Disentangling the relationship between cancer mortality and COVID-19 in the US
Figures
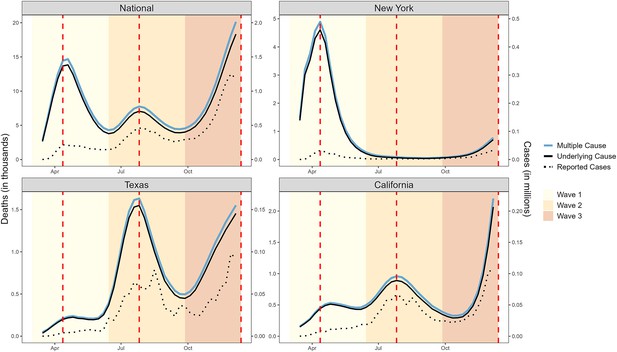
Weekly counts of death certificates listing COVID-19 as either the underlying or a multiple cause.
When included on a death certificate, COVID-19 was most often listed as the underlying cause of death rather than a contributing cause. National-level data reveal three distinct waves: Wave 1 (spring, March 1 to June 27, 2020), Wave 2 (summer, June 28 to October 3, 2020), and Wave 3 (winter, October 4 to December 6, 2020, incomplete). Vertical dashed lines represent the peak of each wave, dotted lines represent the number of reported cases (y-axis on the right). New York experienced its first large COVID-19 wave in Wave 1, while Texas had its first large wave in Wave 2 and California did not experience a large wave until Wave 3 which had not yet peaked at the end of 2020.
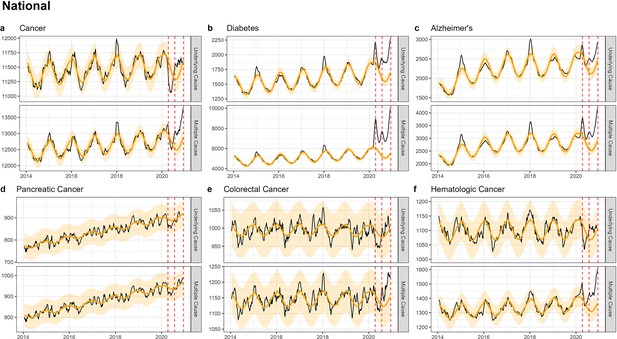
National-level weekly observed and estimated baseline mortality for each diagnosis group (Cancer (a), Diabetes (b), Alzheimer’s (c), Pancreatic Cancer (d), Colorectal Cancer (e), Hematologic Cancer (f)) as both the underlying cause or anywhere on the death certificate (multiple cause) from 2014 to 2020.
Red dashed lines represent the timing of the peaks for the three COVID-19 waves in 2020. Baselines during the pandemic are projected based on the previous years of data.
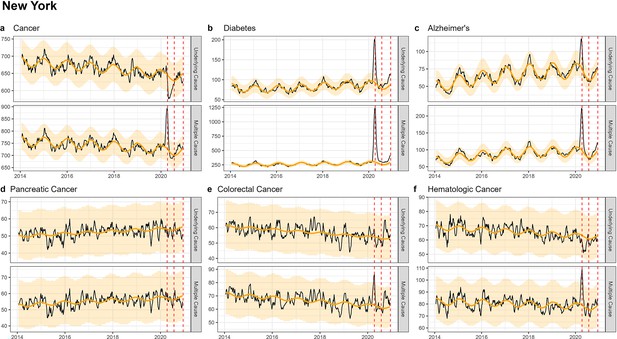
Weekly observed and estimated baseline mortality for each diagnosis group (Cancer (a), Diabetes (b), Alzheimer’s (c), Pancreatic Cancer (d), Colorectal Cancer (e), Hematologic Cancer (f)) as both the underlying cause or anywhere on the death certificate (multiple cause) from 2014 to 2020 in New York.
Red dashed lines represent the timing of the peaks for the three COVID-19 waves in 2020. New York experienced its first large wave of COVID-19 in spring 2020 (Wave 1).
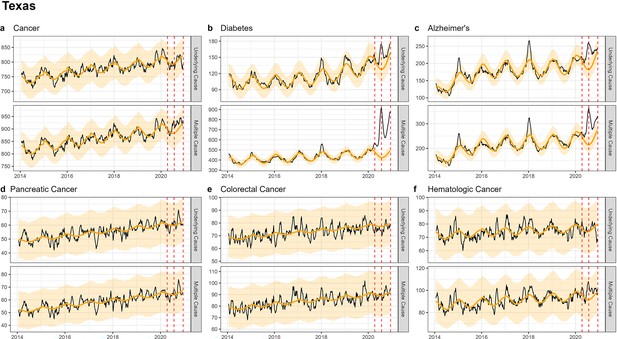
Weekly observed and estimated baseline mortality for each diagnosis group (Cancer (a), Diabetes (b), Alzheimer’s (c), Pancreatic Cancer (d), Colorectal Cancer (e), Hematologic Cancer (f)) as both the underlying cause or anywhere on the death certificate (multiple cause) from 2014 to 2020 in Texas.
Red dashed lines represent the timing of the peaks for the three COVID-19 waves in 2020. Texas experienced its first large wave of COVID-19 in the summer of 2020 (Wave 2).
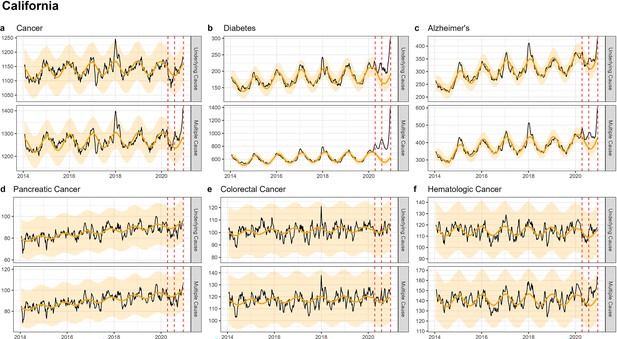
Weekly observed and estimated baseline mortality for each diagnosis group (Cancer (a), Diabetes (b), Alzheimer’s (c), Pancreatic Cancer (d), Colorectal Cancer (e), Hematologic Cancer (f)) as both the underlying cause or anywhere on the death certificate (multiple cause) from 2014 to 2020 in California.
