The vaginal immunoproteome for the prediction of spontaneous preterm birth: A retrospective longitudinal study
Figures
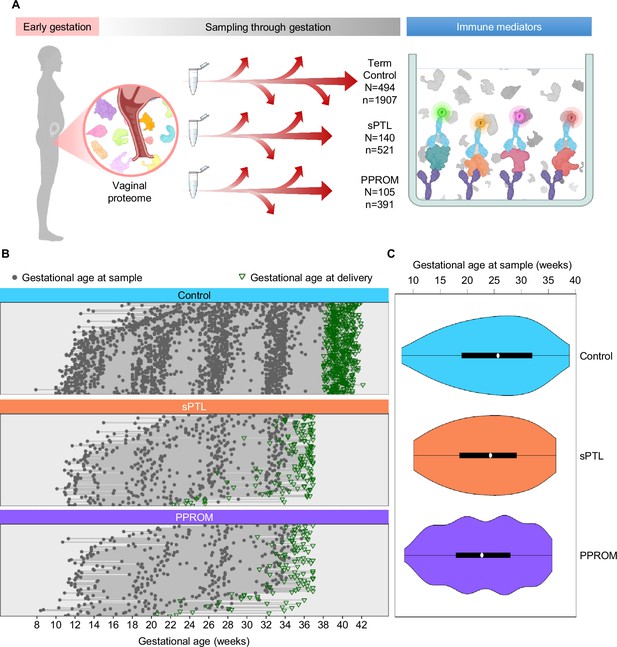
Longitudinal vaginal sampling of women with a term or preterm delivery.
(A) Representative diagram showing the collection of vaginal swabs throughout gestation from women who underwent uncomplicated term birth (control; N = 494 subjects, n = 1907 swabs), spontaneous preterm labor with intact membranes (sPTL; N = 140, n = 521), or preterm prelabor rupture of membranes (PPROM; N = 105, n = 391) to quantify the concentrations of cytokines, chemokines, and other immune mediators in the cervico-vaginal fluid by immunoassay. (B) Plots showing the distribution of swabs collected throughout gestation (weeks) for each study group. Gray dots represent gestational ages when vaginal swabs were taken, and green triangles show the gestational age at delivery. (C) Violin plots showing sample frequency across gestational age (weeks) for each study group.
© 2024, BioRender Inc. Figure 1A was created using BioRender, and is published under a CC BY-NC-ND license. Further reproductions must adhere to the terms of this license.
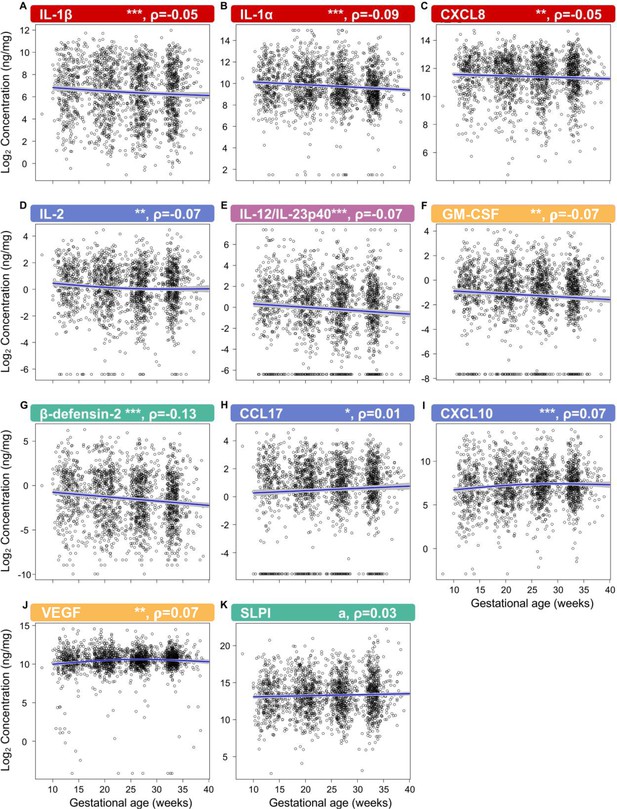
The vaginal immunoproteome is finely regulated during normal gestation.
Linear mixed effects modeling was used to determine changes in (A) IL-1β, (B) IL-1α, (C) CXCL8, (D) IL-2, (E) IL-12/IL-23p40, (F) GM-CSF, (G) β-defensin-2, (H) CCL17, (I) CXCL10, (J) VEGF, and (K) SLPI throughout pregnancies, resulting in term birth. Immune mediator labels denote category: pro-inflammatory cytokines (red), T-cell cytokine response (blue), macrophage cytokine response (purple), chemokines (green), growth factors (orange), and antimicrobial peptides (AMPs) (teal). Each black circle represents the protein concentration of one sample. Blue lines represent the linear fit, with gray shaded areas representing the 95% confidence interval of the mean. Scatterplot trends were estimated using generalized additive models with spline transformations of gestational age. *p<0.05 and q<0.1, **p<0.01 and q<0.1, ***p<0.001 and q<0.1, ap<0.05 and q>0.1. Correlation coefficients are shown above each figure as rho-values (ρ).
-
Figure 2—source data 1
Vaginal immune mediator shifts across gestational age in term uncomplicated pregnancies.
- https://cdn.elifesciences.org/articles/90943/elife-90943-fig2-data1-v1.xlsx
-
Figure 2—source data 2
The 10th, 50th, and 95th quantiles of vaginal immune mediator concentrations weekly across gestation, resulting in term birth.
- https://cdn.elifesciences.org/articles/90943/elife-90943-fig2-data2-v1.xlsx
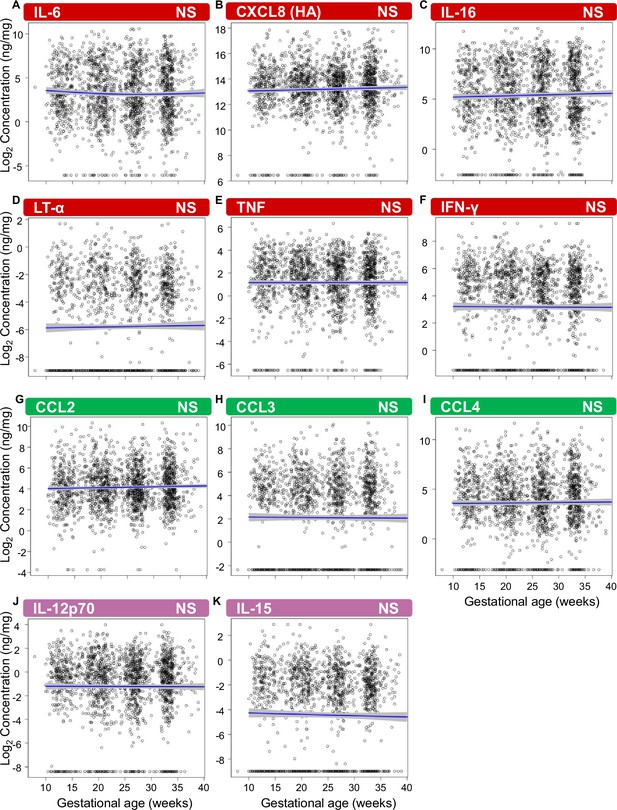
Vaginal pro-inflammatory mediators, monocyte chemoattractants, and macrophage cytokines unaltered with gestational age in women who ultimately delivered at term.
