COVID-19: Avoiding culture shock with the SARS-CoV-2 spike protein
Researchers across the globe are frantically trying to understand the biology of different SARS-CoV-2 variants to develop new therapeutics and bring the COVID-19 pandemic to an end. The process begins in the laboratory, with painstaking experiments to judge whether a drug can stop SARS-CoV-2 from replicating in cells in a dish, or whether a vaccine can stop an animal from getting sick. But such experiments require copious amounts of SARS-CoV-2, and the authenticity of that virus stock (which is usually cultured in animal cell lines) is paramount to ensure the validity of test results.
The standard 'go-to' cells for producing stocks of SARS-CoV-2 are derived from the Vero lineage (which are kidney cells isolated from an African green monkey almost 60 years ago). These cells are highly susceptible to viruses due to the absence of type I interferon cytokines, an important group of signaling proteins released by cells in the presence of viruses. Vero cells are a popular choice for isolating and propagating many viruses because they are well characterized and easy to maintain, they adhere to laboratory dishes, and they show visible structural changes when infected. However, like viruses circulating naturally in human populations, viruses grown in the laboratory also have a tendency to change and adapt to the environment that they are in.
An early study, since replicated by others, found that SARS-CoV-2 stocks cultured in Vero-derived cells often harbor mutations or deletions in the spike gene (Lau et al., 2020). The deletions remove an important region on the spike protein, called the multibasic cleavage site, which affects the ability of the virus to infect human airway cells (Hoffmann et al., 2020; Mykytyn et al., 2021; Pohl et al., 2021). Such viruses therefore do not behave like authentic SARS-CoV-2 in several aspects: they are less pathogenic (Johnson et al., 2021; Lau et al., 2020); they do not transmit (Peacock et al., 2021); and they exhibit altered sensitivities to inhibition by antiviral interferon-stimulated genes and patient antibodies (Johnson et al., 2021; Winstone et al., 2021).
These characteristics can make it difficult to interpret laboratory experiments that use Vero-produced viruses to assess the effectiveness of experimental drugs or vaccines. The ability of inactivated SARS-CoV-2 vaccines made in Vero cells to stimulate correct antibody responses might also be partially compromised, although this has not been formally assessed (Gao et al., 2020; Wang et al., 2020). Now, in eLife, Bart Haagmans and colleagues of the Erasmus Medical Center in Rotterdam and the University of Illinois at Urbana-Champaign – including Mart Lamers as first author – report simple methods for producing SARS-CoV-2 stocks in human cells that prevent such mutations and deletions in the gene for the spike protein (Figure 1; Lamers et al., 2021).
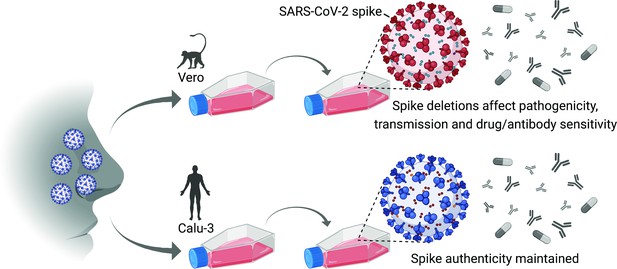
Culturing SARS-CoV-2 in Vero cells and human cells.
Schematic representation of a human SARS-CoV-2 patient sample passaged using the Vero cell line (which was isolated from an African green monkey almost 60 years ago; top), or the Calu-3 cell line (which is a human cell line; bottom). Vero cells are deficient in a serine protease called TMPRSS2 that is needed for the virus to enter cells at the plasma membrane; however, certain SARS-CoV-2 variants with spike deletions (shown in red) can enter Vero cells via a different pathway, so these variants are artificially selected for and come to dominate the virus population. The pathogenicity, transmission properties, and sensitivity to antiviral drugs and antibodies of the variants are different to those of the wild-type virus. Calu-3 cells are not deficient in TMPRSS2, so the authenticity of the spike gene is maintained, and studies with such virus stocks more faithfully recapitulate human virus biology.
Figure created with BioRender.com.
First, Lamers et al. used a method called deep sequencing to confirm that repeated culture of SARS-CoV-2 in Vero cells leads to an increase in viral genomes with mutations or deletions in the important region of the spike gene. Less sensitive sequencing methods, or a reliance on 'consensus sequences', can leave researchers with the false impression that such deletions are absent.
Lamers et al. then pinpointed how these spike deletions give certain SARS-CoV-2 variants a replicative advantage in Vero cells, which enables them to dominate the virus population. Vero cells are deficient in a serine protease that is needed for SARS-CoV-2 to enter human airway cells at the plasma membrane: however, SARS-CoV-2 variants with the spike gene deletions exploit a different pathway (called endocytosis) to enter Vero cells. It seems the ability of the variants to take advantage of this second entry route allows them to dominate when Vero cells are used.
