Science Forum: Adding a One Health approach to a research framework for minority health and health disparities
Abstract
The National Institute on Minority Health and Health Disparities (NIMHD) has developed a framework to guide and orient research into health disparities and minority health. The framework depicts different domains of influence (such as biological and behavioral) and different levels of influence (such as individual and interpersonal). Here, influenced by the “One Health” approach, we propose adding two new levels of influence – interspecies and planetary – to this framework to reflect the interconnected nature of human, animal, and environmental health. Extending the framework in this way will help researchers to create new avenues of inquiry and encourage multidisciplinary collaborations. We then use the One Health approach to discuss how the COVID-19 pandemic has exacerbated health disparities, and show how the expanded framework can be applied to research into health disparities related to antimicrobial resistance and obesity.
Introduction
Research frameworks are useful because they allow important problems to be tackled from many different directions and perspectives (Mills et al., 2010) For the individual researcher, a framework can help with the formulation of research questions and situate their research in a broader context. Research frameworks are also useful to funding agencies: for example, the National Institute on Minority Health and Health Disparities (NIMHD) in the United States employs a research framework to assess the state of current research and to identify gaps and opportunities for funding (Alvidrez et al., 2019).
The NIMHD framework has two axes: the vertical axis lists five “domains” that influence minority health and health disparities (biological, behavioral, physical/built environment, sociocultural environment, and healthcare system), while the horizontal axis lists four “levels of influence” (individual, interpersonal, community, and societal). The model builds on a framework for research into health disparities that was developed by the National Institute on Aging, (Hill et al., 2015) and also on the socioecological model (Bronfenbrenner, 1977; Kilanowski, 2017).
The NIMHD encourages using the research framework to examine the interaction of factors from different domains and levels to understand health disparities. Investigators can use the framework while conducting their literature review to map and organize study findings and identify gaps in knowledge. Then, they can formulate research questions and define theories and models evaluating the influence of factors from several levels and domains. For example, the NIMHD has used the framework to evaluate disparities by racial/ethnic category in lung cancer mortality by identifying factors from three domains and levels of influence. Specifically, genetic risk is highlighted as a determinant in the biological domain and at the individual level, while access to quality treatment is an influence in the healthcare system domain and at the community level. Moreover, the framework facilitates considerations of the influence of structural racism on health disparities: differences in state laws, cigarette taxes, social norms, and smoking bans affect racial and ethnic category disparities through the behavioral domain and the societal level (Alvidrez et al., 2019). The framework highlights the complex nature of minority health and health disparities, and the need to consider multiple domains and levels of influence when trying to understand these areas and change them for the better (see Box 1 for definitions of minority health and other terms used in this article).
Definitions.
Minority health: Aspects of health and disease among racial and ethnic category minority populations as defined by the US Census.
Health disparity: A preventable difference in health outcomes that adversely affects socially and/or economically disadvantaged populations. These populations include racial and ethnic category minority groups, persons of less privileged socioeconomic status, underserved rural residents, and sexual and gender minorities; all share a social disadvantage in part due to having been subject to discrimination or racism.
One Health: An approach recognizing the health of people is closely connected to the health of animals and our shared environment; the health of one affects the health of all. One Health is a collaborative and multidisciplinary approach to understanding and managing health in a wholistic way that prioritizes ecosystem balance.
Human ecosystem: Combines components of the ecosystem traditionally recognized by ecologists (plants, animals, microbes, physical environmental complex) with the built environment and social characteristics, structures, and interactions of interest.
Research framework: A structure supporting collective scientific endeavours by guiding the development and investigation of a research question and conceptualizing the relationship between relevant factors.
The importance of merging aspects of environmental health with health equity has long been highlighted by the World Health Organization. In 2008, for example, the Commission on Social Determinants of Health stressed the impact of climate change on the health of individuals and the planet (Gama and Colombo, 2010). Increasingly, studies show that biological, cultural and environmental factors – and interactions between these factors – are all relevant to research into health disparities, (van Daalen et al., 2020; Garnier et al., 2020; Mueller et al., 2018) and the COVID-19 pandemic has increased focus on the human-animal-environment interface (de Garine-Wichatitsky et al., 2020). However, it is challenging to include the impact of environmental factors and human-animal linkages on health disparities in the NIMHD framework, so we are proposing to expand the framework by adding two new levels of influence – interspecies and planetary – and making use of the “One Health” approach to thinking about the emergence and prevention of disease. (CDC, 2020a) This expansion allows researchers to build on the biological and social determinants of health, and their root causes such as structural racism, already explored in the NIMHD framework. The two new levels of influence explicitly frame questions that link interspecies factors (i.e., the interactions between the human host and their microbiome or animal and human shared infections) and planetary factors (i.e., rising temperatures or global food production practices) with those stemming from biological, social, cultural, and structural and explore their combined impact on health and disease.
Health disparities and One Health
The One Health approach involves multiple health science professions collaborating to attain optimal health for people, other animals, and the environment (Schneider et al., 2019). The One Health approach has primarily been adopted to investigate and prevent the spread of infectious and zoonotic diseases.(Kelly et al., 2020; Schmiege et al., 2020). For several endemic, zoonotic diseases, One Health approaches targeting animal or environmental reservoirs of infection have proven more equitable than interventions focusing on clinical management of disease, which can be inaccessible for disadvantaged and poor communities. In Latin America, for example, modest investments in mass dog vaccinations have effectively prevented rabies-related death in humans and resulted in near elimination of the virus from the community (Vigilato et al., 2013). This approach has been more effective, and equitable, than increased expenditures in the administration of post-exposure prophylaxis, which has been emphasized in many Asian countries where there is still high incidence of human rabies cases (Cleaveland et al., 2017).
Human health is linked to non-human animal health in many ways: some of these links are direct (e.g., food consumption) and some are indirect (e.g., via the environment), and many of these links are not fully understood (Davis and Sharp, 2020; Wolf, 2015). Differences in the frequency of human-animal interactions among population groups, (Rabinowitz and Conti, 2013) individual and cultural food practices, (Wolfe et al., 2005; Kamau et al., 2021) livelihood systems, (Woldehanna and Zimicki, 2015) and livestock production practices (Edwards-Callaway, 2018; Ducrot et al., 2008) could lead to health disparities. These relationships are particularly relevant for populations such as farmworkers, (Pol et al., 2021) people experiencing homelessness, (Hanrahan, 2019) individuals living in agricultural communities, (Wing and Wolf, 2000) and certain racial and ethnic category minorities. For example, individuals with high fish diets have the potential for increased exposure to harmful contaminants influenced by waterway pollutants, marine food webs, and climate change (Gribble et al., 2016). The unequal distribution of pollutants is a matter of environmental racism, and this interacts with other social and structural factors disproportionately impacting impoverished communities and communities of color. This may be particularly relevant among Native American and Pacific Islander communities who consume fish at higher rates than other subpopulations (Washington State Department of Ecology, 2013). There is limited research in the area, but evidence of elevated blood mercury among these groups (Hightower et al., 2006) could lead to health disparities stemming from a complex association between environmental justice, climate change, systemic racism, and this interspecies relationship (CDC, 2021b). The NIMHD framework does not easily facilitate consideration of these determinants.