Linear mixed effects modeling was used to determine changes in (A) IL-6, (B) CXCL8 (HA, high affinity), (C) IL-16, (D) LT-α, (E) TNF, (F) IFN-γ, (G) CCL2, (H) CCL3, (I) CCL4, (J) IL-12p70, and (K) IL-15 throughout pregnancy. Each black circle represents the protein concentration of one sample. Blue lines represent the linear fit, with gray shaded areas representing the 95% confidence interval of the mean. Scatterplot trends were estimated using generalized additive models with spline transformations of gestational age. Immune mediator labels denote their immunobiology category: pro-inflammatory cytokines (red), chemokines (green), and macrophage cytokine response (purple). NS, nonsignificant.
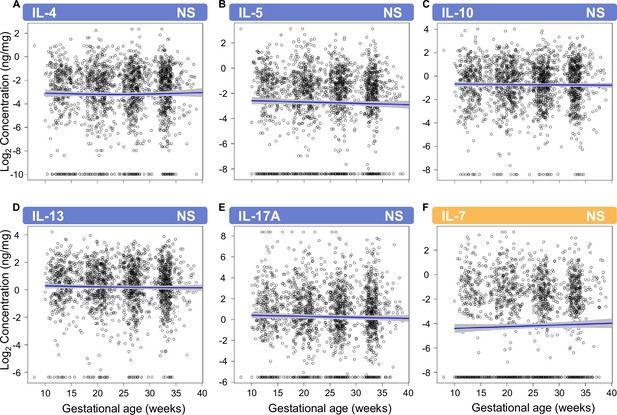
Vaginal T-cell cytokines and the growth factor IL-7 that are unaltered with gestational age in women who ultimately delivered at term.
Linear mixed effects modeling was used to determine changes in (A) IL-4, (B) IL-5, (C) IL-10, (D) IL-13, (E) IL-17A, and (F) IL-7 throughout pregnancy. Each black circle represents the protein concentration of one sample. Blue lines represent the linear fit, with gray shaded areas representing the 95% confidence interval. Scatterplot trends were estimated using generalized additive models with spline transformations of gestational age. Immune mediator labels denote their immunobiology category: T-cell cytokine response (blue) and growth factors (orange). NS, nonsignificant.
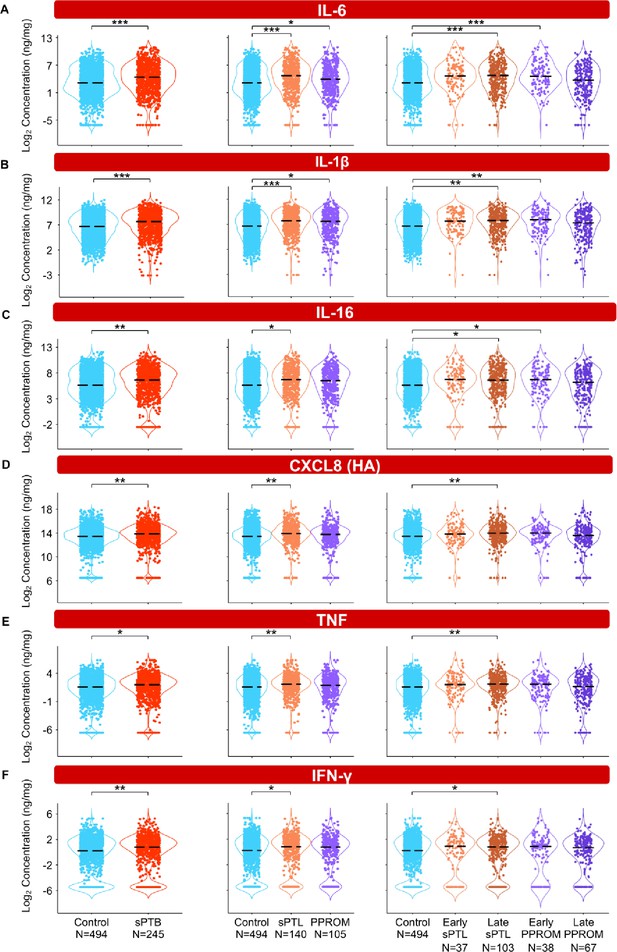
The vaginal immunoproteome of women with spontaneous preterm birth (sPTB) displays a pro-inflammatory profile.
Linear mixed effects modeling adjusted for gestational age at sampling, body mass index (BMI), parity, and history of preterm birth was used to compare the concentrations of proteins between groups. Violin plots showing the concentrations of (A) IL-6, (B) IL-1β, (C) IL-16, (D) CXCL8 (HA), (E) TNF, and (F) IFN-γ. Violin plots for early spontaneous preterm labor with intact membranes (sPTL) and early preterm prelabor rupture of membranes (PPROM) contain data <34 weeks, all other violin plots contain data <37 weeks. Light blue = controls, red = all sPTB, orange = sPTL, purple = PPROM, light orange = early sPTL (gestational age at delivery <34 weeks), dark orange = late sPTL (gestational age at delivery 34–36+6 weeks), light purple = early PPROM (gestational age at delivery <34 weeks), dark purple = late PPROM (gestational age at delivery 34–36+6 weeks). *p<0.05, **p<0.01, ***p<0.001.
-
Figure 3—source data 1
Pro-inflammatory immune mediator concentration differences between term and sPTB cases with and without adjustment for maternal characteristics, between term, sPTL, and PPROM cases, and between term, early sPTL, late sPTL, early PPROM, and late PPROM cases.
Red text values in cells indicate significance of the immune mediator both before and after adjustment for maternal characteristics. Gray highlighted cells indicate significance for immune mediators without adjustment for maternal characteristics. Yellow highlighted cells indicate significance of the immune mediator for the etiology of preterm birth and the gestational age period at delivery.
