Association between APOL1 risk variants and the occurrence of sepsis in Black patients hospitalized with infections: a retrospective cohort study
Figures
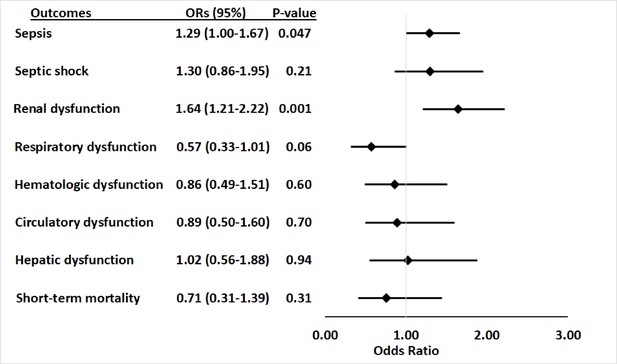
Association between APOL1 high-risk genotypes and the risk of sepsis, and septic shock, and individual sepsis organ dysfunction criteria.
Analyses were adjusted for age, sex and three principal components (PCs). Sepsis was defined as meeting the Sepsis-3 criteria for sepsis (Donnelly et al., 2017; Rhee et al., 2017), septic shock was defined using International Classification of Disease, ninth revision, Clinical Modification (ICD-9) and -10 codes for septic shock/severe sepsis (ICD-9-CM, 995.92 and 785.52; ICD-10-CM, R65.20 and R65.21); organ dysfunction data represent the individual organ dysfunction criteria in the Sepsis-3 definition; short-term mortality was defined as in-hospital death or discharge to hospice.
-
Figure 1—source data 1
Association between APOL1 high-risk genotypes and the risk of sepsis, and septic shock, and individual sepsis organ dysfunction criteria: expanded summary data.
- https://cdn.elifesciences.org/articles/88538/elife-88538-fig1-data1-v1.xlsx
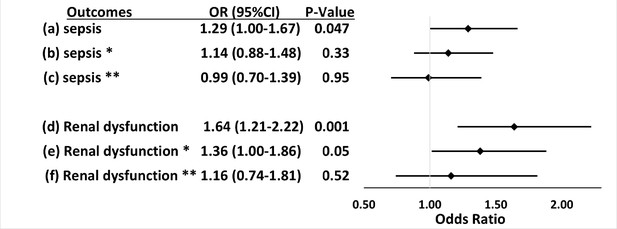
Associations between APOL1 high-risk genotypes and the risk of sepsis and renal dysfunction before and after adjustment for renal disease, and exclusion of patients with pre-existing severe renal disease.
We test the associations between APOL1 high-risk genotypes and the risk of sepsis (a, b, c) or the risk of sepsis-related renal dysfunction (d, e, f). Sepsis was defined as meeting the Sepsis-3 criteria for sepsis (Donnelly et al., 2017; Rhee et al., 2017), sepsis-related renal dysfunction represents the individual organ dysfunction criteria in the Sepsis-S3 definition. Analyses (a) and (d) were adjusted for age, sex, and three PCs. *In analyses (b) and (e) we adjusted for age, sex, three principal components, and pre-existing severe renal disease. **In analyses (c) and (f), we excluded patients with pre-existing severe renal disease and adjusted for age, sex, and three principal components.
-
Figure 2—source data 1
Associations between APOL1 high-risk genotypes and the risk of sepsis and renal dysfunction before and after adjustment for renal disease, and exclusion of patients with pre-existing severe renal disease: expanded summary data.
- https://cdn.elifesciences.org/articles/88538/elife-88538-fig2-data1-v1.xlsx
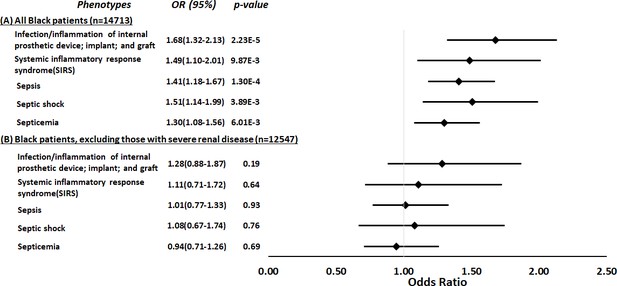
Restricted phenome-wide association analysis (PheWAS) associations between APOL1 high-risk genotype and sepsis-related phenotypes.
We tested the associations between APOL1 high-risk genotype and sepsis-related phenotypes, including infection of internal prosthetic device, systemic inflammatory response syndrome (SIRS), sepsis, septic shock, and septicemia. We conduct the analyses in all electronic medical record (EHR)-reported Black individuals with available MEGAEX genotypes in BioVU (n=14,713, panel A) and after excluding individuals with severe renal diseases (n=12,547, panel B). Analyses were adjusted for age, sex, and three principal components.
-
Figure 3—source data 1
Restricted phenome-wide association analysis (PheWAS) associations between APOL1 high-risk genotype and sepsis-related phenotypes: expanded summary data.