Red dashed lines represent the timing of the peaks for the three COVID-19 waves in 2020. California did not experience a large wave of COVID-19 until the winter of 2020–2021 (Wave 3), only the first half of which is captured here.
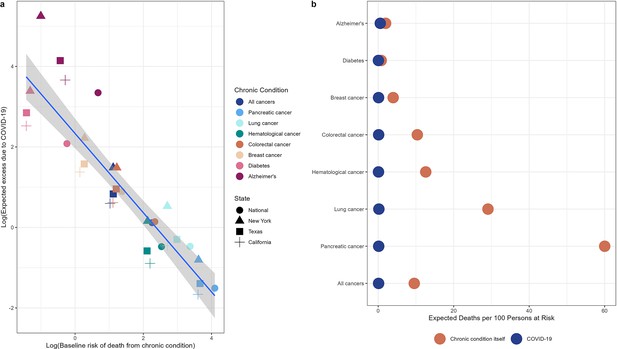
Illustration of competing risks.
Based on our demographic model, we expect a small increase in cancer mortality relative to diabetes and Alzheimer’s due to the higher competing risk of death from cancer compared to COVID-19. Panel (a) shows the log of the baseline mortality rate (based on observed mortality in 2019) from each condition on the x-axis and the log of the expected excess mortality (elevation over baseline) on the y-axis. Chronic conditions are shown in colors while states are shown in different shapes. Pancreatic cancer, the deadliest cancer considered, is on the bottom right (highest baseline mortality, lowest expected excess) while diabetes and Alzheimer’s are on the top left (lowest baseline mortality, highest expected excess). Panel (b) shows the baseline number of deaths per 100 persons at risk for each condition expected from March to December 2020 (based on deaths over this same period in 2019, orange dots) compared to the expected number of deaths due to COVID-19 under the null hypothesis (blue dots). The null hypothesis stipulates that there is no biological association between any of these chronic diseases and COVID-19. For diabetes and Alzheimer’s, the baseline risks of death are similar to the risk of death from COVID-19, while risk of death from cancer outcompetes risk of COVID-19 death for all types of cancer.
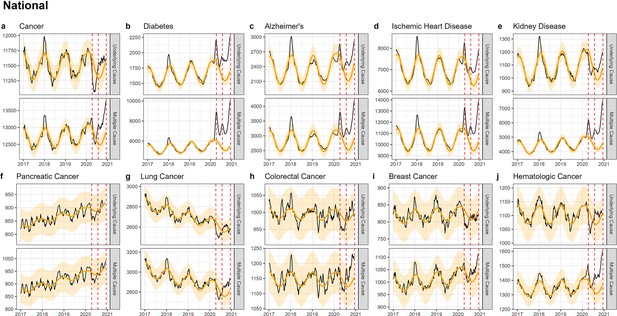
National-level weekly observed and estimated baseline mortality for each diagnosis group (Cancer (a), Diabetes (b), Alzheimer’s (c), Ischemic Heart Disease (d), Kidney Disease (e), Pancreatic Cancer (f), Lung Cancer (g), Colorectal Cancer (h), Breast Cancer (i), Hematologica Cancer (j)) as both the underlying cause or anywhere on the death certificate (multiple cause) from 2017 to 2020.
Red dashed lines represent the timing of the peaks for the three COVID-19 waves in 2020. Baselines during the pandemic are projected based on the previous years of data.
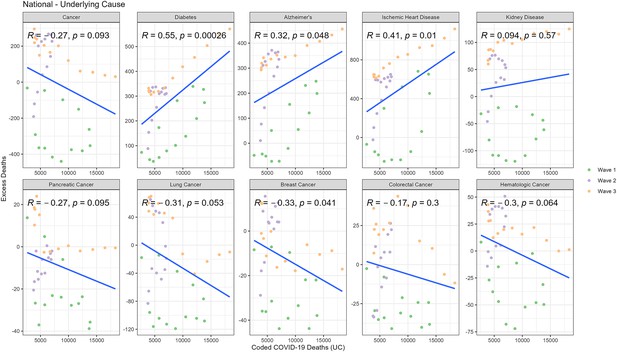
Correlation between weekly number of COVID-19-coded deaths and excess underlying deaths for each diagnosis group (National).
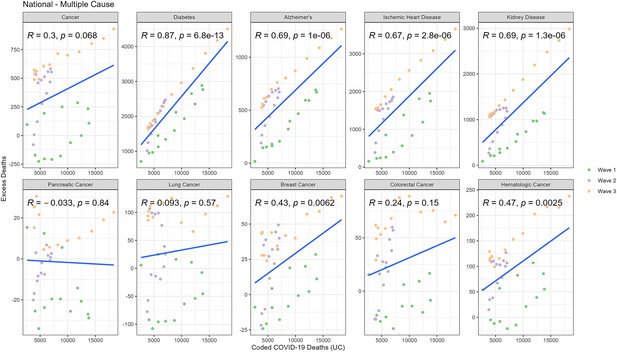
Correlation between weekly number of COVID-19-coded deaths and excess multiple cause deaths for each diagnosis group (National).
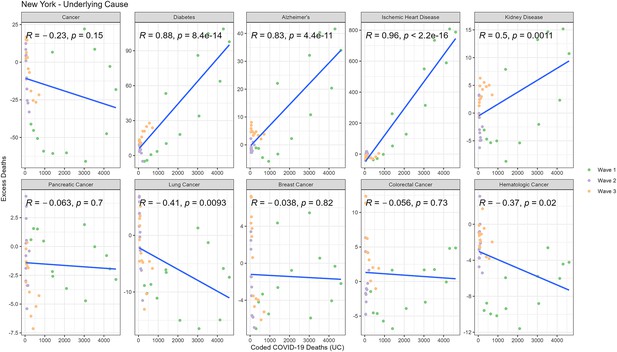
Correlation between weekly number of COVID-19-coded deaths and excess underlying deaths for each diagnosis group (New York).