- https://cdn.elifesciences.org/articles/90943/elife-90943-fig3-data1-v1.xlsx
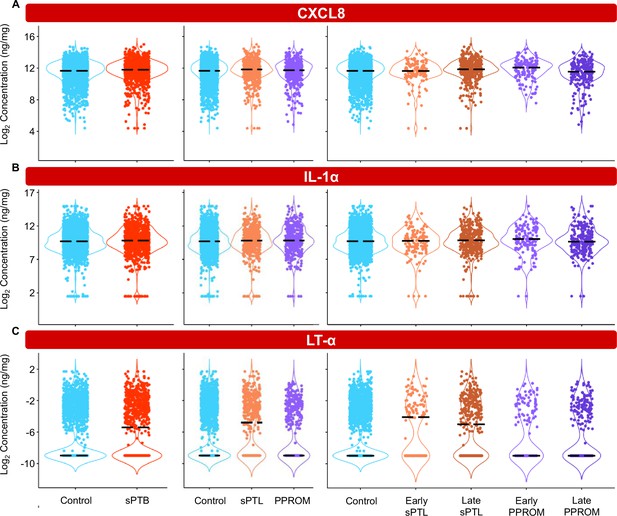
Specific pro-inflammatory cytokines in the vaginal fluid are unaltered with birth outcome.
Linear mixed effects modeling adjusted for gestational age at sampling, body mass index (BMI), parity, and history of preterm birth was used to compare the concentrations of proteins between groups. Violin plots showing the concentrations of (A) CXCL8, (B) IL-1α, and (C) LT-α. Violin plots for early spontaneous preterm labor with intact membranes (sPTL) and early preterm prelabor rupture of membranes (PPROM) contain data <34 weeks, all other violin plots contain data <37 weeks. Light blue = controls, red = all spontaneous preterm births (sPTB), orange = sPTL, purple = PPROM, light orange = early sPTL (gestational age at delivery <34 weeks), dark orange = late sPTL (gestational age at delivery 34–36+6 weeks), light purple = early PPROM (gestational age at delivery <34 weeks), dark purple = late PPROM (gestational age at delivery 34–36+6 weeks).
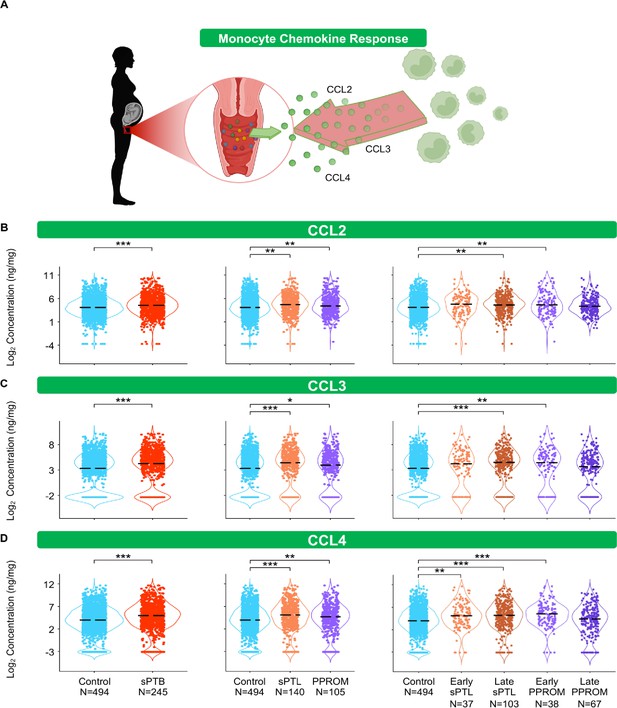
The vaginal immunoproteome of women with spontaneous preterm birth (sPTB) harbors a stereotypical monocyte response.
(A) Linear mixed effects modeling adjusted for gestational age at sampling, body mass index (BMI), parity, and history of preterm birth was used to compare the concentrations of proteins between groups. Violin plots showing the concentrations of (B) CCL2, (C) CCL3, and (D) CCL4. Violin plots for early spontaneous preterm labor with intact membranes (sPTL) and early preterm prelabor rupture of membranes (PPROM) contain data <34 weeks, all other violin plots contain data <37 weeks. Light blue = controls, red = all sPTB, orange = sPTL, purple = PPROM, light orange = early sPTL (gestational age at delivery <34 weeks), dark orange = late sPTL (gestational age at delivery 34–36+6 weeks), light purple = early PPROM (gestational age at delivery <34 weeks), dark purple = late PPROM (gestational age at delivery 34–36+6 weeks). *p<0.05, **p<0.01, ***p<0.001.
© 2024, BioRender Inc. Figure 4A was created using BioRender, and is published under a CC BY-NC-ND license. Further reproductions must adhere to the terms of this license.
-
Figure 4—source data 1
Monocyte chemokine and macrophage cytokine concentration differences between term and sPTB cases with and without adjustment for maternal characteristics between term, sPTL, and PPROM cases as well as between term, early sPTL, late sPTL, early PPROM, and late PPROM cases.
Red text values in cells indicate significance of the immune mediator both before and after adjustment for maternal characteristics. Gray highlighted cells indicate significance for immune mediators without adjustment for maternal characteristics. Yellow highlighted cells indicate significance of the immune mediator for the etiology of preterm birth and the gestational age period at delivery.
- https://cdn.elifesciences.org/articles/90943/elife-90943-fig4-data1-v1.xlsx
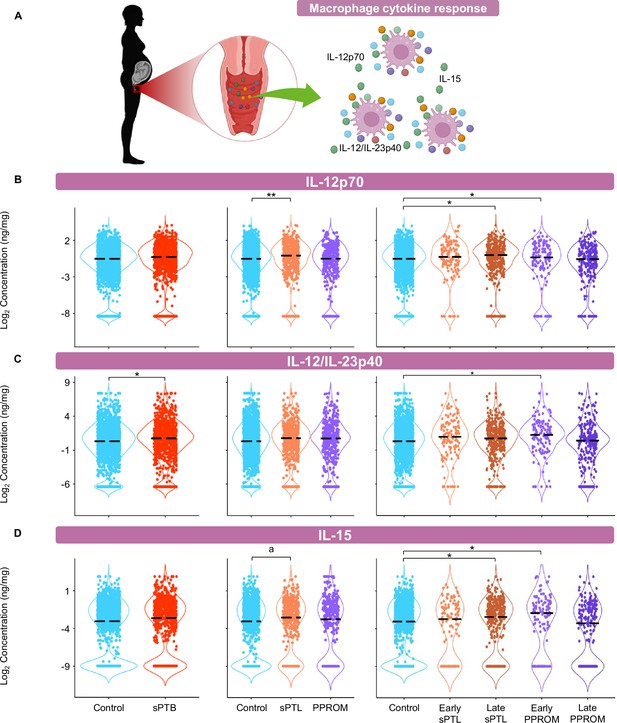
The vaginal immunoproteome of women with spontaneous preterm birth (sPTB) includes altered macrophage cytokines.
