Meta-Research: Why we need to report more than 'Data were Analyzed by t-tests or ANOVA'
- Article
- Figures and data
- Abstract
- Introduction
- Can we determine which type of ANOVA was performed?
- Can we determine what type of t-test was performed?
- Papers rarely contain information needed to verify the test result
- Moving towards a more transparent and reproducible future
- Materials and methods
- Data availability
- References
- Decision letter
- Author response
- Article and author information
- Metrics
Abstract
Transparent reporting is essential for the critical evaluation of studies. However, the reporting of statistical methods for studies in the biomedical sciences is often limited. This systematic review examines the quality of reporting for two statistical tests, t-tests and ANOVA, for papers published in a selection of physiology journals in June 2017. Of the 328 original research articles examined, 277 (84.5%) included an ANOVA or t-test or both. However, papers in our sample were routinely missing essential information about both types of tests: 213 papers (95% of the papers that used ANOVA) did not contain the information needed to determine what type of ANOVA was performed, and 26.7% of papers did not specify what post-hoc test was performed. Most papers also omitted the information needed to verify ANOVA results. Essential information about t-tests was also missing in many papers. We conclude by discussing measures that could be taken to improve the quality of reporting.
https://doi.org/10.7554/eLife.36163.001Introduction
The inability to reproduce key scientific results in certain areas of research is a growing concern among scientists, funding agencies, journals and the public (Nature, 2013; Fosang and Colbran, 2015; National Institutes of Health, 2015a; National Institutes of Health, 2015b; Nature, 2017). Problems with the statistical analyses used in published studies, along with inadequate reporting of the experimental and statistical techniques employed in the studies, are likely to have contributed to these concerns. Older studies suggest that statistical errors, such as failing to specify what test was used or using incorrect or suboptimal statistical tests, are common (Müllner et al., 2002; Ruxton, 2006; Strasak et al., 2007), and more recent studies suggest that these problems persist. A study published in 2011 found that half of the neuroscience articles published in five top journals used inappropriate statistical techniques to compare the magnitude of two experimental effects (Nieuwenhuis et al., 2011). A more recent study of papers reporting the results of experiments that examined the effects of prenatal interventions on offspring found that the statistical analyses in 46% of the papers were invalid because authors failed to account for non-independent observations (i.e., animals from the same litter; Lazic et al., 2018). Many studies omit essential details when describing experimental design or statistical methods (Real et al., 2016; Lazic et al., 2018). Errors in reported p-values are also common and can sometimes alter the conclusions of a study (Nuijten et al., 2016).
A main principle of the SAMPL guidelines for reporting statistical analyses and methods in the published literature is that authors should "describe statistical methods with enough detail to enable a knowledgeable reader with access to the original data to verify the reported results" (Lang and Altman, 2013). However, these guidelines have not been widely adopted.
Clear statistical reporting also allows errors to be identified and corrected prior to publication. The journal Science has attempted to improve statistical reporting by adding a Statistical Board of Reviewing Editors (McNutt, 2014). Other journals, including Nature and affiliated journals (Nature, 2013; Nature, 2017), eLife (Teare, 2016) and The EMBO Journal (EMBO Press, 2017) have recently implemented policies to encourage transparent statistical reporting. These policies may include specifying which test was used for each analysis, reporting test statistics and exact p-values, and using dot plots, box plots or other figures that show the distribution of continuous data.
T-tests and analysis of variance (ANOVA) are the statistical bread-and-butter of basic biomedical science research (Strasak et al., 2007). However, statistical methods in these papers are often limited to vague statements such as: "Data were analyzed by t-tests or ANOVA, as appropriate, and statistical significance was defined as p<0.05." There are several problems with such descriptions. First, there are many different types of t-tests and ANOVAs. Vague statistical methods deprive reviewers, editors and readers of the opportunity to confirm that an appropriate type of t-test or ANOVA was used and that the results support the conclusions in the paper. For example, if authors use an unpaired t-test when a paired t-test is needed, the failure to account for repeated measurements on the same subject will lead to an incorrect p-value. Analyses that use inappropriate tests give potentially misleading results because the tests make incorrect assumptions about the study design or data and often test the wrong hypothesis. Without the original data, it is difficult to determine how the test results would have been different had an appropriate test been used. Clear reporting allows readers to confirm that an appropriate test was used and makes it easier to identify and fix potential errors prior to publication.