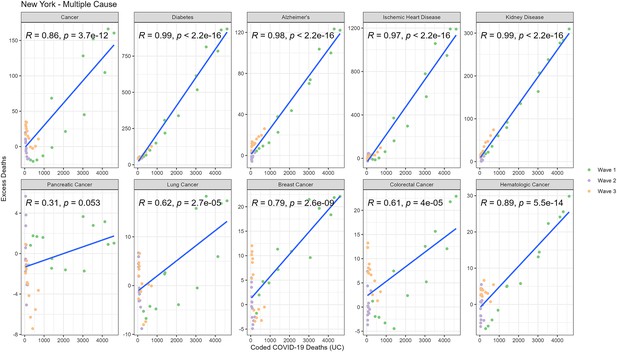
Correlation between weekly number of COVID-19-coded deaths and excess underlying deaths for each diagnosis group (New York).
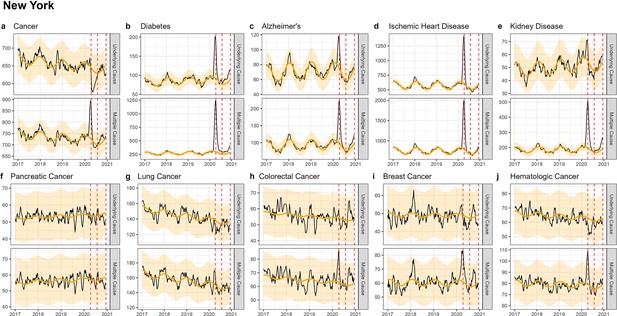
Weekly observed and estimated baseline mortality for each diagnosis group (Cancer (a), Diabetes (b), Alzheimer’s (c), Ischemic Heart Disease (d), Kidney Disease (e), Pancreatic Cancer (f), Lung Cancer (g), Colorectal Cancer (h), Breast Cancer (i), Hematologica Cancer (j)) as both the underlying cause or anywhere on the death certificate (multiple cause) from 2017 to 2020 in New York.
Red dashed lines represent the timing of the peaks for the three COVID-19 waves in 2020. Baselines during the pandemic are projected based on the previous years of data.
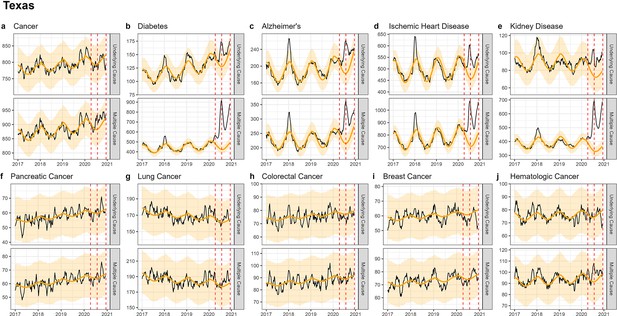
Weekly observed and estimated baseline mortality for each diagnosis group (Cancer (a), Diabetes (b), Alzheimer’s (c), Ischemic Heart Disease (d), Kidney Disease (e), Pancreatic Cancer (f), Lung Cancer (g), Colorectal Cancer (h), Breast Cancer (i), Hematologica Cancer (j)) as both the underlying cause or anywhere on the death certificate (multiple cause) from 2017 to 2020 in Texas.
Red dashed lines represent the timing of the peaks for the three COVID-19 waves in 2020. Baselines during the pandemic are projected based on the previous years of data.
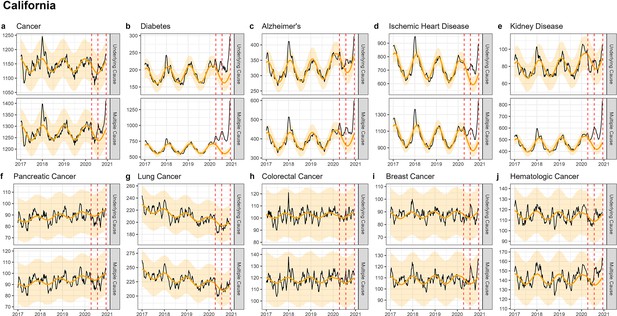
Weekly observed and estimated baseline mortality for each diagnosis group (Cancer (a), Diabetes (b), Alzheimer’s (c), Ischemic Heart Disease (d), Kidney Disease (e), Pancreatic Cancer (f), Lung Cancer (g), Colorectal Cancer (h), Breast Cancer (i), Hematologica Cancer (j)) as both the underlying cause or anywhere on the death certificate (multiple cause) from 2017 to 2020 in New York.
Red dashed lines represent the timing of the peaks for the three COVID-19 waves in 2020. Baselines during the pandemic are projected based on the previous years of data.
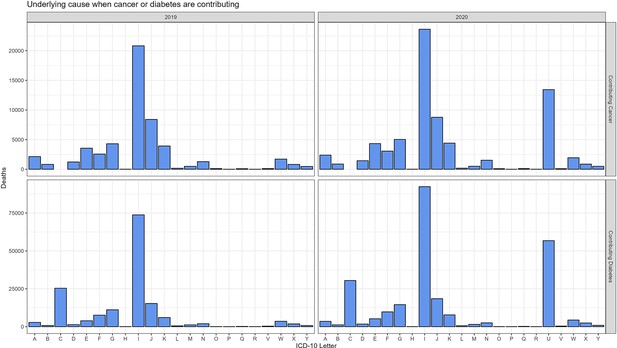
Comparison of ICD-10 letter categories between 2020 and 2019 for the underlying cause (UC) of death when cancer or diabetes are included on the death certificate, but are not listed as the UC of death.
For both cancer and diabetes, I codes (diseases of the circulatory system) make up the majority of underlying deaths. The most notable difference between 2019 and 2020 is the increase in U codes, which includes COVID-19 (U071). In total there were 13,434 deaths ascribed to COVID-19 (UC deaths) among cancer multiple cause (MC) deaths. COVID-19 was included in <3% of all cancer deaths and 17% of diabetes deaths. In both cases it was listed as the UC on the majority of death certificates where it was included (81% and 97% for cancer and diabetes, respectively).