(A) Linear mixed effects modeling adjusted for gestational age at sampling, body mass index (BMI), parity, and history of preterm birth was used to compare the concentrations of proteins between groups. Violin plots showing the concentrations of (B) IL-12p70, (C) IL-12/IL-23p40, and (D) IL-15. Violin plots for early spontaneous preterm labor with intact membranes (sPTL) and early preterm prelabor rupture of membranes (PPROM) contain data <34 weeks, all other violin plots contain data <37 weeks. Light blue = controls, red = all sPTB, orange = sPTL, purple = PPROM, light orange = early sPTL (gestational age at delivery <34 weeks), dark orange = late sPTL (gestational age at delivery 34–36+6 weeks), light purple = early PPROM (gestational age at delivery <34 weeks), dark purple = late PPROM (gestational age at delivery 34–36+6 weeks). *p<0.05, **p<0.01, ap>0.05 and q<0.1.
© 2024, BioRender Inc. Figure 4—figure supplement 1A was created using BioRender, and is published under a CC BY-NC-ND license. Further reproductions must adhere to the terms of this license.
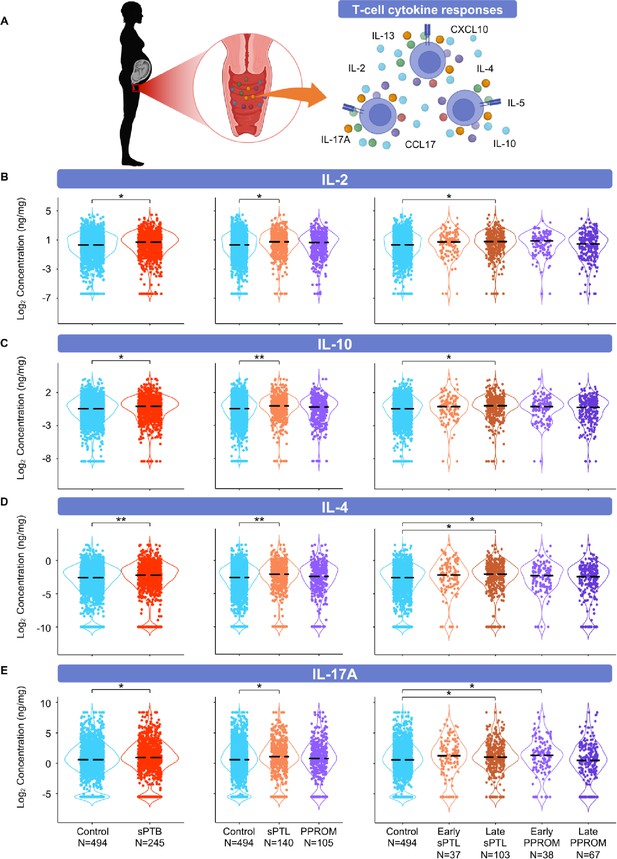
The vaginal immunoproteome of women with spontaneous preterm birth (sPTB) is enriched for T-cell mediators.
(A) Linear mixed effects modeling adjusted for gestational age at sampling, body mass index (BMI), parity, and history of preterm birth was used to compare the concentrations of proteins between groups. Violin plots showing the concentrations of (B) IL-2, (C) IL-10, (D) IL-4, and (E) IL-17A. Violin plots for early spontaneous preterm labor with intact membranes (sPTL) and early preterm prelabor rupture of membranes (PPROM) contain data <34 weeks, all other violin plots contain data <37 weeks. Light blue = controls, red = all sPTB, orange = sPTL, purple = PPROM, light orange = early sPTL (gestational age at delivery <34 weeks), dark orange = late sPTL (gestational age at delivery 34–36+6 weeks), light purple = early PPROM (gestational age at delivery <34 weeks), dark purple = late PPROM (gestational age at delivery 34–36+6 weeks). *p<0.05, **p<0.01.
© 2024, BioRender Inc. Figure 5A was created using BioRender, and is published under a CC BY-NC-ND license. Further reproductions must adhere to the terms of this license.
-
Figure 5—source data 1
T-cell cytokine concentration differences between term and sPTB cases with and without adjustment for maternal characteristics, between term, sPTL, and PPROM cases, and between term, early sPTL, late sPTL, early PPROM, and late PPROM cases.
Red text values in cells indicate significance of the immune mediator both before and after adjustment for maternal characteristics. Gray highlighted cells indicate significance for immune mediators without adjustment for maternal characteristics. Yellow highlighted cells indicate significance of the immune mediator for the etiology of preterm birth and the gestational age period at delivery.
- https://cdn.elifesciences.org/articles/90943/elife-90943-fig5-data1-v1.xlsx
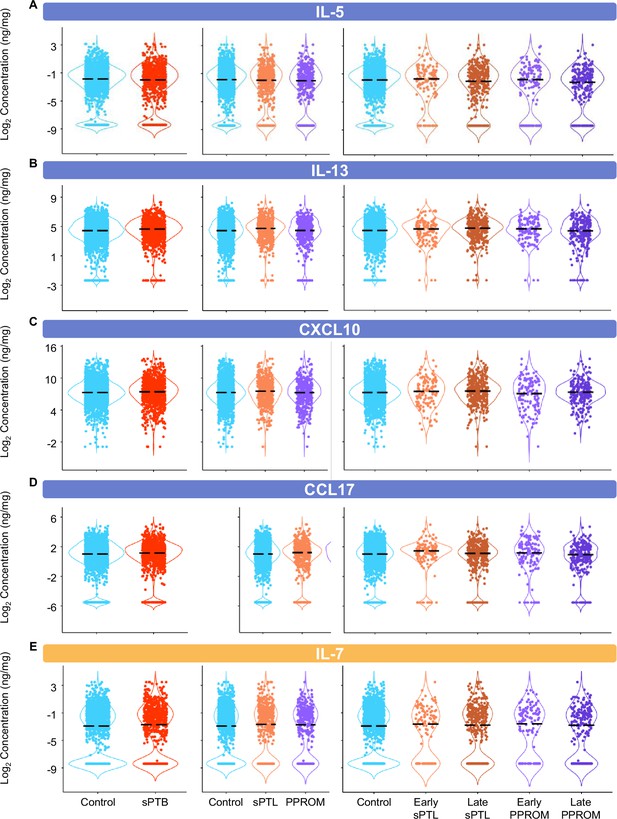
T-cell cytokines/chemokines and the growth factor IL-7 in the vaginal fluid are unaltered with birth outcome.