There is a bidirectional relationship between human and environmental health, and the NIMHD framework includes the physical/built environment as a domain of influence. However, the natural environment and climate change can also influence health disparities. For example, extreme weather events or changes to the natural environment can disproportionately impact segments of the population based on geography and access to resources. In the Western part of the United States, the increasing number, size, and intensity of wildfire events occurring due to extreme heat and drought may disproportionately impact nearby populations through displacement or prolonged exposure to smoke, worsening or creating new populations with health disparities (US EPA, 2017a). Further, climate change impacts on health, environmental pollutants, habitat loss, biological diversity, and the distribution of resources, disproportionately impact poor people and populations of color, and can drive or exacerbate health disparities (van Daalen et al., 2020; Huong et al., 2020; Hinchliffe et al., 2021).
As an example of the interconnectedness of plant and human health, consider a mycotoxin called aflatoxin that is produced by common fungi and may play a causative role in hepatocellular carcinoma (Ramirez et al., 2017). Hepatocellular carcinoma disproportionately affects Latinos, and aflatoxin commonly affects corn and maize crops, considered a Latin American dietary staple (Overcash and Reicks, 2021). Climate change impacts on temperature and drought increase aflatoxin levels in crops and could exacerbate hepatocellular carcinoma disparities among populations relying on the health and safety of those crops (Kebede et al., 2012).
The complexity of the linkages humans have with each other, with non-human species, and with the environment should be incorporated with the exploration of social systems and structural racism to understand or model health outcomes and subsequent health disparities (Craddock and Hinchliffe, 2015). We believe adding elements of the One Health approach to the NIMHD framework will help expand health disparities research, open new avenues of inquiry for both One Health and health disparities researchers, and promote multidisciplinary collaborations, all of which should lead to broader and more sustainable solutions to health disparities. Using the COVID-19 pandemic as a motivating example, we will use the One Health approach to identify new determinants of health disparities not easily incorporated in the original NIMHD framework. We will then present an expanded research framework and show how this new framework can be used to think about health disparities in the fields of infectious diseases (using antimicrobial resistance as an example) and non-communicable diseases (using obesity as an example).
While the One Health approach and the NIMHD framework are already being used by researchers, the work is conducted in disciplinary silos. One Health researchers may not see how they can help inform and address health disparities or how they can begin incorporating social and structural systems in their work (Craddock and Hinchliffe, 2015; Solis and Nunn, 2021). Health disparities researchers may not consider the influence of the broader human ecosystem and its interactions with social, cultural, and structural systems. We hope that the expanded research framework will highlight the overlap in their work and stimulate new areas of research and thinking. It is important to note the relationships presented throughout are theoretical and meant to be illustrative of the hypothesis generating potential of the expanded framework, not an assumption of causal relationships or a replacement for exploring the complex social and structural systems creating health disparities. Further, although the NIMHD research framework focuses on minority health and health disparities in the United States, we will discuss how it might also apply to other countries.
Health disparities and COVID-19
The disproportionate impact COVID-19 has had on some racial and ethnic category minority populations, and on people with low economic resources, has re-centered conversations concerning health disparities. Those with underlying medical conditions (such as diabetes, heart disease, and chronic lung disease) have also been strongly overrepresented in case severity and fatalities (Burch and Searcey, 2020; Kim et al., 2020). Marginalized communities already impacted by health disparities are also disproportionately affected by these conditions, increasing the harm caused by COVID-19 (Kim et al., 2020; Lopez et al., 2021). Several of the factors that contribute to COVID-19 health disparities are accounted for in the NIMHD framework (such as structural racism and its impact on neighborhood and built environment characteristics, healthcare access, occupation and workplace conditions, income, and education CDC, 2020b). The One Health approach allows factors not easily accounted for in the NIMHD framework (such as disproportionate access to natural resources like clean air, drinking water, potable water for sanitation and hygiene, and nutritious foods) to be considered (Garnier et al., 2020).
The WHO has classified COVID-19 as a zoonotic disease (WHO, 2020). While an animal reservoir has not yet been identified, (Haider et al., 2020) most zoonotic diseases are thought to enter human populations through a spill-over event originating from human-animal exposure. Unlike some zoonotic diseases, COVID-19 does not require a non-human animal host for pathogen persistence. The disease may have originated in animals and then independently persisted in human populations through respiratory transmission (Singla et al., 2020; Jayaweera et al., 2020; Meyerowitz et al., 2021).
Epidemics of zoonotic origin can be triggered by changes in human and non-human animal reservoirs’ interaction dynamics. Environmental, climatic, socio-economic, and habitat or animal abundance changes can modify the probability of human and non-human animal interactions. And as the rate of such interactions increases, so does the rate at which respiratory viruses and other infectious agents evolve and adapt to their new hosts (Duffy, 2018). Understanding the drivers of non-human animal and environmental exposures can build on social and systemic factors by incorporating human-animal linkages and planetary health to deepen our understanding of the COVID-19 pandemic and related health inequities. This improved understanding may strengthen our capacity to prevent and better predict the course of future pandemic threats.
Disease transmission between humans and non-human animals is a primary focus of the One Health approach. Previous coronavirus outbreaks exemplify the ways human interactions with non-human animals can increase viral exposure. Human invasion of the natural environment, contact with livestock, rodents, shrews, or bats, as well as the consumption of rare and wild non-human animals, contributes to infection with viruses we normally would not encounter (Li et al., 2019). For COVID-19, exposure to bridge hosts (the species that transmit viruses to humans from their natural reservoirs) may be a predictor of viral exposure early in the outbreak (Solis and Nunn, 2021). Hypothesized COVID-19 bridge hosts include animals in animal markets or domesticated animals and livestock (El Zowalaty and Järhult, 2020). High rates of exposure to wildlife and livestock is an identified predictor of COVID-19 exposure in China, mainly between poultry and rodents/shrews in living dwellings (Li et al., 2019). Viral reservoirs and bridge hosts exposures are associated with less economic resources, inadequate housing and impoverished neighborhoods (i.e., stagnant water, animals residing in dwellings, uncollected trash, and overgrown lots), adding potential mediating factors to determinants of health identified in the NIMHD framework (Solis and Nunn, 2021). There are also many aspects of COVID-19 related to minority health and health disparity that we are unable to discuss in detail for reasons of space: these include the impact of the human-animal bond on COVID-19 mental health outcomes, (Shim, 2020; Saltzman et al., 2021; Brooks et al., 2018; Ratschen et al., 2020) the influence of environmental factors (notably temperature, humidity, and atmospheric pollution) on morbidity, (Ratschen et al., 2020; Chin et al., 2020; Ma et al., 2020; Conticini et al., 2020) and questions related to vaccine equity (Katz et al., 2021).