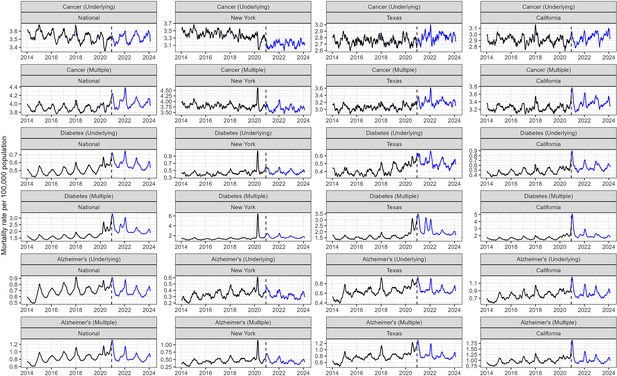
Post-2020 trends in cancer, diabetes, and Alzheimer’s mortality.
Aggregated weekly data was downloaded from CDC Wonder. Trends in cancer mortality rate appear stable in the national data and in Texas and California, but decreasing in New York. The diabetes mortality rate is higher post-2020 compared to earlier years across all states. Alzheimer’s appears stable and slowly decreasing.
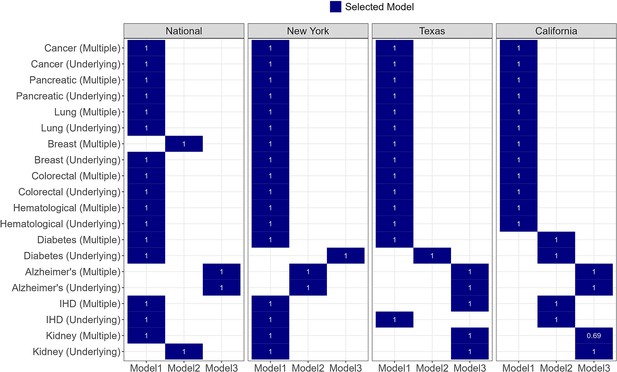
For each condition three time series models with different time trends were considered (see Materials and methods).
The final model for each condition and location is indicated in blue. The final model was fit to 2014–2018 data only and used to predict the 2019 data. A coverage proportion (shown in white) was calculated as the proportion of observed 2019 data that fell within the projection intervals of the model. For all causes of death and states (except multiple cause [MC] kidney disease in California) the coverage proportion was 1, indicating that all data points fell within the prediction intervals.
Tables
Each diagnosis group and its corresponding ICD-10 codes, number of underlying deaths, mean age in years at time of death, the percentage of deaths occurring at home, and the percentage of deaths occurring in nursing homes for 2019 and 2020.
| Year | Diagnosis group | ICD-10 codes | No. deaths | Mean age, years (IQR) | %Home/ER | %Nursing home |
|---|---|---|---|---|---|---|
| 2019 | Cancer | C00-C99 | 493,397 | 72 (64–81) | 45 | 12 |
| Pancreatic cancer | C25 | 37,864 | 72 (64–80) | 51 | 9 | |
| Colorectal cancer | C18-C20 | 42,484 | 71 (61–82) | 46 | 13 | |
| Hematological cancers | C81-C96 | 47,174 | 74 (67–84) | 35 | 11 | |
| Diabetes | E10-E14 | 70,763 | 72 (63–82) | 53 | 17 | |
| Alzheimer’s | G30 | 98,675 | 87 (82–92) | 29 | 50 | |
| 2020 | Cancer | C00-C99 | 513,275 | 72 (64–81) | 55 | 8 |
| Pancreatic cancer | C25 | 39,893 | 72 (65–80) | 61 | 6 | |
| Colorectal cancer | C18-C20 | 43,990 | 71 (61–82) | 56 | 9 | |
| Hematological cancers | C81-C96 | 49,161 | 74 (67–84) | 46 | 8 | |
| Diabetes | E10-E14 | 88,124 | 71 (62–82) | 58 | 15 | |
| Alzheimer’s | G30 | 115,256 | 86 (82–92) | 33 | 46 |
The estimated number of excess deaths and the percentage over baseline for each diagnosis group when listed as both the underlying cause or anywhere on the death certificate (multiple cause).
Estimates for the national-level data are provided for the full pandemic period and for each state based on when the first large wave was experienced.
| Cause of death | State | Wave | Multiple cause | Underlying cause | ||
|---|---|---|---|---|---|---|
| Excess deaths | % Over baseline | Excess deaths | % Over baseline | |||
| Cancer | National | Overall | 13601* | 3.0 | 11 | 0.0 |
| New York | 1 | 747 | 6.0 | –474 | –5.0 | |
| Texas | 2 | 467 | 4.0 | 39 | 0.0 | |
| California | 3 | 529 | 4.0 | 82 | 1.0 | |
| Pancreatic cancer | National | Overall | –25 | –0.0 | –282 | –1.0 |
| New York | 1 | 8 | 1.0 | –16 | –2.0 | |
| Texas | 2 | 17 | 2.0 | 24 | 3.0 | |
| California | 3 | 0 | 0.0 | –18 | –2.0 | |
| Colorectal cancer | National | Overall | 988 | 2.0 | –168 | –0.0 |
| New York | 1 | 91 | 9.0 | –16 | –2.0 | |
| Texas | 2 | 4 | 0.0 | –34 | –3.0 | |
| California | 3 | 27 | 2.0 | –1 | –0.0 | |
| Hematological cancers | National | Overall | 3615* | 7.0 | 111 | 0.0 |
| New York | 1 | 121 | 10.0 | –107 | –11.0 | |
| Texas | 2 | 136 | 11.0 | 21 | 2.0 | |
| California | 3 | 114 | 8.0 | 20 | 2.0 | |
| Diabetes | National | Overall | 82,318* | 37.0 | 10,784* | 16.0 |
| New York | 1 | 5945* | 128.0 | 568* | 40.0 | |
| Texas | 2 | 4612* | 77.0 | 420* | 23.0 | |
| California | 3 | 3474* | 59.0 | 575* | 33.0 | |
| Alzheimer’s | National | Overall | 21,712* | 19.0 | 8528* | 9.0 |
| New York | 1 | 734* | 49.0 | 188 | 16.0 | |
| Texas | 2 | 1398* | 45.0 | 805* | 31.0 | |
| California | 3 | 726* | 18.0 | 259 | 8.0 | |
-
*
Confidence interval does not include zero.