Linear mixed effects modeling adjusted for gestational age at sampling, body mass index (BMI), parity, and history of preterm birth was used to compare the concentrations of proteins between groups. Violin plots showing the concentrations of (A) IL-5, (B) IL-13, (C) CXCL10, (D) CCL17, and (E) IL-7. Violin plots for early spontaneous preterm labor with intact membranes (sPTL) and early preterm prelabor rupture of membranes (PPROM) contain data <34 weeks, all other violin plots contain data <37 weeks. Light blue = controls, red = all spontaneous preterm births (sPTB), orange = sPTL, purple = PPROM, light orange = early sPTL (gestational age at delivery <34 weeks), dark orange = late sPTL (gestational age at delivery 34–36+6 weeks), light purple = early PPROM (gestational age at delivery <34 weeks), dark purple = late PPROM (gestational age at delivery 34–36+6 weeks). Immune mediator labels denote their immunobiology category: T-cell cytokine response (blue) and growth factors (orange).
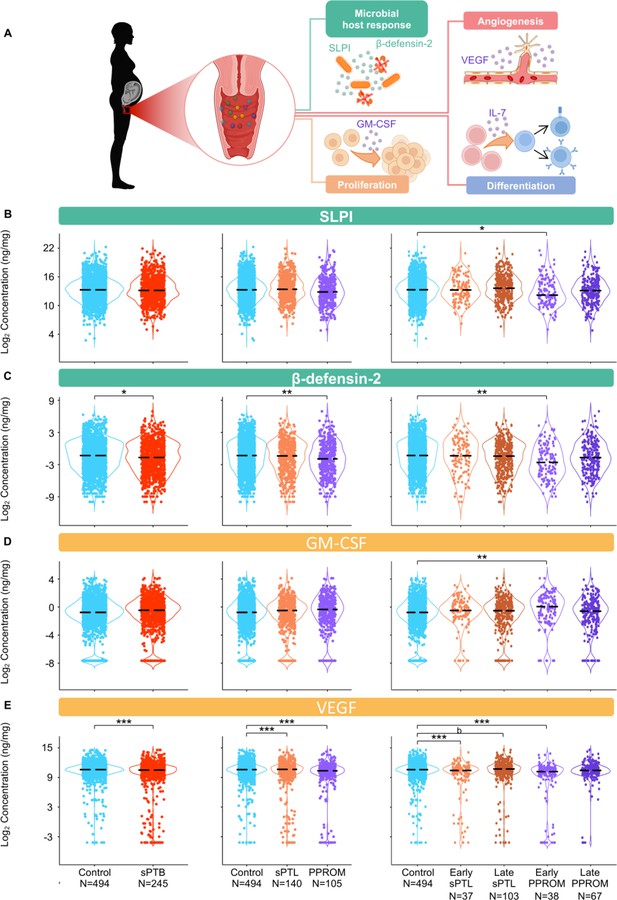
The vaginal immunoproteome of women with spontaneous preterm birth (sPTB) exhibits altered antimicrobial proteins and growth factors.
(A) Linear mixed effects modeling adjusted for gestational age at sampling, body mass index (BMI), parity, and history of preterm birth was used to compare the concentrations of proteins between groups. Immune mediator labels denote category: antimicrobial peptides (AMPs) (teal) and growth factors (orange). Violin plots showing the concentrations of (B) SLPI, (C) β-defensin-2, (D) GM-CSF, and (E) VEGF. Violin plots for early spontaneous preterm labor with intact membranes (sPTL) and early preterm prelabor rupture of membranes (PPROM) contain data <34 weeks, all other violin plots contain data <37 weeks. Light blue = controls, red = all sPTB, orange = sPTL, purple = PPROM, light orange = early sPTL (gestational age at delivery <34 weeks), dark orange = late sPTL (gestational age at delivery 34–36+6 weeks), light purple = early PPROM (gestational age at delivery <34 weeks), dark purple = late PPROM (gestational age at delivery 34–36+6 weeks). *p<0.05, **p<0.01, ***p<0.001, bp>0.05 and q<0.1.
© 2024, BioRender Inc. Figure 6A was created using BioRender, and is published under a CC BY-NC-ND license. Further reproductions must adhere to the terms of this license.
-
Figure 6—source data 1
Antimicrobial peptide and growth factor concentration differences between term and sPTB cases with and without adjustment for maternal characteristics, between term, sPTL, and PPROM cases, and between term, early sPTL, late sPTL, early PPROM, and late PPROM cases.
Red text values in cells indicate significance of the immune mediator both before and after adjustment for maternal characteristics. Gray highlighted cells indicate significance for immune mediators without adjustment for maternal characteristics. Yellow highlighted cells indicate significance of the immune mediator for the etiology of preterm birth and the gestational age period at delivery.
- https://cdn.elifesciences.org/articles/90943/elife-90943-fig6-data1-v1.xlsx
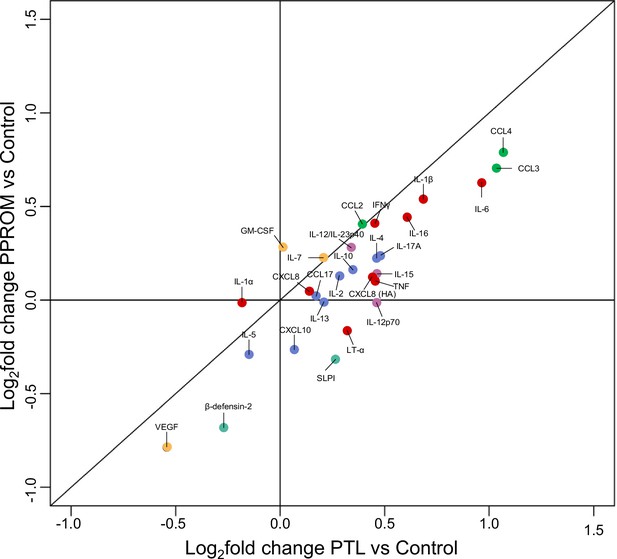
Changes in the vaginal immunoproteome are correlated between spontaneous preterm labor with intact membranes (sPTL) and preterm prelabor rupture of membranes (PPROM).
Correlation of changes in the concentrations of vaginal immune mediators observed in PPROM vs. control (y-axis; coefficient PPROM vs. control) and in sPTL vs. control (coefficient sPTL vs. control). Proteins are categorized into pro-inflammatory cytokines (red), T-cell cytokine response (blue), macrophage cytokine response (purple), chemokines (green), growth factors (orange), and antimicrobial peptides (AMPs) (teal).