Experts agree that COVID-19 will not be the last pandemic (Gill, 2020). Learning from our successes and mistakes during this pandemic will be crucial to prepare appropriately. COVID-19 highlights the importance of considering how the relationships between humans, non-human animals, and the environment affect minority health and contribute to health disparities. Expanding the NIMHD framework to explicitly include determinants from these domains can help us foresee and better respond to future, global threats by expanding our view of health determinants and drivers of disparities. We believe this is best achieved by incorporating a One Health approach in the NIMHD framework. Recently, a One Health Disparities framework was introduced for zoonotic disease researchers to incorporate the ways the social environment relates to disparities in disease exposure, susceptibility, and expression (Solis and Nunn, 2021). Alternatively, we are proposing an expanded NIMHD framework as a way for health disparities researchers to explicitly include determinants stemming from human-animal and human-environmental linkages in their work. The relevance of this expansion will become even more clear heading into the future. As globalization increases, climate change progresses, and population growth continues to strain the relationship between humans, non-human animals, and the environment, thinking about health and health disparities in this holistic way will be essential.
The expanded framework
Our proposed expansion involves adding two new levels of influence from the One Health approach – the interspecies and planetary levels – to the NIMHD framework (Figure 1). The interspecies level covers the interplay, interconnectedness, and interdependencies of humans and non-human species (Davis and Sharp, 2020). The definition of interspecies is kept as broad as possible to allow room for new areas of inquiry and flexibility in adapting the framework. The planetary level includes the Earth’s natural systems, resources, and biodiversity (Lerner and Berg, 2017). Adding these two new levels promotes the evaluation of health disparities mechanisms across disciplines by introducing aspects of the human ecosystem previously missing from the NIMHD framework.
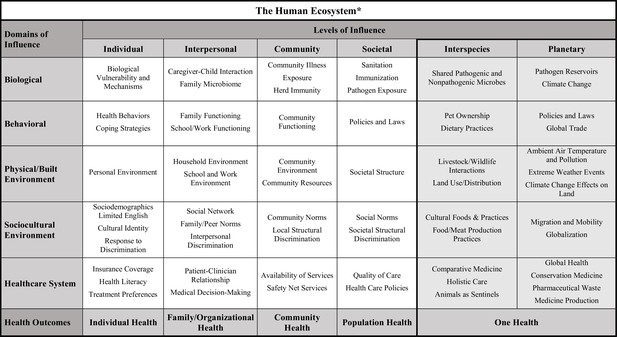
Proposed expansion of the National Institute on Minority Health and Health Disparities (NIMHD) research framework.
The NIMHD research framework includes five domains (rows) and four levels (columns) that influence minority health and health disparities. The proposed expansion of the framework introduces two new levels of influence – the interspecies level and the planetary level (both shaded in grey). The new framework reflects how human health is a product of the human ecosystem, which combines traditionally recognized ecosystem components (plants, animals, microbes, physical environmental complex) with the built environment and social characteristics, structures, and interactions between all these elements. The figure shows examples of some of the factors that are relevant at the intersection between each domain and each level. The origins of the two new levels lie in the “One Health” approach, which recognizes that the health of people is closely connected to the health of animals and our shared environment. The bottom row of the framework demonstrates that health outcomes can also span multiple levels – individual, family and organizational, community, population, and, in the expanded framework, One Health.
Just as the interpersonal level in the present framework explores human-human interactions, the new interspecies level explores relationships between humans and non-human species across all five domains of influence. Examples of such relationships include microbes shared between humans and non-human animals (i.e., the biological domain), (Trinh et al., 2018) pet ownership (behavioral), (Mueller et al., 2018) livestock and wildlife interactions (physical/built environment), (Hemsworth, 2003) food production practices (sociocultural environment), (Edwards-Callaway, 2018; Ducrot et al., 2008) and comparative medicine, a discipline that synergizes health research in human and non-human animal medicine (healthcare system) (Center for Veterinary Medicine, 2021).
In the present framework, the societal level of influence includes the presence and actions of governmental and civil society organizations at different levels (such as state, country, or region), (Alvidrez et al., 2019) and the new planetary level of influence adds considerations of globalization and impacts of the natural environment. Examples include the effects on minority health and health disparities of climate change (i.e., the biological domain), (US EPA, 2017b) global trade (behavioral), (Friel et al., 2015) ambient air temperature and pollution (physical/built environment), (Son et al., 2019; Yi et al., 2010; Schifano et al., 2013) migration and mobility (sociocultural environment), (Castañeda et al., 2015) global health programs, and the global system for producing medicines and medical devices (healthcare system) (Newman and Cragg, 2020). More examples are given in Figure 1 (but please note that these examples are not meant to be comprehensive or to imply causal inference).
Example: Antimicrobial resistance
We will now show how the expanded framework can be applied to research into health disparities in two areas: antimicrobial resistance (AMR) (Figure 2) and obesity. The problem of AMR is primarily driven by antibiotic overuse and misuse in humans, non-human animals, and the environment. Moreover, the interconnected nature of AMR means that it has already been studied by One Health researchers, (McEwen and Collignon, 2018; Robinson et al., 2016) which makes it a promising candidate for the expanded NIMHD framework. There are documented disparities by racial and ethnic category in antibiotic use and AMR infections in the US (Olesen and Grad, 2018; Hota et al., 2007; Iwamoto et al., 2013). There are also known occupational disparities in AMR pathogen exposure, with those in the agricultural and medical fields being at increased risk (Fynbo and Jensen, 2018; Voss et al., 2005). Racial/ethnic category minority individuals, such as African American/Black and Hispanic/Latino, are more likely to work in these industries due to a combination of government policies and laws, and the unequal distribution of income and resources (Division of Labor Force Statistics, 2020).
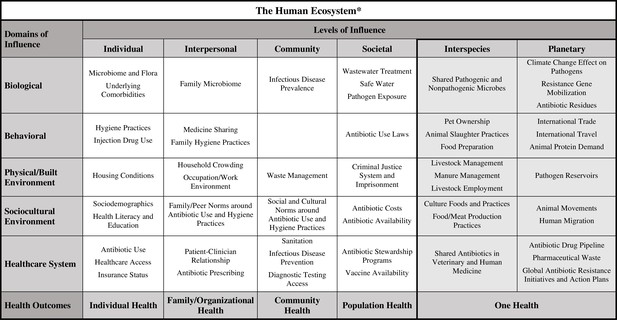
Expanded framework applied to health disparities research in antimicrobial resistance (AMR).
An example of how the expanded framework can be utilized by investigators as they develop their research questions and study designs for research into disparities related to AMR and AMR-related infections. The factors listed under the interspecies and planetary levels of influence are included in a more straightforward and systematic way than they would be in the original NIMHD framework.