Projections of COVID-19-related excess mortality patterns for different cancers and chronic conditions in the US, under different hypotheses for the association between the condition and COVID-19.
Projections are provided for the null hypothesis of no biological interaction between the condition and COVID-19; these projections are solely driven by the size and mean age of the population living with each condition (where age determines the infection-fatality ratio from COVID-19), and the baseline risk of death from the condition over a similar time period (March to December 2019 for the national data, and for the states comparable dates in 2019 corresponding to the relevant COVID-19 wave). Additional projections are provided under alternative hypotheses, where each condition is associated with a relative risk (RR) of 2 or 5 for COVID-19-related death (infection-fatality ratio multiplied by 2 or 5).
| Chronic condition | State | Population-at-risk | Mean age | Wave | Observed MC deaths over same period in 2019 | Observed excess(% over baseline) in 2020 | Expected excess (null) | Expected excess (RR = 2) | Expected excess (RR = 5) |
|---|---|---|---|---|---|---|---|---|---|
| All cancers | National | 5,718,925 | 65 | Overall | 546,453 | 3 (1–4) | 1 (1–2) | 2 (1–4) | 6 (4–10) |
| New York | 400,891 | 65 | Wave 1 | 12,244 | 6 (−1 to 15) | 4 (2–10) | 9 (3–20) | 22 (8–51) | |
| Texas | 397,993 | 63 | Wave 2 | 12,187 | 4 (−3 to 11) | 2 (1–6) | 5 (2–12) | 11 (4–29) | |
| California | 599,552 | 64 | Wave 3 | 16,713 | 4 (−1 to 10) | 2 (0–5) | 4 (1–9) | 9 (2–23) | |
| Pancreatic | National | 66,319 | 67 | Overall | 39,798 | 0 (−6 to 7) | 0 (0–0) | 0 (0–1) | 1 (1–2) |
| New York | 2584 | 67 | Wave 1 | 963 | 1 (−21 to 35) | 0 (0–1) | 1 (0–2) | 2 (1–5) | |
| Texas | 2264 | 66 | Wave 2 | 882 | 2 (−19 to 34) | 0 (0–1) | 0 (0–1) | 1 (0–3) | |
| California | 3482 | 67 | Wave 3 | 1277 | 0 (−17 to 24) | 0 (0–0) | 0 (0–1) | 1 (0–2) | |
| Lung cancer | National | 425,015 | 70 | Overall | 123,622 | 1 (−3 to 5) | 1 (0–1) | 1 (1–2) | 3 (2–5) |
| New York | 17,709 | 71 | Wave 1 | 2643 | 1 (−13 to 20) | 2 (1–4) | 3 (1–8) | 8 (3–20) | |
| Texas | 12,700 | 70 | Wave 2 | 2513 | 2 (−11 to 20) | 1 (0–2) | 1 (1–4) | 4 (1–9) | |
| California | 19,079 | 70 | Wave 3 | 2861 | 3 (−10 to 18) | 1 (0–2) | 1 (0–3) | 3 (1–8) | |
| Hematological | National | 459,463 | 62 | Overall | 57,892 | 7 (1–13) | 1 (0–1) | 1 (1–2) | 3 (2–5) |
| New York | 15,577 | 62 | Wave 1 | 1305 | 10 (−11 to 40) | 1 (0–3) | 2 (1–5) | 6 (2–13) | |
| Texas | 14,927 | 59 | Wave 2 | 1231 | 11 (−9 to 38) | 1 (0–1) | 1 (0–3) | 3 (1–7) | |
| California | 21,290 | 61 | Wave 3 | 1916 | 8 (−8 to 29) | 0 (0–1) | 1 (0–2) | 2 (1–5) | |
| Colorectal | National | 473,264 | 66 | Overall | 49,053 | 2 (−4 to 8) | 1 (1–2) | 2 (1–4) | 6 (4–10) |
| New York | 30,859 | 66 | Wave 1 | 1048 | 9 (−13 to 44) | 4 (2–10) | 9 (3–20) | 22 (8–51) | |
| Texas | 36,641 | 65 | Wave 2 | 1224 | 0 (−18 to 26) | 3 (1–7) | 5 (2–13) | 13 (4–33) | |
| California | 51,863 | 65 | Wave 3 | 1575 | 2 (−14 to 24) | 2 (1–5) | 4 (1–10) | 9 (3–24) | |
| Breast | National | 1,097,917 | 64 | Overall | 43,519 | 2 (−4 to 9) | 2 (2–4) | 5 (3–8) | 12 (8–21) |
| New York | 74,459 | 64 | Wave 1 | 981 | 16 (−8 to 53) | 9 (3–21) | 18 (7–42) | 46 (17–106) | |
| Texas | 77,860 | 62 | Wave 2 | 1019 | 3 (−17 to 32) | 5 (2–12) | 10 (3–24) | 24 (8–61) | |
| California | 123,433 | 63 | Wave 3 | 1421 | 2 (−15 to 25) | 4 (1–10) | 8 (2–20) | 20 (5–51) | |
| Diabetes | National | 29,105,146 | 60 | Overall | 229,326 | 37 (31–43) | 8 (5–14) | 16 (10–28) | 40 (26–69) |
| New York | 1,792,926 | 60 | Wave 1 | 4804 | 128 (104–158) | 30 (11–68) | 59 (22–136) | 148 (55–340) | |
| Texas | 2,450,005 | 58 | Wave 2 | 5898 | 77 (61–96) | 17 (6–44) | 35 (12–87) | 86 (30–218) | |
| California | 3514,440 | 59 | Wave 3 | 8399 | 59 (47–74) | 12 (3–32) | 25 (7–64) | 62 (17–160) | |
| Alzheimer’s | National | 6,070,000 | 81 | Overall | 118,993 | 19 (11–28) | 28 (18–48) | 57 (36–96) | 142 (90–240) |
| New York | 426,500 | 81 | Wave 1 | 1563 | 49 (23–87) | 191 (70–432) | 381 (140–863) | 953 (350–2158) | |
| Texas | 459,300 | 80 | Wave 2 | 2974 | 45 (27–69) | 63 (21–158) | 126 (43–315) | 315 (107–788) | |
| California | 719,700 | 81 | Wave 3 | 5394 | 18 (6–33) | 39 (11–98) | 78 (21–196) | 195 (53–491) |
Diagnosis groups and corresponding ICD-10 codes, number of underlying and multiple cause deaths, mean age in years at time of death, the percentage of deaths occurring at home, and the percentage of deaths occurring in nursing homes for 2019 and 2020.