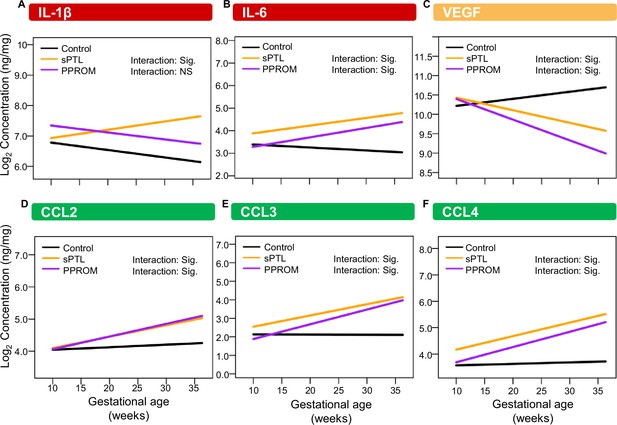
The trajectory of specific vaginal immune mediators across gestation is distinct with negative birth outcomes compared to gestations resulting in term birth.
Linear mixed effect modeling with an allowance for an interaction term between preterm birth subsets and gestational age at sampling was used to compare the trajectory of immune mediator concentrations across gestation in pregnancies resulting in black = term delivery, orange = spontaneous preterm labor with intact membranes (sPTL), purple = preterm prelabor rupture of membranes (PPROM). Modeling showed significant change in the trendline of sPTL and/or PPROM in (A) IL-1β, (B) IL-6, (C) VEGF, (D) CCL2, (E) CCL3, and (F) CCL4. Immune mediator labels denote their immunobiology category: pro-inflammatory cytokines (red), growth factors (orange), chemokines (green), and macrophage cytokine response (purple).
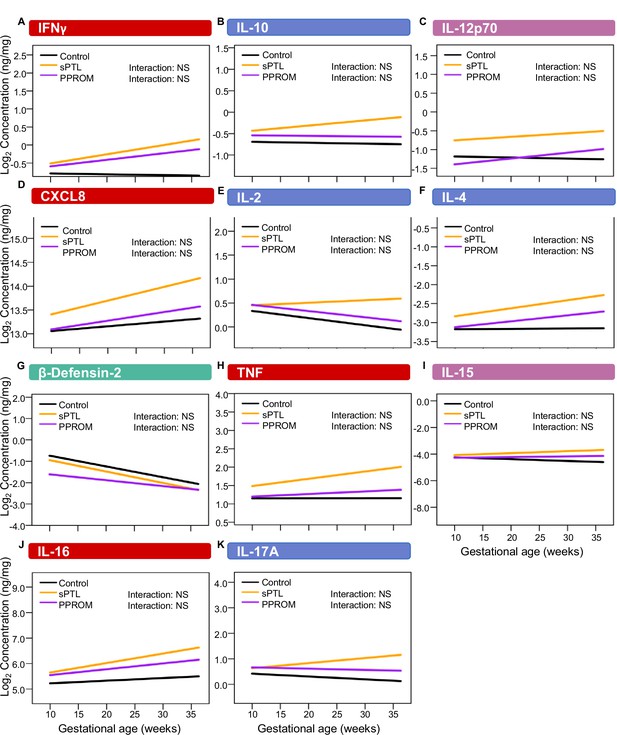
The trajectory of specific vaginal immune mediators across gestation is unaltered with birth outcome.
Linear mixed effect modeling with an allowance for an interaction term between preterm birth subsets and gestational age at sampling was used to compare the trajectory of immune mediator concentrations across gestation in pregnancies resulting in black = term delivery, orange = spontaneous preterm labor with intact membranes (sPTL), purple = preterm prelabor rupture of membranes (PPROM). Modeling showed significant change in the trendline of sPTL and/or PPROM in (A) IFNγ, (B) IL-10, (C) IL-12p70, (D) CXCL8, (E) IL-2, (F) IL-4 (G) β-defensin-2 (H) TNF, (I) IL-15, (J) IL-16, and (K) IL-17A. Immune mediator labels denote their immunobiology category: pro-inflammatory cytokines (red), T-cell cytokine response (blue), macrophage cytokine response (purple), and antimicrobial peptides (AMPs) (teal). NS, non-significant.
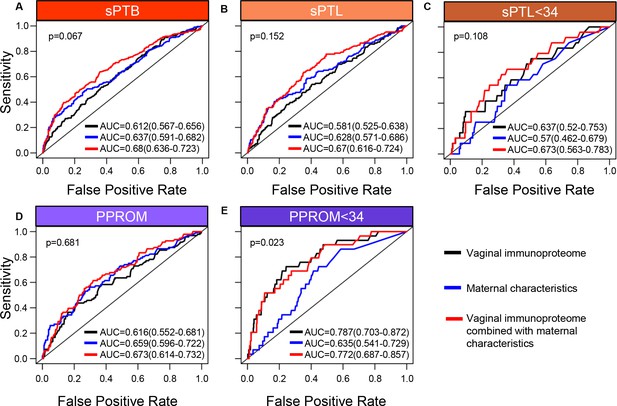
The vaginal immunoproteome allows for the prediction of early spontaneous preterm births (sPTB).
Random forest modeling including protein concentrations generated from the last swab before 28 weeks of gestation was used to generate models using the combination of all cytokines, chemokines, immune-related growth factors, and antimicrobial molecules in this study (black line), maternal characteristics (blue line), or the combination of all cytokines, chemokines, immune-related growth factors, and antimicrobial molecules in this study together with maternal characteristics (red line) for (A) all sPTB, (B) all spontaneous preterm labor with intact membranes (sPTL), (C) sPTL who delivered before 34 weeks of gestation, (D) all preterm prelabor rupture of membranes (PPROM), and (E) PPROM who delivered before 34 weeks of gestation. Area under the curve (AUC) values and 95% confidence intervals are given for each curve. P-values correspond to the comparisons between the curves of maternal characteristics alone and the curves of maternal characteristics together with all cytokines, chemokines, immune-related growth factors, and antimicrobial molecules within each study group.
-
Figure 7—source data 1
Comparison of AUC vs. AUPR statistics for vaginal immunoproteome predictive models of sPTB and subtypes.
AUC and AUPR calculations used preterm birth and related subgroups as the positive group while the reference (i.e., negative) group always constituted normal pregnancy group controls.