Under the NIMHD framework, the domain/level of influence combinations relevant to AMR disparities could include housing conditions (individual/physical plus built environment), antibiotic sharing among family and peers and access to medications without prescriptions (interpersonal/behavioral), and antibiotic prescribing practices (interpersonal/healthcare system). However, there are other potential sources of health disparities related to AMR that are not accommodated by the NIMHD framework. By encouraging the consideration of interactions between humans and other species through the inclusion of an interspecies level, the expanded framework will enable the identification of some of these factors. One example might be antibiotic sharing between humans and non-human animals (i.e., the healthcare domain). Further, humans and non-human animals share and exchange pathogenic and non-pathogenic bacteria (i.e., the biological domain). A third example is that individuals living in rural and agricultural communities are disproportionately impacted by environmental exposures associated with nearby livestock and manure management practices (i.e., the physical/built environment domain). Additionally, while the evidence on whether livestock raised with antibiotics have higher levels of AMR than those raised without antibiotics is mixed, and we test animal products for antibiotic residues in the US, this is not necessarily true for the rest of the world (Vikram et al., 2018; Van Boeckel et al., 2019).
Since antibiotic-free meat is often cost-prohibitive for those with low socioeconomic status, consumption of livestock raised with antibiotics in countries with fewer regulations may be important to consider when exploring AMR disparities by income, geography, or race/ethnicity category. The interspecies level of influence explicitly frames human exposure to non-human species in the home, workplace, or environment as relevant determinants of health disparities related to AMR.
Globalization and climate change are also highly relevant when considering AMR, and the planetary level of influence in the expanded framework allows these factors to be considered straightforwardly and clearly. International trade and travel (i.e., the behavioral domain) transfer bacteria and viruses across borders through the import and export of organic materials and human movement. These could be significant determinants to consider as certain immigrant populations in the US frequently travel to their native countries, many of which have a high prevalence of AMR infections (Nadimpalli et al., 2021; Ruppé et al., 2018). The planetary level is also relevant to the challenge of dealing with pharmaceutical waste. How we manage such waste (i.e., the healthcare system domain), and how such waste is distributed, could be associated with socioeconomic status, putting those of lower status at increased risk for exposure to antibiotic residues (biological domain) and pathogen reservoirs (physical/built environment domain).
The risk factors for AMR are well documented, but our understanding of the combination of factors and interactions that contribute to disparities in AMR is limited (Holmes et al., 2016). Including the planetary level of influence in the expanded framework highlights the need for multidisciplinary research that considers the interplay between humans, biodiversity, and the environment (Venkatasubramanian et al., 2020). For example, environmental scientists could collaborate on studies evaluating geographic disparities in AMR that explore the possible impact of climate change on the abiotic environment in which people live (i.e., the planetary level/biological domain), and how the effect of this relationship disproportionately impacts segments of the population based on socioeconomic status. While there is no direct evidence of climate change impacts to the abiotic environment leading to disparities in AMR, the expanded framework allows such possibilities to be explored.
Example: Obesity
Obesity, defined by a body mass index above 30 kg/m2, is a major public health concern due to its contribution to several leading causes of disability and death, including diabetes, heart disease, stroke, osteoarthritis, and cancer (CDC, 2021a). Obesity affects people in every country worldwide and the prevalence is increasing, making it classifiable as a pandemic (Swinburn et al., 2019). This pandemic results from a number of factors, including urbanization, global trade, and easy access to inexpensive caloric-dense food, (Swinburn et al., 2019) and disparities in obesity are evident by geography, gender, age, and socioeconomic status, as well as race and ethnicity categories (Hill et al., 2014; Wang and Beydoun, 2007). Solutions to the growing obesity pandemic will, therefore, require a multifaceted understanding of all these factors and the interactions between them.
The NIMHD framework facilitated our thinking about long-standing structural racism and how racial residential segregation, inequitable access to healthy and affordable food, and reduced opportunities for a healthy lifestyle lead to obesity-related health disparities (Bleich and Ard, 2021). Behaviors contributing to these disparities may include physical activity and diet (i.e., the individual level/behavioral domain), cheap pricing of low nutritional value foods (the societal level/behavioral domain), targeted marketing or advertising (societal level/sociocultural environment domain) and the distribution of full-service grocery stores, convenience stores, and fast-food restaurants that results from societal level factors such as systemic racism affecting zoning laws and lending practices (community level/physical plus built environment domain) (Petersen et al., 2019). We believe the expanded framework (Figure 3) can build on these efforts, broaden the scope of health disparities research in obesity, and foster collaboration among researchers from different disciplines.
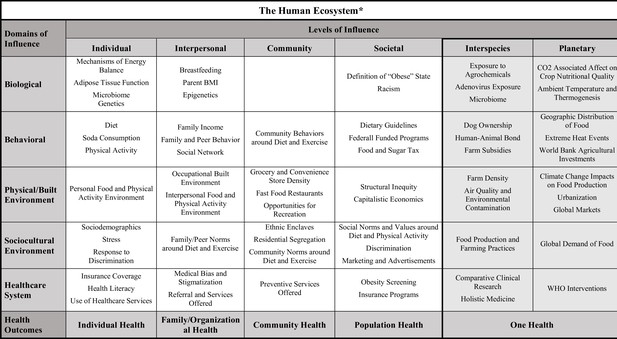
Expanded framework applied to health disparities research in obesity.
An example of how the expanded framework can be utilized by investigators as they develop their research questions and study designs for research into disparities related to obesity. The factors listed under the interspecies and planetary levels of influence are included in a more straightforward and systematic way than they would be in the original NIMHD framework.
For example, emerging data shows changes to our microbiome, a non-human species living within us, can affect our health, and obesity (Feng et al., 2020). Social, economic, and environmental factors are likely to modify the microbiome over time, resulting in poor health outcomes (Findley et al., 2016). Thus, changes to the microbiome may be an important mediator or modifier in studies evaluating the relationship between social factors and obesity among socially disadvantaged communities.
The expanded framework could also guide disparities research in new directions. For example, two zoonotic viruses – avian adenovirus (SMAM-1) and adenovirus 36 (Adv36) – are associated with obesity in both humans and non-human animals (Ponterio and Gnessi, 2015). There is some evidence for racial/ethnic category and geographic differences in Adv36 seropositivity, but research in this area (at the intersection between the interspecies level and the biological domain) is limited (Tosh et al., 2020; LaVoy et al., 2021). Finally, the expanded framework can also facilitate multidisciplinary collaboration. For example, there is a correlation between obesity in dogs and obesity in their owners: (Bjørnvad et al., 2019) this suggests that public health professionals could work with veterinarians to disseminate health and educational information regarding pets and owners. This type of approach has the bonus of potentially reaching marginalized populations who may mistrust the medical system, lack health insurance, or participate in alternative medicine practices (and are therefore missed by the traditional routes for disseminating health information). Previous studies have successfully improved access to vital services among some of the highest-risk populations, such as those experiencing homelessness, by leveraging the human-animal bond and providing healthcare services through a One Health model (Panning et al., 2016).