The second problem is that stating that tests were used "as appropriate" relies on the assumption that others received similar statistical training and would make the same decisions. This is problematic because it is possible to complete a PhD without being trained in statistics: only 67.5% of the top NIH-funded physiology departments in the United States required statistics training for some or all PhD programs that the department participated in (Weissgerber et al., 2016a). When training is offered, course content can vary widely among fields, institutions and departments as there are no accepted standards for the topics that should be covered or the level of proficiency required. Moreover, courses are rarely designed to meet the needs of basic scientists who work with small sample size datasets (Vaux, 2012; Weissgerber et al., 2016a). Finally, these vague statements fail to explain why t-tests and ANOVA were selected, as opposed to other techniques that can be useful for small sample size datasets.
This systematic review focuses on the quality of reporting for ANOVA and t-tests, which are two of the most common statistical tests performed in basic biomedical science papers. Our objectives were to determine whether articles provided sufficient information to determine which type of ANOVA or t-test was performed and to verify the test result. We also assessed the prevalence of two common problems: i) using a one-way ANOVA when the study groups could be divided into two or more factors, and ii) not specifying that the analysis included repeated measures or within-subjects factors when ANOVA was performed on non-independent or longitudinal data.
To obtain our sample two reviewers independently examined all original research articles published in June 2017 (n = 328, Figure 1) in the top 25% of physiology journals, as determined by 2016 journal impact factor (see Methods for full details). Disagreements were resolved by consensus. 84.5% of the articles (277/328) included either a t-test or an ANOVA, and 38.7% of articles (127/328) included both. ANOVA (n = 225, 68.6%) was more common than t-tests (n = 179, 54.5%). Among papers that reported the number of factors for at least one ANOVA, most were using a maximum of one (n = 112, 49.8%) or two (n = 69, 30.7%) factors. ANOVAs with three or more factors were uncommon (n = 6, 2.7%). This approach involved a number of limitations. All the journals in our sample were indexed in PubMed and only published English language articles, so our results may not be generalizable to brief reports, journals with lower impact factors, journals that publish articles in other languages, or journals that are not indexed in PubMed. Further research is also needed to determine if statistical reporting practices in other fields are similar to what we found in physiology.
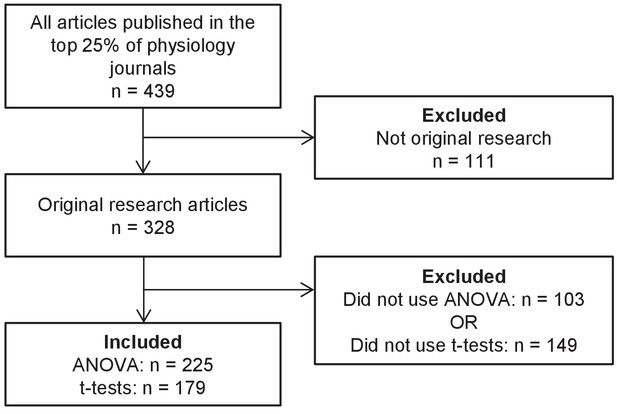
Systematic review flow chart.
The flow chart illustrates the selection of articles for inclusion in this analysis at each stage of the screening process.
-
Figure 1—source data 1
Data from systematic review.
- https://doi.org/10.7554/eLife.36163.003
Can we determine which type of ANOVA was performed?
While ANOVA encompasses a wide variety of techniques, basic biomedical science papers generally use one and two-way ANOVAs, with or without repeated measures. We focused on reporting requirements for these basic tests, as more complex types of ANOVA were rare in our dataset (<3%; Figure 1—source data 1). Authors need to report three key pieces of information to allow readers to confirm that the type of ANOVA that was used is appropriate for the study design (see Box 1 for terminology and Box 2 for a detailed description of what should be reported). Many papers were missing some or all of this information (Figure 2). 213 papers (95% of the papers that used ANOVA) did not contain all information needed to determine what type of ANOVA was performed, including the names and number of factors and whether each factor was entered as a between-subjects or within-subjects factor.
Box 1.
ANOVA terminology
# ANOVA examines the effect of one or more categorical independent variables, known as 'factors', on a dependent variable. Examples of factors might include age (young vs. old), hypertension (hypertensive vs. normotensive) or time since drug administration (baseline, 1 hour, 6 hours, 12 hours, and 24 hours).
# The groups or conditions within each factor are called levels. In the example above, age has two levels (young vs. old), hypertension has two levels, and time since drug administration has five levels.