- https://cdn.elifesciences.org/articles/90943/elife-90943-fig7-data1-v1.xlsx
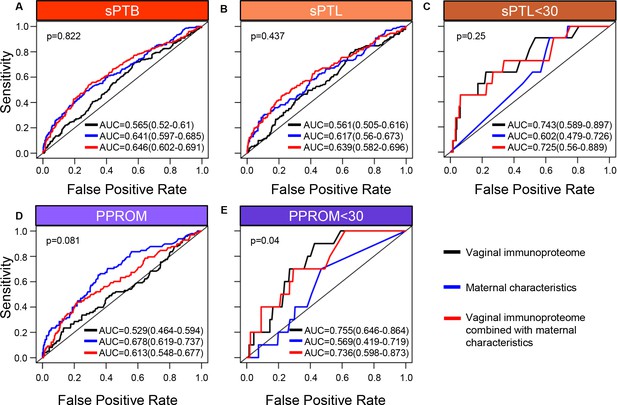
The vaginal immunoproteome shows moderate predictive value for early spontaneous preterm labor with intact membranes (sPTL) and preterm prelabor rupture of membranes (PPROM) using swabs collected before 24 weeks.
The vaginal immunoproteome allows for the prediction of early sPTB. Random forest modeling including protein concentrations generated from the last swab before 24 weeks of gestation was used to generate models using the combination of all cytokines, chemokines, immune-related growth factors, and antimicrobial molecules in this study (black line), maternal characteristics (blue line), or the combination of all cytokines, chemokines, immune-related growth factors, and antimicrobial molecules in this study together with maternal characteristics (red line) for (A) all spontaneous preterm births (sPTB), (B) all sPTL, (C) sPTL who delivered before 30 weeks of gestation, (D) all PPROM, and (E) PPROM who delivered before 30 weeks of gestation. Area under the curve (AUC) values and 95% confidence intervals are given for each curve.
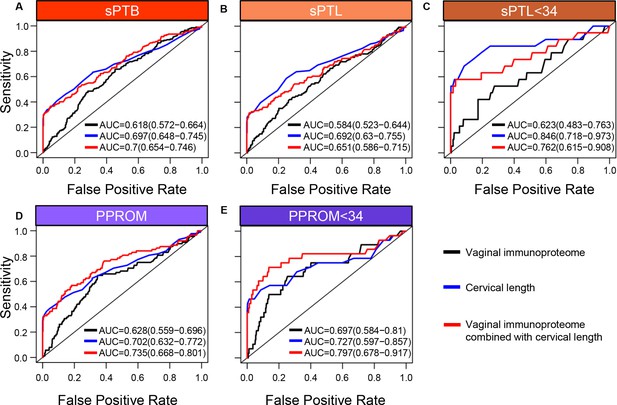
The vaginal immunoproteome provides increased value when combined with the quantitative cervical length measurement model for predicting early preterm prelabor rupture of membranes (PPROM).
The vaginal immunoproteome allows for the prediction of early spontaneous preterm births (sPTB). Random forest modeling including protein concentrations generated from the last swab before 28 weeks of gestation and cervical length measured during this time period was used to generate models using the combination of all cytokines, chemokines, immune-related growth factors, and antimicrobial molecules in this study (black line), quantitative cervical length measurements (blue line), or the combination of all cytokines, chemokines, immune-related growth factors, and antimicrobial molecules in this study together with cervical length measurements (red line) for (A) all sPTB, (B) all spontaneous preterm labor with intact membranes (sPTL), (C) sPTL who delivered before 34 weeks of gestation, (D) all PPROM, and (E) PPROM who delivered before 34 weeks of gestation. Area under the curve (AUC) values and 95% confidence intervals are given for each curve.
Tables
Demographics and clinical characteristics of the study groups.
Demographics and clinical information are presented as a median (with interquartile ranges) or as proportions (n/N).
Differences between study groups and the control group were assessed by the Mann–Whitney U test for continuous data or the Fisher’s exact test for categorical data.
| Term control(n = 494) | Spontaneous preterm birth (n = 245) | ||||
|---|---|---|---|---|---|
| sPTL (n = 140) | p | PPROM (n = 105) | p | ||
| Maternal age (years) | 24 (21–27) | 23.5 (21-27) | 0.37 | 25 (22–30) | 0.02 |
| BMI (kg/m2) | 27.5 (22.7–33.8) | 26.4 (22.5–31.7) | 0.05 | 28.2 (23.2–33.3) | 0.79 |
| Maternal race | 0.09 | 0.4 | |||
| African American | 94.5% (467/494) | 90% (126/140) | 98.1% (103/105) | ||
| White | 1.8% (9/494) | 5% (7/140) | 1% (1/105) | ||
| Other | 3.7 (18/494) | 5% (7/140) | 1% (1/105) | ||
| Nulliparity | 20.4% (101/494) | 12.9% (18/140) | 0.02 | 19% (20/105) | 0.79 |
| History of preterm birth | 11.1% (55/494) | 39.3% (55/140) | <0.001 | 32.4% (34/105) | <0.001 |
| Gestational age at delivery (weeks) | 39.6 (39–40.4) | 35.7 (33.7–36.6) | <0.001 | 35 (32.6–35.9) | <0.001 |
| Birthweight (g) | 3300 (3090–3593) | 2363 (1995–2748) | <0.001 | 2235 (1760–2575) | <0.001 |
| Maternal Inflammatory response | 0% (0/494) | 21.1% (28/133)* | <0.001 | 22.4% (22/98)* | <0.001 |
| Fetal inflammatory response | 4.3% (21/494) | 20.3% (27/133)* | <0.001 | 28.5% (28/98)* | <0.001 |
| Early sPTB (<34 weeks) | – | 27.1% (38/140) | 36.2% (38/105) | ||
| Late sPTB (34–36+6) weeks | – | 72.9% (102/140) | 63.8% (67/105) | ||
-
BMI = body mass index; sPTL = spontaneous preterm labor; sPTB = spontaneous preterm birth; PPROM = preterm prelabor rupture of membranes.
-
*
Seven missing data.
Immune mediator assay sensitivity and proportion outside of range of detection.