The Lancet Commission on Obesity deems climate change effects on health a pandemic, and emphasizes how interconnected it is with the obesity pandemic. Efforts to address disparities in obesity could be strengthened by considering the links between the two pandemics and exploring the influence of planetary factors on disparities. Questions for researchers to address would include: how do increases in atmospheric carbon dioxide affect crop nutritional quality, and how do rising temperatures disproportionately impact the geographic distribution of food crops, thermogenesis, and food insecurity? And what are the impacts of anthropogenic changes to the environment (such as urbanization or increased air pollution) and the increasing global demand for food? With regard to disparities, it will be important to explore how climate change disproportionately impacts individuals of low socioeconomic status through food insecurity, reduced opportunities for physical activity or metabolic processes. For example, rising atmosphere air temperature is associated with less adaptive thermogenesis, the complex metabolic process by which humans burn energy to generate heat. This association is likely to disproportionately harm disadvantaged populations who are more likely to work outdoors and live in hotter urban areas than their more privileged counterparts (Koch et al., 2021).
Conclusions
The NIMHD has developed a flexible and adaptable framework to inform research into minority health and health disparities in the United States. In this article, influenced by the One Health approach, we added two new levels of influence – interspecies and planetary – to the NIHMD framework and demonstrated how the expanded framework could open new avenues of inquiry and encourage multidisciplinary collaborations. We then applied the framework to two examples: AMR and obesity.
While our proposal aims to stimulate novel thinking, we acknowledge the need for more evidence to show that adding a One Health approach can be beneficial to research addressing health disparities. Further, we do not expect the expanded framework to be relevant and applicable for all fields and topics. Moreover, we accept that many other factors – related to putting collaborations together, obtaining funding for projects, and collecting and analyzing data – must be addressed.
Human health is complex and is influenced by many different factors. By ensuring that our expanded framework includes factors related to interactions between humans and other species, and factors related to globalization and climate change, we believe that it will help ensure that no stone remains unturned in efforts to improve health for all and reduce health disparities.
Data availability
There is no accompanying data for the paper.
References
-
The National Institute on Minority Health and Health Disparities Research FrameworkAmerican Journal of Public Health 109:S16–S20.https://doi.org/10.2105/AJPH.2018.304883
-
Toward an experimental ecology of human developmentAmerican Psychologist 32:513–531.https://doi.org/10.1037/0003-066X.32.7.513
-
Immigration as a social determinant of healthAnnual Review of Public Health 36:375–392.https://doi.org/10.1146/annurev-publhealth-032013-182419
-
One Health contributions towards more effective and equitable approaches to health in low- and middle-income countriesPhilosophical Transactions of the Royal Society. Series B, Biological Sciences 372:1725.https://doi.org/10.1098/rstb.2016.0168
-
Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern ItalyEnvironmental Pollution (Barking, Essex: 1987) 261:114465.https://doi.org/10.1016/j.envpol.2020.114465
-
One world, one health? Social science engagements with the One Health agendaSocial Science & Medicine 129:1–4.https://doi.org/10.1016/j.socscimed.2014.11.016
-
Rethinking One Health: Emergent human, animal and environmental assemblagesSocial Science & Medicine 258:113093.https://doi.org/10.1016/j.socscimed.2020.113093
-
Will the COVID-19 crisis trigger a One Health coming-of-age?The Lancet. Planetary Health 4:e377–e378.https://doi.org/10.1016/S2542-5196(20)30179-0
-
WebsiteEmployed Persons by Detailed Industry, Sex, Race, and Hispanic or Latino EthnicityAccessed June 28, 2022.
-
Review on the epidemiology and dynamics of BSE epidemicsVeterinary Research 39:15.https://doi.org/10.1051/vetres:2007053
-
Why are RNA virus mutation rates so damn high?PLOS Biology 16:e3000003.https://doi.org/10.1371/journal.pbio.3000003
-
Human–animal interactions: Effects, challenges, and progressAdvances in Cattle Welfare 2018:71–92.https://doi.org/10.1016/B978-0-08-100938-3.00004-8
-
Impact of air pollution on intestinal redox lipidome and microbiomeFree Radical Biology & Medicine 151:99–110.https://doi.org/10.1016/j.freeradbiomed.2019.12.044
-
Health Disparities and the MicrobiomeTrends in Microbiology 24:847–850.https://doi.org/10.1016/j.tim.2016.08.001
-
Trade policy and public healthAnnual Review of Public Health 36:325–344.https://doi.org/10.1146/annurev-publhealth-031914-122739
-
Closing the gap in a generation: health equity through action on the social determinants of healthFinal Report of the Commission on Social Determinants of Health. Rev Direito Sanitário 10:266.https://doi.org/10.11606/issn.2316-9044.v10i3p253-266
-
Mercury, selenium and fish oils in marine food webs and implications for human healthJournal of the Marine Biological Association of the United Kingdom 96:43–59.https://doi.org/10.1017/S0025315415001356
-
COVID-19-Zoonosis or Emerging Infectious Disease?Frontiers in Public Health 8:596944.https://doi.org/10.3389/fpubh.2020.596944
-
Social Work and Human Animal Bonds and Benefits in Health ResearchCritical Social Work 14:e873.https://doi.org/10.22329/csw.v14i1.5873
-
Human–animal interactions in livestock productionApplied Animal Behaviour Science 81:185–198.https://doi.org/10.1016/S0168-1591(02)00280-0
-
Blood mercury reporting in NHANES: identifying Asian, Pacific Islander, Native American, and multiracial groupsEnvironmental Health Perspectives 114:173–175.https://doi.org/10.1289/ehp.8464
-
The National Institute on Aging Health Disparities Research FrameworkEthnicity & Disease 25:245–254.https://doi.org/10.18865/ed.25.3.245
-
Planetary healthy publics after COVID-19The Lancet Planetary Health 5:e230–e236.https://doi.org/10.1016/S2542-5196(21)00050-4
-
The intersection of land use and human behavior as risk factors for zoonotic pathogen exposure in Laikipia County, KenyaPLOS Neglected Tropical Diseases 15:e0009143.https://doi.org/10.1371/journal.pntd.0009143
-
From Vaccine Nationalism to Vaccine Equity - Finding a Path ForwardNew England Journal of Medicine 384:1281–1283.https://doi.org/10.1056/NEJMp2103614
-
Breadth of the Socio-Ecological ModelJournal of Agromedicine 22:295–297.https://doi.org/10.1080/1059924X.2017.1358971
-
COVID-19: Magnifying the Effect of Health DisparitiesJournal of General Internal Medicine 35:2441–2442.https://doi.org/10.1007/s11606-020-05881-4
-
Climate Change and ObesityHormone and Metabolic Research 53:575–587.https://doi.org/10.1055/a-1533-2861
-
High adenovirus 36 seroprevalence among a population of Hispanic American youthInternational Journal of Adolescent Medicine and Health 33:e110.https://doi.org/10.1515/ijamh-2018-0110
-
A Comparison of Three Holistic Approaches to Health: One Health, EcoHealth, and Planetary HealthFrontiers in Veterinary Science 4:e63.https://doi.org/10.3389/fvets.2017.00163
-
Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, ChinaThe Science of the Total Environment 724:138226.https://doi.org/10.1016/j.scitotenv.2020.138226
-
Antimicrobial Resistance: a One Health PerspectiveMicrobiology Spectrum 6:e17.https://doi.org/10.1128/microbiolspec.ARBA-0009-2017
-
Transmission of SARS-CoV-2: A Review of Viral, Host, and Environmental FactorsAnnals of Internal Medicine 174:69–79.https://doi.org/10.7326/M20-5008
-
Encyclopedia of Case Study Research814–816, Research Framework, Encyclopedia of Case Study Research, SAGE Publications, Inc, 10.4135/9781412957397.