Lamers et al. next asked whether a human-airway cell line, Calu-3, might be a better alternative to culture SARS-CoV-2, given that this cell line possesses the necessary protease (Mykytyn et al., 2021). Indeed, they found that repeated culture of SARS-CoV-2 in Calu-3 cells (or Vero cells engineered to express the serine protease) prevented the accumulation of mutations and deletions in the SARS-CoV-2 spike. Moreover, Calu-3 cells were as good as Vero cells at producing the large amounts of virus necessary for further experiments. Thus, the authentic nature of SARS-CoV-2 stocks made in this way, as assessed by deep sequencing, will give confidence to the interpretation of subsequent experiments.
The results from this study make a compelling case for SARS-CoV-2 researchers to thoroughly characterize the genomic sequences of the virus stocks they produce (and to avoid consensus sequencing). Furthermore, researchers should consider the cells, the growth media and the additives used for virus production to prevent artefactual SARS-CoV-2 culture adaptations that might impact the evaluation of drug or vaccine effectiveness.
Cell culture systems to propagate viruses are the linchpin of virology, yet they have not really changed since the beginnings of the field. The application of modern technological advances, such as rational gene editing of cells or the use of in vivo-like organoid tissue models, promises to transform this critical aspect of virology and should allow researchers to update their methods to maintain experimental authenticity.
References
-
Attenuated SARS-CoV-2 variants with deletions at the S1/S2 junctionEmerging Microbes & Infections 9:837–842.https://doi.org/10.1080/22221751.2020.1756700
Article and author information
Author details
Publication history
Copyright
© 2021, Hale
This article is distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use and redistribution provided that the original author and source are credited.
Metrics
-
- 2,280
- views
-
- 161
- downloads
-
- 8
- citations
Views, downloads and citations are aggregated across all versions of this paper published by eLife.
Download links
Downloads (link to download the article as PDF)
Open citations (links to open the citations from this article in various online reference manager services)
Cite this article (links to download the citations from this article in formats compatible with various reference manager tools)
Further reading
-
- Epidemiology and Global Health
- Microbiology and Infectious Disease
Influenza viruses continually evolve new antigenic variants, through mutations in epitopes of their major surface proteins, hemagglutinin (HA) and neuraminidase (NA). Antigenic drift potentiates the reinfection of previously infected individuals, but the contribution of this process to variability in annual epidemics is not well understood. Here, we link influenza A(H3N2) virus evolution to regional epidemic dynamics in the United States during 1997—2019. We integrate phenotypic measures of HA antigenic drift and sequence-based measures of HA and NA fitness to infer antigenic and genetic distances between viruses circulating in successive seasons. We estimate the magnitude, severity, timing, transmission rate, age-specific patterns, and subtype dominance of each regional outbreak and find that genetic distance based on broad sets of epitope sites is the strongest evolutionary predictor of A(H3N2) virus epidemiology. Increased HA and NA epitope distance between seasons correlates with larger, more intense epidemics, higher transmission, greater A(H3N2) subtype dominance, and a greater proportion of cases in adults relative to children, consistent with increased population susceptibility. Based on random forest models, A(H1N1) incidence impacts A(H3N2) epidemics to a greater extent than viral evolution, suggesting that subtype interference is a major driver of influenza A virus infection ynamics, presumably via heterosubtypic cross-immunity.
-
- Microbiology and Infectious Disease
Understanding the interplay between the HIV reservoir and the host immune system may yield insights into HIV persistence during antiretroviral therapy (ART) and inform strategies for a cure. Here, we applied machine learning (ML) approaches to cross-sectional high-parameter HIV reservoir and immunology data in order to characterize host–reservoir associations and generate new hypotheses about HIV reservoir biology. High-dimensional immunophenotyping, quantification of HIV-specific T cell responses, and measurement of genetically intact and total HIV proviral DNA frequencies were performed on peripheral blood samples from 115 people with HIV (PWH) on long-term ART. Analysis demonstrated that both intact and total proviral DNA frequencies were positively correlated with T cell activation and exhaustion. Years of ART and select bifunctional HIV-specific CD4 T cell responses were negatively correlated with the percentage of intact proviruses. A leave-one-covariate-out inference approach identified specific HIV reservoir and clinical–demographic parameters, such as age and biological sex, that were particularly important in predicting immunophenotypes. Overall, immune parameters were more strongly associated with total HIV proviral frequencies than intact proviral frequencies. Uniquely, however, expression of the IL-7 receptor alpha chain (CD127) on CD4 T cells was more strongly correlated with the intact reservoir. Unsupervised dimension reduction analysis identified two main clusters of PWH with distinct immune and reservoir characteristics. Using reservoir correlates identified in these initial analyses, decision tree methods were employed to visualize relationships among multiple immune and clinical–demographic parameters and the HIV reservoir. Finally, using random splits of our data as training-test sets, ML algorithms predicted with approximately 70% accuracy whether a given participant had qualitatively high or low levels of total or intact HIV DNA . The techniques described here may be useful for assessing global patterns within the increasingly high-dimensional data used in HIV reservoir and other studies of complex biology.