| Underlying cause | Multiple cause | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Year | Diagnosis group | ICD-10 codes | No. deaths | Mean age, years (IQR) | %Home/ER | %Nursing home | No. deaths | Mean age, years (IQR) | %Home/ER | %Nursing home |
| 2019 | Cancer | C00-C99 | 493,397 | 72 (64–81) | 45 | 12 | 546,453 | 72 (64–82) | 44 | 13 |
| Pancreatic cancer | C25 | 37,864 | 72 (64–80) | 51 | 9 | 39,798 | 72 (64–80) | 50 | 9 | |
| Lung cancer | C34 | 114,552 | 72 (65–80) | 45 | 12 | 123,622 | 72 (65–80) | 44 | 12 | |
| Colorectal cancer | C18-C20 | 42,484 | 71 (61–82) | 46 | 13 | 49,053 | 72 (62–83) | 45 | 14 | |
| Breast cancer | C50 | 35,115 | 69 (59–81) | 44 | 13 | 43,519 | 71 (61–83) | 43 | 15 | |
| Hematological cancer | C81-C96 | 47,174 | 74 (67–84) | 35 | 11 | 57,892 | 74 (67–84) | 35 | 12 | |
| Diabetes | E10-E14 | 70,763 | 72 (63–82) | 53 | 17 | 229,326 | 74 (65–84) | 46 | 19 | |
| Alzheimer’s | G30 | 98,675 | 87 (82–92) | 29 | 50 | 118,993 | 87 (82–92) | 29 | 48 | |
| Ischemic heart disease | I20-I25 | 292,659 | 77 (67–88) | 50 | 18 | 440,225 | 77 (68–87) | 47 | 18 | |
| Kidney disease | N00-07, 17–19,25-28 | 46,120 | 76 (68–87) | 25 | 18 | 189,938 | 76 (67–87) | 20 | 15 | |
| 2020 | Cancer | C00-C99 | 513,275 | 72 (64–81) | 55 | 8 | 586,503 | 72 (64–82) | 52 | 9 |
| Pancreatic cancer | C25 | 39,893 | 72 (65–80) | 61 | 6 | 42,383 | 72 (65–80) | 60 | 6 | |
| Lung cancer | C34 | 115,554 | 72 (65–80) | 54 | 8 | 127,671 | 72 (65–80) | 53 | 8 | |
| Colorectal cancer | C18-C20 | 43,990 | 71 (61–82) | 56 | 9 | 52,319 | 72 (62–83) | 53 | 10 | |
| Breast cancer | C50 | 36,296 | 70 (60–81) | 54 | 10 | 47,094 | 72 (62–83) | 51 | 12 | |
| Hematological cancer | C81-C96 | 49,161 | 74 (67–84) | 46 | 8 | 64,840 | 74 (68–84) | 43 | 9 | |
| Diabetes | E10-E14 | 88,124 | 71 (62–82) | 58 | 15 | 343,061 | 73 (65–83) | 45 | 16 | |
| Alzheimer’s | G30 | 115,256 | 86 (82–92) | 33 | 46 | 151,206 | 86 (82–92) | 31 | 47 | |
| Ischemic heart disease | I20-I25 | 327,854 | 76 (67–88) | 54 | 16 | 533,204 | 77 (68–87) | 49 | 16 | |
| Kidney disease | N00-07, 17–19,25-28 | 49,796 | 76 (68–87) | 30 | 15 | 255,708 | 75 (67–86) | 21 | 12 | |
Estimated Excess Deaths by Cause and Wave (National).
Estimated number of excess deaths and the percentage over baseline for each diagnosis group (National). Estimates are aggregated over all of 2020 and for each COVID-19 wave during 2020.