-
Natural Products as Sources of New Drugs over the Nearly Four Decades from 01/1981 to 09/2019Journal of Natural Products 83:770–803.https://doi.org/10.1021/acs.jnatprod.9b01285
-
Racial/Ethnic Disparities in Antimicrobial Drug Use, United States, 2014-2015Emerging Infectious Diseases 24:2126–2128.https://doi.org/10.3201/eid2411.180762
-
Diet Quality and Eating Practices among Hispanic/Latino Men and Women: NHANES 2011-2016International Journal of Environmental Research and Public Health 18:1302.https://doi.org/10.3390/ijerph18031302
-
Profiling a one-health model for priority populationsCanadian Journal of Public Health 107:e222–e223.https://doi.org/10.17269/cjph.107.5463
-
Links among human health, animal health, and ecosystem healthAnnual Review of Public Health 34:189–204.https://doi.org/10.1146/annurev-publhealth-031912-114426
-
Lifestyle and Clinical Correlates of Hepatocellular Carcinoma in South Texas: A Matched Case-control StudyClinical Gastroenterology and Hepatology 15:1311–1312.https://doi.org/10.1016/j.cgh.2017.03.022
-
Antibiotic resistance is the quintessential One Health issueTransactions of the Royal Society of Tropical Medicine and Hygiene 110:377–380.https://doi.org/10.1093/trstmh/trw048
-
Digestive tract colonization by multidrug-resistant Enterobacteriaceae in travellers: An updateTravel Medicine and Infectious Disease 21:28–35.https://doi.org/10.1016/j.tmaid.2017.11.007
-
Oxford Research Encyclopedia of Global Public Health“One Health” From Concept to Application in the Global World, Oxford Research Encyclopedia of Global Public Health, Oxford University Press, 10.1093/acrefore/9780190632366.013.29.
-
Mental Health Inequities in the Context of COVID-19JAMA Network Open 3:e2020104.https://doi.org/10.1001/jamanetworkopen.2020.20104
-
Human animal interface of SARS-CoV-2 (COVID-19) transmission: a critical appraisal of scientific evidenceVeterinary Research Communications 44:119–130.https://doi.org/10.1007/s11259-020-09781-0
-
One health disparities and COVID-19Evolution, Medicine, and Public Health 9:70–77.https://doi.org/10.1093/emph/eoab003
-
Human adenovirus-36 seropositivity and obesity among Midwestern US adolescentsInternational Journal of Adolescent Medicine and Health 32:126.https://doi.org/10.1515/ijamh-2017-0126
-
Climate change and gender-based health disparitiesThe Lancet Planetary Health 4:e44–e45.https://doi.org/10.1016/S2542-5196(20)30001-2
-
”Planetary Health” Perspectives and Alternative Approaches to Tackle the AMR ChallengeAntimicrobial Resistance: Global Challenges and Future Interventions 1:165–188.https://doi.org/10.1007/978-981-15-3658-8
-
Progress towards eliminating canine rabies: Policies and perspectives from Latin America and the CaribbeanPhilosophical Transactions of the Royal Society. Series B, Biological Sciences 368:20120143.https://doi.org/10.1098/rstb.2012.0143
-
Methicillin-resistant Staphylococcus aureus in pig farmingEmerging Infectious Diseases 11:1965–1966.https://doi.org/10.3201/eid1112.050428
-
Intensive livestock operations, health, and quality of life among eastern North Carolina residentsEnvironmental Health Perspectives 108:233–238.https://doi.org/10.1289/ehp.00108233
-
Bushmeat hunting, deforestation, and prediction of zoonoses emergenceEmerging Infectious Diseases 11:1822–1827.https://doi.org/10.3201/eid1112.040789
Decision letter
-
Peter RodgersSenior and Reviewing Editor; eLife, United Kingdom
In the interests of transparency, eLife publishes the most substantive revision requests and the accompanying author responses.
Decision letter after peer review:
Thank you for submitting your article "Proposed Incorporation of a One Health Approach in a Framework to Address Minority Health and Health Disparities" to eLife for consideration as a Feature Article. Your article has been reviewed by three peer reviewers, and their reports are detailed below. Two of the reviewers have also agreed to be named: Susan Craddock and Alissa Levine.
The reviewers and the eLife Features Editor (Peter Rodgers) have discussed the reviews and drafted this decision letter to help you prepare a revised submission.
As you will see from the reports, the reviewers had a number of concerns about how the article was written/structured, as well as some specific concerns about the content of the article. These specific concerns are listed below under the heading Essential Revisions.
The next step will be for a member of the eLife Features Team to edit the present version of the article, and then send the edited version to you so that you can check the edits, answer any queries, and address the specific concerns about the content listed below.
Summary:
This manuscript makes a convincing argument for adding two new components (links between human and other life forms, and the global context of health) to the research framework that is used by the National Institute on Minority Health and Health Disparities (NIMHD) to study health disparities. Consideration of these two elements will enable researchers to broaden their perspective and open new channels of scientific inquiry. However, there are a number of points that need to be addressed to make the article suitable for publication.
Essential revisions:
1. The One Health approach needs to be clearly explained near the start of the article.
2. Related to the previous point, please check that you need to use all of the following terms: "One Health concept", "One Health interventions", "One Health approach" and "One Health lens". If any of these terms are equivalent, please use just one of them.
3. In the definitions box, please define healthy disparity without referring to health disparities.
4. Line 207: One of the papers you cite (Solis and Nunn, One health disparities and COVID-19) covers very similar ground to your article. When you cite this article, please say more about its content and how it differs from your article.
5. Lines: 306-307: The way 'racial and ethnic groups' is being used needs some examination. If these individuals are from other countries as the authors suggest, then this can be very different than minority populations born and raised in the US, who typically are poorer than whites, more apt to live in polluted and degraded neighborhoods, and have worse health status. Many who fly back to home countries (South Asian communities are a good example but so too might some going back to Ethiopia or South Africa, etc.) are typically wealthier, better resourced, and have access to quality health care.
6. Performing a study that employs all the elements of the combined framework seems challenging, and possibly unfeasible. Please comment on this. Please also provide examples as to how this combined framework can be used in a single study
7. Given that the One Health and NIMHD frameworks are already being used by researchers, what are the advantages of combining them in a new framework?Reviewer #1 (Recommendations for the authors):
This article addresses an important – or potentially important – means of expanding explanations of health inequity. I agree with what the authors are arguing, but they need some pretty significant revisions before this is ready for publication.