Vaginal immune mediator proportions below the limit of detection and greater than 2 * 99th percentile. Chemokines listed in red were excluded from analyses due to a majority of samples being below the limit of detection.
| Immune mediator | Sensitivity of detection | Control | sPTL | PPROM | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Below limit | Below limit % | Above limit | Above limit % | Below limit | Below limit % | Above limit | Above limit % | Below limit | Below limit % | Above limit | Above limit % | ||
| IFN-γ | 0.368 pg/mL | 515.00 | 27.01 | 7.00 | 0.37 | 103.00 | 19.77 | 1.00 | 0.19 | 83.00 | 21.23 | 1.00 | 0.26 |
| IL-1β | 0.152 pg/mL | 0.00 | 0.00 | 1.00 | 0.05 | 4.00 | 0.77 | 1.00 | 0.19 | 1.00 | 0.26 | 0.00 | 0.00 |
| IL-2 | 0.219 pg/mL | 29.00 | 1.52 | 2.00 | 0.10 | 10.00 | 1.92 | 1.00 | 0.19 | 6.00 | 1.53 | 0.00 | 0.00 |
| IL-4 | 0.028 pg/mL | 147.00 | 7.71 | 2.00 | 0.10 | 30.00 | 5.76 | 2.00 | 0.38 | 30.00 | 7.67 | 2.00 | 0.51 |
| IL-6 | 0.113 pg/mL | 43.00 | 2.25 | 0.00 | 0.00 | 10.00 | 1.92 | 2.00 | 0.38 | 8.00 | 2.05 | 3.00 | 0.77 |
| CXCL8 | 0.101 pg/mL | 0.00 | 0.00 | 0.00 | 0.00 | 4.00 | 0.77 | 1.00 | 0.19 | 0.00 | 0.00 | 0.00 | 0.00 |
| IL-10 | 0.054 pg/mL | 34.00 | 1.78 | 2.00 | 0.10 | 10.00 | 1.92 | 3.00 | 0.58 | 5.00 | 1.28 | 2.00 | 0.51 |
| IL-12p70 | 0.084 pg/mL | 178.00 | 9.33 | 0.00 | 0.00 | 35.00 | 6.72 | 1.00 | 0.19 | 42.00 | 10.74 | 0.00 | 0.00 |
| IL-13 | 0.119 pg/mL | 55.00 | 2.88 | 0.00 | 0.00 | 9.00 | 1.73 | 2.00 | 0.38 | 16.00 | 4.09 | 0.00 | 0.00 |
| TNF | 0.108 pg/mL | 94.00 | 4.93 | 2.00 | 0.10 | 14.00 | 2.69 | 4.00 | 0.77 | 23.00 | 5.88 | 2.00 | 0.51 |
| GM-CSF | 0.200 pg/mL | 176.00 | 9.23 | 4.00 | 0.21 | 46.00 | 8.83 | 2.00 | 0.38 | 30.00 | 7.67 | 2.00 | 0.51 |
| IL-1α | 0.089 pg/mL | 15.00 | 0.79 | 8.00 | 0.42 | 14.00 | 2.69 | 1.00 | 0.19 | 5.00 | 1.28 | 3.00 | 0.77 |
| IL-5 | 0.162 pg/mL | 324.00 | 16.99 | 4.00 | 0.21 | 102.00 | 19.58 | 3.00 | 0.58 | 82.00 | 20.97 | 1.00 | 0.26 |
| IL-7 | 0.124 pg/mL | 772.00 | 40.48 | 3.00 | 0.16 | 190.00 | 36.47 | 4.00 | 0.77 | 141.00 | 36.06 | 1.00 | 0.26 |
| IL-12/IL-23p40 | 0.408 pg/mL | 211.00 | 11.06 | 8.00 | 0.42 | 48.00 | 9.21 | 1.00 | 0.19 | 34.00 | 8.70 | 2.00 | 0.51 |
| IL-15 | 0.111 pg/mL | 707.00 | 37.07 | 4.00 | 0.21 | 159.00 | 30.52 | 1.00 | 0.19 | 142.00 | 36.32 | 6.00 | 1.53 |
| IL-16 | 0.478 pg/mL | 123.00 | 6.45 | 4.00 | 0.21 | 31.00 | 5.95 | 1.00 | 0.19 | 26.00 | 6.65 | 1.00 | 0.26 |
| IL-17A | 0.381 pg/mL | 247.00 | 12.95 | 10.00 | 0.52 | 42.00 | 8.06 | 4.00 | 0.77 | 46.00 | 11.76 | 4.00 | 1.02 |
| LT-α | 0.095 pg/mL | 957.00 | 50.18 | 4.00 | 0.21 | 236.00 | 45.30 | 3.00 | 0.58 | 201.00 | 51.41 | 0.00 | 0.00 |
| VEGF | 0.264 pg/mL | 7.00 | 0.37 | 2.00 | 0.10 | 9.00 | 1.73 | 2.00 | 0.38 | 12.00 | 3.07 | 1.00 | 0.26 |
| CCL11/Eotaxin | 0.480 pg/mL | 1504.00 | 78.87 | 0.00 | 0.00 | 379.00 | 72.74 | 0.00 | 0.00 | 294.00 | 75.19 | 1.00 | 0.26 |
| CCL26/Eotaxin-3 | 1.099 pg/mL | 1480.00 | 77.61 | 7.00 | 0.37 | 394.00 | 75.62 | 3.00 | 0.58 | 309.00 | 79.03 | 0.00 | 0.00 |
| CXCL8 (HA) | 22.575 pg/mL | 84.00 | 4.40 | 0.00 | 0.00 | 11.00 | 2.11 | 1.00 | 0.19 | 23.00 | 5.88 | 0.00 | 0.00 |
| CXCL10 | 0.119 pg/mL | 4.00 | 0.21 | 2.00 | 0.10 | 2.00 | 0.38 | 2.00 | 0.38 | 0.00 | 0.00 | 0.00 | 0.00 |
| CCL2 | 0.072 pg/mL | 10.00 | 0.52 | 2.00 | 0.10 | 4.00 | 0.77 | 2.00 | 0.38 | 0.00 | 0.00 | 4.00 | 1.02 |
| CCL13/MCP-4 | 0.230 pg/mL | 1693.00 | 88.78 | 2.00 | 0.10 | 438.00 | 84.07 | 7.00 | 1.34 | 332.00 | 84.91 | 5.00 | 1.28 |
| CCL22/MDC | 1.740 pg/mL | 985.00 | 51.65 | 3.00 | 0.16 | 245.00 | 47.02 | 2.00 | 0.38 | 197.00 | 50.38 | 0.00 | 0.00 |
| CCL3 | 0.319 pg/mL | 718.00 | 37.65 | 2.00 | 0.10 | 134.00 | 25.72 | 2.00 | 0.38 | 116.00 | 29.67 | 2.00 | 0.51 |
| CCL4 | 0.226 pg/mL | 221.00 | 11.59 | 2.00 | 0.10 | 33.00 | 6.33 | 2.00 | 0.38 | 32.00 | 8.18 | 2.00 | 0.51 |
| CCL17 | 0.375 pg/mL | 192.00 | 10.07 | 0.00 | 0.00 | 45.00 | 8.64 | 2.00 | 0.38 | 38.00 | 9.72 | 0.00 | 0.00 |
| SLPI | 20.336 pg/mL | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| β-defensin-2 | 0.007 ng/mL | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
-
sPTL = spontaneous preterm labor; PPROM = preterm prelabor rupture of membranes; HA = high affinity.