| Cause of death | Wave | Multiple cause | Underlying cause | ||
|---|---|---|---|---|---|
| Excess deaths | % Over baseline | Excess deaths | % Over baseline | ||
| Cancer | Overall | 13,601* | 3.0 | 11 | 0.0 |
| 1 | 79 | 0.0 | –3917* | –2.0 | |
| 2 | 6519* | 4.0 | 2662 | 2.0 | |
| 3 | 7003* | 6.0 | 1266 | 1.0 | |
| Pancreatic cancer | Overall | –25 | –0.0 | –282 | –1.0 |
| 1 | –213 | –1.0 | –281 | –2.0 | |
| 2 | 44 | 0.0 | –30 | –0.0 | |
| 3 | 144 | 1.0 | 29 | 0.0 | |
| Lung cancer | Overall | 1102 | 1.0 | –814 | –1.0 |
| 1 | –729 | –1.0 | –1221 | –3.0 | |
| 2 | 784 | 2.0 | 249 | 1.0 | |
| 3 | 1047 | 4.0 | 158 | 1.0 | |
| Breast cancer | Overall | 838 | 2.0 | –438 | –1.0 |
| 1 | –66 | –0.0 | –415 | –3.0 | |
| 2 | 437 | 3.0 | 81 | 1.0 | |
| 3 | 467 | 5.0 | –105 | –1.0 | |
| Colorectal cancer | Overall | 988 | 2.0 | –168 | –0.0 |
| 1 | –169 | –1.0 | –463 | –3.0 | |
| 2 | 454 | 3.0 | 112 | 1.0 | |
| 3 | 703* | 6.0 | 183 | 2.0 | |
| Hematological cancers | Overall | 3615* | 7.0 | 111 | 0.0 |
| 1 | 546 | 2.0 | –447 | –2.0 | |
| 2 | 1412* | 8.0 | 412 | 3.0 | |
| 3 | 1657* | 12.0 | 146 | 1.0 | |
| Diabetes | Overall | 82,318* | 37.0 | 10,784* | 16.0 |
| 1 | 25,306* | 25.0 | 2305* | 7.0 | |
| 2 | 27,534* | 38.0 | 4330* | 20.0 | |
| 3 | 29,477* | 56.0 | 4148* | 26.0 | |
| Alzheimer’s | Overall | 21,712* | 19.0 | 8528* | 9.0 |
| 1 | 4763* | 9.0 | 547 | 1.0 | |
| 2 | 8054* | 22.0 | 4257* | 14.0 | |
| 3 | 8894* | 33.0 | 3724* | 16.0 | |
| Ischemic heart disease | Overall | 58,793* | 14.0 | 17,194* | 6.0 |
| 1 | 12,042* | 6.0 | 862 | 1.0 | |
| 2 | 21,783* | 16.0 | 7912* | 9.0 | |
| 3 | 24,967* | 25.0 | 8419* | 13.0 | |
| Kidney disease | Overall | 41,907* | 22.0 | 785 | 2.0 |
| 1 | 8182* | 10.0 | –1048 | –5.0 | |
| 2 | 14,767* | 25.0 | 777 | 5.0 | |
| 3 | 18,958* | 44.0 | 1056* | 10.0 | |
-
*
Confidence interval does not include zero.
Estimated Excess Deaths by Cause and Wave (New York).
Estimated number of excess deaths and the percentage over baseline for each diagnosis group (New York). Estimates are aggregated over all of 2020 and for each COVID-19 wave during 2020.
| Cause of death | Wave | Multiple cause | Underlying cause | ||
|---|---|---|---|---|---|
| Excess deaths | % Over baseline | Excess deaths | % Over baseline | ||
| Cancer | Overall | 1012 | 4.0 | –557 | –2.0 |
| 1 | 747 | 6.0 | –474 | –5.0 | |
| 2 | 120 | 1.0 | -6 | –0.0 | |
| 3 | 144 | 2.0 | –77 | –1.0 | |
| Pancreatic cancer | Overall | –29 | –1.0 | –58 | –3.0 |
| 1 | 8 | 1.0 | –16 | –2.0 | |
| 2 | -1 | –0.0 | -9 | –1.0 | |
| 3 | –37 | –6.0 | –33 | –6.0 | |
| Lung cancer | Overall | 47 | 1.0 | –163 | –3.0 |
| 1 | 27 | 1.0 | –143 | –7.0 | |
| 2 | 23 | 1.0 | 16 | 1.0 | |
| 3 | -3 | –0.0 | –36 | –3.0 | |
| Breast cancer | Overall | 205 | 9.0 | –46 | –2.0 |
| 1 | 151 | 16.0 | –34 | –4.0 | |
| 2 | 31 | 4.0 | 3 | 0.0 | |
| 3 | 23 | 4.0 | –15 | –3.0 | |
| Colorectal cancer | Overall | 189 | 8.0 | 42 | 2.0 |
| 1 | 91 | 9.0 | –16 | –2.0 | |
| 2 | 40 | 5.0 | 26 | 4.0 | |
| 3 | 58 | 9.0 | 33 | 6.0 | |
| Hematological cancers | Overall | 156 | 5.0 | –149 | –6.0 |
| 1 | 121 | 10.0 | –107 | –11.0 | |
| 2 | 1 | 0.0 | –25 | –3.0 | |
| 3 | 35 | 5.0 | –18 | –3.0 | |
| Diabetes | Overall | 7240* | 66.0 | 866* | 26.0 |
| 1 | 5945* | 128.0 | 568* | 40.0 | |
| 2 | 631* | 18.0 | 121 | 11.0 | |
| 3 | 664* | 24.0 | 177 | 21.0 | |
| Alzheimer’s | Overall | 884* | 26.0 | 233 | 9.0 |
| 1 | 734* | 49.0 | 188 | 16.0 | |
| 2 | 1 | 0.0 | 1 | 0.0 | |
| 3 | 150 | 17.0 | 44 | 6.0 | |
| Ischemic heart disease | Overall | 7118* | 25.0 | 3756* | 17.0 |
| 1 | 6607* | 54.0 | 4092* | 44.0 | |
| 2 | 179 | 2.0 | –184 | –3.0 | |
| 3 | 331 | 5.0 | –152 | –3.0 | |
| Kidney disease | Overall | 2438* | 34.0 | 51 | 3.0 |
| 1 | 1946* | 63.0 | 22 | 3.0 | |
| 2 | 144 | 6.0 | –13 | –2.0 | |
| 3 | 349* | 19.0 | 42 | 8.0 | |
-
*
Confidence interval does not include zero.
Estimated Excess Deaths by Cause and Wave (Texas).