In general, authors need to reorganize and tighten this article. The Introduction could flow better, and I don't think the opening definitions of theory versus framework are needed. Opening with some sort of statement on the importance of researching minority health and health equity issues from many perspectives (maybe even invoking covid from the beginning as the latest elucidation of health inequities and their multiple and interacting causes) rather than opening with definitions of framework versus theory would be more compelling.
The current NIMHD framework should first be elaborated, and subsequently authors should point out why it is inadequate to many compromised health situations from covid to AMR to obesity. Then, introduce the OH approach and be clear on what it is. Too often vague terms (resources, environment, food systems) are used rather than actual explanations of what the OH approach is, what it adds, etc. Then introduce all three of your examples. The current organization is confusing and discombobulated.
Finally, the authors' consistent parenthetical inclusion of what category or categories each facet fit into was ultimately distracting. I understand the need to make clear what facets a OH approach brings and in particular which facets are planetary and/or interspecies, but I would ponder dropping the categories – I think if the authors better explain what these facets are in a OH approach, their reader audience can figure out for themselves what is added in terms of the current NIMHD framework.
110-1: Elaborate on what is meant by human health's inextricable links to animal and environmental health. Provide some examples – that way, it makes more sense when you mention evaluating the impact of 'these interactions.' Without elaboration, it is not clear what kind of interactions you are talking about.
115-120: Some of these facets are self-explanatory, but several are not and they need to be explained. Conflicting priorities? Livelihood systems? Interactions in the environment? The examples provided starting at line 122 are good – provide more because this is important to your argument.
Though you subsequently invoke the covid pandemic to illustrate your argument for OH to be added to the current framework, you do need further elaboration on these interactions, providing more examples from how particular facets disproportionately impact marginalized populations. Your wildfire example, for instance, could happen to wealthier populations living in the hills surrounding urban areas in California.
205-207: Explain why exposure to bats, etc. happens more often to marginalized communities.
Is this the only example you provide from covid? Are there not many others you could provide?
209-217: this paragraph seems to be something of a grab-bag of facets, sone of which have more tentative connection to a OH approach – like vaccine equity. Could you take the animal ownership further?
246: This paragraph should go further up when 'interspecies' is first introduced.
In this section on AMR, what about antibiotics use in livestock and the fact that more marginalized communities subsequently consume this meat because livestock raised without antibiotics tends to be more expensive?
306-307: The way 'racial and ethnic groups' is being used needs some examination. If these individuals are from other countries as the authors suggest, then this can be very different than minority populations born and raised in the US, who typically are poorer than whites, more apt to live in polluted and degraded neighborhoods, and have worse health status. Many who fly back to home countries (South Asian communities are a good example but so too might some going back to Ethiopia or South Africa, etc.) are typically wealthier, better resourced, and have access to quality health care.
309-311: This needs further explanation – explain how waste is distributed and that this is one of many examples of environmental racism.Reviewer #2 (Recommendations for the authors):
This manuscript makes a convincing argument for incorporating two new components in the framework used to study health disparities: links between human and other life forms, and the global context of health. Consideration of these elements will enable researchers to broaden their perspective and open new channels of scientific inquiry.
1. The authors propose expanding the NIMHD framework to include interspecies and planetary considerations as posited in the One Health approach.
2. The authors draw on contemporary health concerns to convincingly convey the pertinence of incorporating the elements of the One Health approach into research on minority health and health disparities, for both infectious and non-communicable diseases.
3. This theoretically driven manuscript envisions broadening the application of interspecies and planetary frameworks to global contexts; the examples explored (Covid-19, antimicrobial resistance, and obesity) are each of clear global importance. The authors demonstrate how two additional multilayered dimensions enable a critical rethinking of health disparities.
4. The proposed framework will contribute to a more holistic perspective that seeks out interconnectivity among humans, other species, and their environments. This approach proposes a framework -the One Health lens-through which to imagine and engage in research and analysis. The community of researchers who already use the NIMHD framework can add these newly theorized dimensions to the existing framework, thereby broadening the scope of possible questions to be asked.
5. The useful glossary of terms (Definitions) provided at the outset could be expanded to include guidance on the varied terminology used to refer to One Health (One Health Approach, One Health paradigm, in addition to the One Health lens, which presumably provides a research-oriented operationalization). When introducing a novel way of framing research, the accompanying terms should help guide readers and researchers, providing a vocabulary with which to articulate and differentiate its parts.
Reviewer #3 (Recommendations for the authors):
This manuscript combines the One Health Model with the framework of the National Institute on Minority Health and Health Disparities (NIMHD) to develop a comprehensive framework viewing health disparities through the lens of socioecological and one health models. The authors rightly emphasize the need to understand the complex interactions of social and environmental factors when evaluating health disparities and the need for multidisciplinary collaborations in these fields. The authors present comprehensive tables in the manuscript indicating how the One Health Model can be combined with the NIMHD model and how this adapted model can be used in health disparities research, with examples from antimicrobial resistance (AMR) and obesity. Yet, modifications are needed to render this manuscript suitable for publication. Below are some of my comments:
1. Some of the published literature advance arguments that are similar to what have been pointed out in this study. For example, an article exists that has combined the One Health Model with the NIMHD constructs; the resulted model is labelled « One Health Disparities ». The authors of this article have explained their One Health Disparities model using the COVID-19 pandemic. (Here is the link to the paper: https://doi.org/10.1093/emph/eoab003). Given that the current manuscript draws on combining the One Health Model and NIMHD in the context of COVID19, the authors need to explain how their paper adds to the literature.
2. While looking at the complex interactions between the elements of the adapted model can definitely be useful, I am concerned about the feasibility of such an effort. I believe one cannot evaluate all these factors and their interactions within one study; only a segment of this fulsome framework can be used in a single study. Given that each of the One Health Model and the NIMHD frameworks are being currently used in separate studies regarding health disparities, AMR and obesity, how can a comprehensive framework with all these factors embedded be helpful?
3. Providing definitions of major concepts included in a research paper is good practice. However, some of the definitions provided are slightly vague. For instance, the authors define health disparities as « a difference in health outcomes adversely affecting populations with health disparities in comparison to a reference group. » This definition is confusing because the authors have used the term « health disparities » in the definition of health disparities. Clear definitions of the concepts included in this manuscript can significantly improve the quality of this work.
4. Some of the interrelationships between the elements of the adapted framework seem to be based on assumptions. While the authors have adequately referenced their statements, it would improve the transparency of this manuscript if the authors provide evidence supporting these assumptions in the text of the manuscript.
https://doi.org/10.7554/eLife.76461.sa1Author response
Essential revisions:
1. The One Health approach needs to be clearly explained near the start of the article.
The introduction was adjusted to explain the One health approach more thoroughly. Specifically, we introduce One Health at the end of the introduction and discuss the One Health approach, including examples of how it has been leveraged previously, in the first paragraph under Health Disparities and One Health (Line 90).
2. Related to the previous point, please check that you need to use all of the following terms: "One Health concept", "One Health interventions", "One Health approach" and "One Health lens". If any of these terms are equivalent, please use just one of them.
