |
| S4: no catch-up (two missed cohorts) | 2503 | 1613 | 970 | 39 | 63 | 4954 | 2893 | 1892 | 40 | 62 |
-
No disruption: uninterrupted HPV vaccination in females and males at age 12 with status quo uptake; scenario 1: disruption with rapid catch-up, 1-year delay in HPV vaccine catch-up; scenario 2: disruption with slow catch-up, 1- to 7-year delay in HPV vaccine catch-up; scenario 3: disruption with no HPV vaccine catch-up (herd effects only; 2008 cohort affected); scenario 4: disruption with no HPV vaccine catch-up (herd effects only; 2008 and 2009 cohorts affected).
-
*
Includes outcomes specifically for the cohort consisting of females and males born in 2008 (any effects on the 2009 cohort are not included).
-
†
Includes outcomes specifically for the cohort consisting of females and males born in either 2008 or 2009.
-
‡
Differences between these additional cases compared to additional cases in the outcomes specific to the 2008 cohort (left-hand side of table) are additional cases in unvaccinated individuals in the 2009 cohort, due to a loss in the indirect protection they received from vaccination of the 2008 cohort in the No disruption scenario due to herd effects.
-
vax: vaccine; unvaxed: unvaccinated i.e. assuming no HPV vaccination in cohort(s).
Estimated number of cancer cases in modelled scenarios according to sex and cancer type.
| Modelled scenarios | Total cases (additional compared to no disruption) | Females, N (additional compared to no disruption) | Males, N (additional compared to no disruption) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Anal | Cervical | Oropharyngeal | Vaginal | Vulvar | Anal | Oropharyngeal | Penile | ||
| 2008 cohort | |||||||||
| Unvaxed | 3923 | 489 | 788 | 185 | 162 | 729 | 389 | 911 | 271 |
| No disruption | 1532 | 100 | 62 | 86 | 61 | 580 | 74 | 423 | 146 |
| Scenario 1 | 1537 (4)* | 101 (1) | 63 (1) | 86 | 61 | 580 | 75 (1) | 424 (1) | 146 |
| Scenario 2 | 1603 (70)* | 114 (14) | 74 (12) | 90 (4) | 64 (3) | 586 (6) | 85 (11) | 440 (17) | 150 (4) |
| Scenario 3 | 2282 (750)* | 236 (136) | 250 (188) | 121 (35) | 96 (35) | 632 (52) | 175 (101) | 593 (170) | 180 (34) |
| 2008 and 2009 cohorts | |||||||||
| Unvaxed | 7847 | 978 | 1576 | 370 | 324 | 1458 | 778 | 1822 | 542 |
| No disruption | 3061 | 199 | 125 | 172 | 122 | 1160 | 148 | 845 | 292 |
| Scenario 4 2008 cohort | 2503 (971)* | 276 (176) | 303 (241) | 131 (45) | 107 (46) | 647 (67) | 205 (131) | 644 (221) | 190 (44) |
| 2009 cohort | 2451 (922) | 268 (169) | 285 (222) | 129 (43) | 104 (43) | 644 (64) | 199 (125) | 634 (212) | 188 (42) |
| Scenario 4 total | 4954 (1892)* | 544 (345) | 588 (463) | 260 (88) | 211 (89) | 1291 (131) | 404 (256) | 1278 (433) | 378 (86) |
-
Sum of cases may not add to ‘total cases’ due to rounding.
-
Unvaxed: assuming no HPV vaccination in cohort(s); No disruption: HPV vaccination in females and males at age 12 with coverage of 82.4% in females and 75.5% in males; scenario 1: disruption with rapid catch-up, 1-year delay; scenario 2: disruption with slow catch-up, 1- to 7-year delay; scenario 3: disruption with no catch-up (herd effects only; 2008 cohort affected); scenario 4: disruption with no catch-up (herd effects only; 2008 and 2009 cohorts affected).
-
*
The number of additional cases presented in the table does not always match the difference between case figures stated for individual scenarios in Table 2, due to rounding.
Additional files
-
Supplementary file 1
Data used to inform the model.
(A) Age-specific cancer rates for females in Australia (per 100,000), 2020 projections; (B) age-specific cancer rates for males in Australia (per 100,000), 2020 projections; (C) human papillomavirus HPV attributable fractions and HPV9 preventable proportions for the cancers modelled; (D) estimated number of cervical and total cancer cases in modelled scenarios for explicit screening (main analysis) vs incidence-based approach.
- https://cdn.elifesciences.org/articles/85720/elife-85720-supp1-v1.docx
-
MDAR checklist
- https://cdn.elifesciences.org/articles/85720/elife-85720-mdarchecklist1-v1.pdf