Estimated number of excess deaths and the percentage over baseline for each diagnosis group (Texas). Estimates are aggregated over all of 2020 and for each COVID-19 wave during 2020.
| Cause of death | Wave | Multiple cause | Underlying cause | ||
|---|---|---|---|---|---|
| Excess deaths | % Over baseline | Excess deaths | % Over baseline | ||
| Cancer | Overall | 602 | 2.0 | –130 | –0.0 |
| 1 | –48 | –0.0 | –62 | –0.0 | |
| 2 | 467 | 4.0 | 39 | 0.0 | |
| 3 | 183 | 2.0 | –107 | –1.0 | |
| Pancreatic cancer | Overall | 1 | 0.0 | 5 | 0.0 |
| 1 | –36 | –3.0 | –36 | –4.0 | |
| 2 | 17 | 2.0 | 24 | 3.0 | |
| 3 | 20 | 3.0 | 17 | 3.0 | |
| Lung cancer | Overall | 176 | 2.0 | 108 | 2.0 |
| 1 | 33 | 1.0 | 31 | 1.0 | |
| 2 | 60 | 2.0 | 27 | 1.0 | |
| 3 | 84 | 5.0 | 49 | 3.0 | |
| Breast cancer | Overall | –19 | –1.0 | –131 | –5.0 |
| 1 | –54 | –4.0 | –54 | –6.0 | |
| 2 | 29 | 3.0 | –25 | –3.0 | |
| 3 | 6 | 1.0 | –51 | –8.0 | |
| Colorectal cancer | Overall | –12 | –0.0 | –92 | –3.0 |
| 1 | –33 | –2.0 | –49 | –4.0 | |
| 2 | 4 | 0.0 | –34 | –3.0 | |
| 3 | 17 | 2.0 | –10 | –1.0 | |
| Hematological cancers | Overall | 194 | 5.0 | –12 | –0.0 |
| 1 | 24 | 2.0 | 1 | 0.0 | |
| 2 | 136 | 11.0 | 21 | 2.0 | |
| 3 | 33 | 3.0 | –34 | –4.0 | |
| Diabetes | Overall | 8902* | 49.0 | 618 | 11.0 |
| 1 | 1411* | 19.0 | 61 | 3.0 | |
| 2 | 4612* | 77.0 | 420* | 23.0 | |
| 3 | 2879* | 62.0 | 138 | 9.0 | |
| Alzheimer’s | Overall | 2242* | 24.0 | 1184 | 15.0 |
| 1 | 309 | 8.0 | 197 | 6.0 | |
| 2 | 1398* | 45.0 | 805* | 31.0 | |
| 3 | 536* | 21.0 | 181 | 8.0 | |
| Ischemic heart disease | Overall | 6018* | 20.0 | 1700 | 9.0 |
| 1 | 736 | 6.0 | 99 | 1.0 | |
| 2 | 3376* | 34.0 | 1228* | 19.0 | |
| 3 | 1905* | 24.0 | 374 | 7.0 | |
| Kidney disease | Overall | 6724* | 47.0 | 579 | 19.0 |
| 1 | 886* | 15.0 | 115 | 9.0 | |
| 2 | 3535* | 76.0 | 285* | 28.0 | |
| 3 | 2303* | 66.0 | 179 | 23.0 | |
-
*
Confidence interval does not include zero.
Estimated Excess Deaths by Cause and Wave (California).
Estimated number of excess deaths and the percentage over baseline for each diagnosis group (California). Estimates are aggregated over all of 2020 and for each COVID-19 wave during 2020.
| Cause of death | Wave | Multiple cause | Underlying cause | ||
|---|---|---|---|---|---|
| Excess deaths | % Over baseline | Excess deaths | % Over baseline | ||
| Cancer | Overall | 991 | 2.0 | –29 | –0.0 |
| 1 | –102 | –1.0 | –236 | –1.0 | |
| 2 | 564 | 3.0 | 125 | 1.0 | |
| 3 | 529 | 4.0 | 82 | 1.0 | |
| Pancreatic cancer | Overall | –97 | –3.0 | –126 | –4.0 |
| 1 | –28 | –2.0 | –39 | –3.0 | |
| 2 | –69 | –5.0 | –70 | –6.0 | |
| 3 | 0 | 0.0 | –18 | –2.0 | |
| Lung cancer | Overall | –10 | –0.0 | –132 | –2.0 |
| 1 | –82 | –3.0 | –96 | –3.0 | |
| 2 | 18 | 1.0 | –48 | –2.0 | |
| 3 | 54 | 3.0 | 13 | 1.0 | |
| Breast cancer | Overall | 67 | 2.0 | –22 | –1.0 |
| 1 | –44 | –3.0 | –34 | –3.0 | |
| 2 | 92 | 6.0 | 44 | 4.0 | |
| 3 | 20 | 2.0 | –33 | –4.0 | |
| Colorectal cancer | Overall | 100 | 2.0 | 20 | 1.0 |
| 1 | 7 | 0.0 | –4 | –0.0 | |
| 2 | 66 | 4.0 | 25 | 2.0 | |
| 3 | 27 | 2.0 | –1 | –0.0 | |
| Hematological cancers | Overall | 279 | 5.0 | 52 | 1.0 |
| 1 | 0 | 0.0 | –33 | –2.0 | |
| 2 | 164 | 9.0 | 64 | 4.0 | |
| 3 | 114 | 8.0 | 20 | 2.0 | |
| Diabetes | Overall | 9163* | 39.0 | 1408* | 20.0 |
| 1 | 1843* | 18.0 | 213 | 7.0 | |
| 2 | 3846* | 49.0 | 620* | 27.0 | |
| 3 | 3474* | 59.0 | 575* | 33.0 | |
| Alzheimer’s | Overall | 2143* | 14.0 | 594 | 5.0 |
| 1 | 375 | 6.0 | –76 | –1.0 | |
| 2 | 1041* | 20.0 | 410 | 9.0 | |
| 3 | 726* | 18.0 | 259 | 8.0 | |
| Ischemic heart disease | Overall | 5905* | 16.0 | 2888* | 11.0 |
| 1 | 650 | 4.0 | 104 | 1.0 | |
| 2 | 2966* | 24.0 | 1581* | 19.0 | |
| 3 | 2289* | 25.0 | 1204* | 19.0 | |
| Kidney disease | Overall | 3858* | 21.0 | 8 | 0.0 |
| 1 | 301 | 4.0 | –114 | –8.0 | |
| 2 | 1967* | 33.0 | 63 | 6.0 | |
| 3 | 1590* | 36.0 | 59 | 7.0 | |
-
*
Confidence interval does not include zero.