- https://cdn.elifesciences.org/articles/88538/elife-88538-fig3-data1-v1.xlsx
Tables
Clinical characteristics of patients admitted to the hospital with infections.
| Total (n=2242) | APOL1 low-risk group(n=1881) | APOL1 high-risk group(n=361) | p-Value | ||
|---|---|---|---|---|---|
| Gender | Female, n (%) | 1306 (58.3) | 1096 (58.3) | 210 (58.2) | 1.00 |
| Male, n (%) | 936 (41.7) | 785 (41.7) | 151 (41.8) | ||
| Age (at admission), median (Q1-Q3) | 50 (33–62) | 50 (33–63) | 50 (34–60) | 0.67 | |
| Comorbidities* | |||||
| Congestive heart failure, n (%) | 312 (13.9) | 260 (13.8) | 52 (14.4) | 0.83 | |
| Chronic pulmonary disease, n (%) | 378 (16.9) | 320 (17) | 58 (16.1) | 0.72 | |
| Cerebrovascular disease, n (%) | 221 (9.9) | 197 (10.5) | 24 (6.6) | 0.03 | |
| Dementia, n (%) | 39 (1.7) | 33 (1.8) | 6 (1.7) | 1.00 | |
| Diabetes with chronic complication, n (%) | 244 (10.9) | 200 (10.6) | 44 (12.2) | 0.44 | |
| Diabetes without chronic complication, n (%) | 170 (7.6) | 136 (7.2) | 34 (9.4) | 0.18 | |
| Hemiplegia or paraplegia, n (%) | 48 (2.1) | 41 (2.2) | 7 (1.9) | 0.93 | |
| AIDS/HIV, n (%) | 44 (2) | 35 (1.9) | 9 (2.5) | 0.56 | |
| Malignancy, including lymphoma and leukemia, except malignant neoplasm of skin, n (%) | 373 (16.6) | 318 (16.9) | 55 (15.2) | 0.48 | |
| Myocardial infarction, n (%) | 222 (9.9) | 189 (10) | 33 (9.1) | 0.67 | |
| Mild liver disease, n (%) | 38 (1.7) | 33 (1.8) | 5 (1.4) | 0.78 | |
| Moderate or severe liver disease, n (%) | 49 (2.2) | 44 (2.3) | 5 (1.4) | 0.35 | |
| Peptic ulcer disease, n (%) | 23 (1) | 19 (1) | 4 (1.1) | 1.00 | |
| Peripheral vascular disease, n (%) | 142 (6.3) | 123 (6.5) | 19 (5.3) | 0.43 | |
| Renal disease, n (%) | 545 (24.3) | 409 (21.7) | 136 (37.7) | 1.60E-10 | |
| Rheumatic disease, n (%) | 73 (3.3) | 58 (3.1) | 15 (4.2) | 0.37 | |
| Metastatic solid tumor, n (%) | 198 (8.8) | 166 (8.8) | 32 (8.9) | 1.00 | |
| Infection type† | |||||
| Circulatory, n (%) | 35 (1.6) | 29 (1.5) | 6 (1.7) | 0.86 | |
| Digestive, n (%) | 247 (11) | 217 (11.5) | 30 (8.3) | 0.07 | |
| Genitourinary, n (%) | 769 (34.3) | 648 (34.5) | 121 (33.6) | 0.75 | |
| Intestinal, n (%) | 60 (2.7) | 46 (2.4) | 14 (3.9) | 0.12 | |
| Musculoskeletal, n (%) | 109 (4.9) | 92 (4.9) | 17 (4.7) | 0.89 | |
| Neurologic, n (%) | 43 (1.9) | 35 (1.9) | 8 (2.2) | 0.65 | |
| Other bacterial, n (%) | 879 (39.3) | 723 (38.5) | 156 (43.3) | 0.08 | |
| Respiratory, n (%) | 711 (31.8) | 589 (31.3) | 122 (33.9) | 0.34 | |
| Skin, n (%) | 325 (14.5) | 286 (15.2) | 39 (10.8) | 0.03 | |
| Other, n (%) | 322 (14.4) | 268 (14.3) | 54 (15) | 0.72 | |
-
*
Comorbidities present in the preceding year as defined by criteria for the Charlson/Deyo comorbidity index.
-
†
Total n=2239; APOL1 low-risk group n=1879; APOL1 high-risk group n=360.
Additional files
-
Supplementary file 1
Supplementary tables.
(a) International Classification of Disease, ninth revision, Clinical Modification (ICD-9-CM) and ICD-10-CM codes for infection categories. (b) ICD-9-CM and ICD-10-CM codes for comorbidities. (c) List of codes to identify severe renal diseases. (d) Associations between APOL1 high-risk genotypes and sepsis-related outcomes. (e) Demographic summary of patients in the phenome-wide association analysis (PheWAS) analysis.
- https://cdn.elifesciences.org/articles/88538/elife-88538-supp1-v1.docx
-
Supplementary file 2
STROBE checklist.
- https://cdn.elifesciences.org/articles/88538/elife-88538-supp2-v1.docx
-
MDAR checklist
- https://cdn.elifesciences.org/articles/88538/elife-88538-mdarchecklist1-v1.docx