We updated the manuscript with the term One Health approach throughout to reduce confusion.
3. In the definitions box, please define healthy disparity without referring to health disparities.
We have updated the definition of health disparity in the definitions box to,
“A difference in health outcomes adversely affecting socially and/or economically disadvantaged populations that have been exposed to racism or discrimination and have been underserved in health care, in comparison to a reference group.”
4. Line 207: One of the papers you cite (Solis and Nunn, One health disparities and COVID-19) covers very similar ground to your article. When you cite this article, please say more about its content and how it differs from your article.
The Solis and Nunn study use the NIMHD framework to demonstrate that social environments are important to zoonotic disease researchers investigating disparities in rates of transmission, susceptibility, and spillover/spillback in populations. They term these “One Health disparities.” Our paper is expanding the NIMHD framework for researchers outside of One health to begin thinking about the ways human-animal and human-environmental relationships influence health disparities broadly. We addressed the difference between ours and the previous study at line 209-213.
5. Lines: 306-307: The way 'racial and ethnic groups' is being used needs some examination. If these individuals are from other countries as the authors suggest, then this can be very different than minority populations born and raised in the US, who typically are poorer than whites, more apt to live in polluted and degraded neighborhoods, and have worse health status. Many who fly back to home countries (South Asian communities are a good example but so too might some going back to Ethiopia or South Africa, etc.) are typically wealthier, better resourced, and have access to quality health care.
We thank the reviewer for pointing out the nuances of this argument and allowing us to clarify our intent. The idea behind this determinant is that individuals traveling more frequently to foreign countries are at increased risk of contact with and contracting AMR bacteria endemic in those areas. They also transfer and carry those pathogens back to the US and their communities. To address and clarify this, we changed ‘racial and ethnic groups’ to immigrant populations at line 286. Further, we added why frequent travel to home countries may present increased risk at line 287.
In addition, many working class immigrants do travel to their home countries especially within the Americas. The proximity of Mexico, the seasonal nature of employment in some cases, and the continued strong bonds with family and place drive this need to return. Immigrants are frequently earning incomes that are several times higher than their families in the home country. Finally, the self-identified construct of race and ethnicity does have global application even if the categories will vary according to region.
6. Performing a study that employs all the elements of the combined framework seems challenging, and possibly unfeasible. Please comment on this. Please also provide examples as to how this combined framework can be used in a single study
We agree performing a study that employs all the elements of the combined framework would likely be impossible. The intent behind the framework is to help guide researchers in developing multilevel and multidimensional studies, understand what the domain and level of influence of their study is at, and to consider what factors may be influencing their findings (even if they can’t measure or quantify it). It also helps understand the broader landscape in which a study is situated. We clarified this intent in the introduction of the paper at line 51 and an example of how the framework has been used follows at line 55.
7. Given that the One Health and NIMHD frameworks are already being used by researchers, what are the advantages of combining them in a new framework?
This is an excellent question. Briefly, we discuss in the paper the benefits of incorporating the One Health approach to the NIMHD framework (addressing health disparities holistically, opening new avenues of inquiry, and promote multidisciplinary collaborations – line 140). We also added a sentence at line 150 to 153 to highlight how the work by One Health researchers and health disparities researchers is conducted in disciplinary silos and how the expanded framework may highlight the overlap in their work and stimulate new ideas.
https://doi.org/10.7554/eLife.76461.sa2Article and author information
Author details
Funding
No external funding was received for this work.
Publication history
- Received: December 17, 2021
- Accepted: June 28, 2022
- Version of Record published: July 7, 2022 (version 1)
Copyright
This is an open-access article, free of all copyright, and may be freely reproduced, distributed, transmitted, modified, built upon, or otherwise used by anyone for any lawful purpose. The work is made available under the Creative Commons CC0 public domain dedication.
Metrics
-
- 1,009
- views
-
- 150
- downloads
-
- 2
- citations
Views, downloads and citations are aggregated across all versions of this paper published by eLife.
Download links
Downloads (link to download the article as PDF)
Open citations (links to open the citations from this article in various online reference manager services)
Cite this article (links to download the citations from this article in formats compatible with various reference manager tools)
Further reading
-
- Cancer Biology
- Epidemiology and Global Health
Background:
Age is the most important risk factor for cancer, but aging rates are heterogeneous across individuals. We explored a new measure of aging-Phenotypic Age (PhenoAge)-in the risk prediction of site-specific and overall cancer.
Methods:
Using Cox regression models, we examined the association of Phenotypic Age Acceleration (PhenoAgeAccel) with cancer incidence by genetic risk group among 374,463 participants from the UK Biobank. We generated PhenoAge using chronological age and nine biomarkers, PhenoAgeAccel after subtracting the effect of chronological age by regression residual, and an incidence-weighted overall cancer polygenic risk score (CPRS) based on 20 cancer site-specific polygenic risk scores (PRSs).
Results:
Compared with biologically younger participants, those older had a significantly higher risk of overall cancer, with hazard ratios (HRs) of 1.22 (95% confidence interval, 1.18–1.27) in men, and 1.26 (1.22–1.31) in women, respectively. A joint effect of genetic risk and PhenoAgeAccel was observed on overall cancer risk, with HRs of 2.29 (2.10–2.51) for men and 1.94 (1.78–2.11) for women with high genetic risk and older PhenoAge compared with those with low genetic risk and younger PhenoAge. PhenoAgeAccel was negatively associated with the number of healthy lifestyle factors (Beta = –1.01 in men, p<0.001; Beta = –0.98 in women, p<0.001).
Conclusions:
Within and across genetic risk groups, older PhenoAge was consistently related to an increased risk of incident cancer with adjustment for chronological age and the aging process could be retarded by adherence to a healthy lifestyle.
Funding:
This work was supported by the National Natural Science Foundation of China (82230110, 82125033, 82388102 to GJ; 82273714 to MZ); and the Excellent Youth Foundation of Jiangsu Province (BK20220100 to MZ).
-
- Epidemiology and Global Health
Paxlovid, a SARS-CoV-2 antiviral, not only prevents severe illness but also curtails viral shedding, lowering transmission risks from treated patients. By fitting a mathematical model of within-host Omicron viral dynamics to electronic health records data from 208 hospitalized patients in Hong Kong, we estimate that Paxlovid can inhibit over 90% of viral replication. However, its effectiveness critically depends on the timing of treatment. If treatment is initiated three days after symptoms first appear, we estimate a 17% chance of a post-treatment viral rebound and a 12% (95% CI: 0%-16%) reduction in overall infectiousness for non-rebound cases. Earlier treatment significantly elevates the risk of rebound without further reducing infectiousness, whereas starting beyond five days reduces its efficacy in curbing peak viral shedding. Among the 104 patients who received Paxlovid, 62% began treatment within an optimal three-to-five-day day window after symptoms appeared. Our findings indicate that broader global access to Paxlovid, coupled with appropriately timed treatment, can mitigate the severity and transmission of SARS-Cov-2.