# Each factor can be entered into the ANOVA as a between-subjects factor or a within-subjects factor. Measurements on unrelated participants, specimens or samples (i.e., age, hypertension) are entered into the ANOVA as between-subjects factors. Longitudinal measurements (i.e., time since drug administration) are entered into the analysis as within-subjects factors.
# Other types of non-independent measurements may also be entered as within-subjects factors. This includes related measurements that are performed in the same participants (i.e., arm vs. leg), or groups in which subjects are matched (i.e., normotensive and hypertensive participants matched for sex and age).
# An ANOVA that includes at least one within-subjects factor is called repeated measures ANOVA.
# A repeated-measures ANOVA with two or more factors may include between-subjects factors, depending on the study design. For example, a two-way repeated measures ANOVA with one between and one within-subjects factor might be used for a study in which men and women completed four weeks of exercise training. Sex (female vs. male) would be a between-subjects factor, whereas exercise training (baseline vs. post-training) would be a within-subjects factor. A two-way repeated measures ANOVA with two within-subjects factors might be used for a study in which vascular function was measured in both arms (right vs. left), before and after 4 weeks of right arm handgrip training (baseline vs. post-training).
# Post-hoc tests are used to determine which groups in the ANOVA differ from each other. These tests are used when p-values for the ANOVA show that there is a significant effect of any factor, or a significant interaction between two or more factors. There are many different types of post-hoc tests. These tests use different procedures to determine which groups to compare and adjust for multiple comparisons; some are more conservative than others.
https://doi.org/10.7554/eLife.36163.004Box 2.
Checklist for clear statistical reporting for t-tests and ANOVAs
Basic biomedical science studies often include several small experiments. Providing information about statistical tests in the legend of each table or figure makes it easy for readers to determine what test was performed for each set of data and confirm that the test is appropriate.
t-tests
# State whether the test was unpaired (for comparing independent groups) or paired (for non-independent data, including repeated measurements on the same individual or matched participants, specimens or samples).
# State whether the test assumed equal or unequal variance between groups.
# Report the t-statistic, degrees of freedom and exact p-value.
# To focus on the magnitude of the difference, it is strongly recommended to report effect sizes with confidence intervals.
ANOVAs
# Specify the number of factors included in the ANOVA (i.e., one- vs. two-way ANOVA).
# For each factor, specify the name and level of the factor and state whether the factor was entered as a within-subjects (i.e., independent) factor or as a between-subjects (i.e., non-independent) factor.
# If the ANOVA has two or more factors, specify whether the interaction term was included. If the ANOVA has three or more factors and includes interaction terms, specify which interaction terms were included.
# Report the F-statistic, degrees of freedom and exact p-value for each factor or interaction.
# Specify if a post-hoc test was performed. If post-hoc tests were performed, specify the type of post-hoc test and, if applicable, the test statistic and p-value.
# To focus on the magnitude of the difference, it is strongly recommended to report effect sizes with confidence intervals.
https://doi.org/10.7554/eLife.36163.005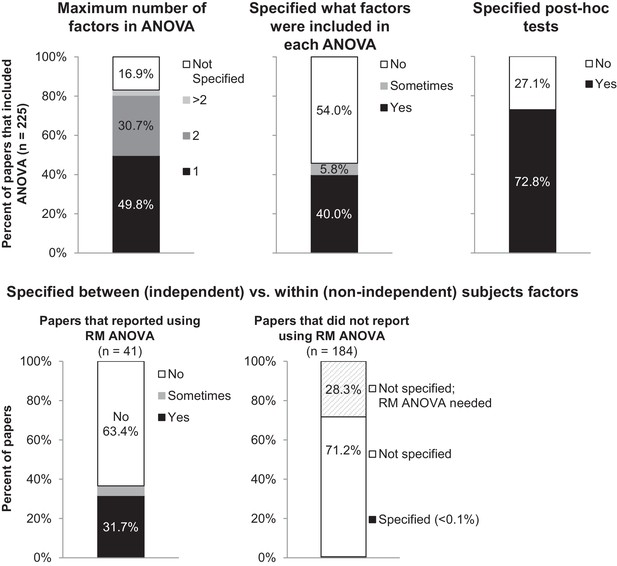
Many papers lack the information needed to determine what type of ANOVA was performed.
The figure illustrates the proportion of papers in our sample that reported information needed to determine what type of ANOVA was performed, including the number of factors, the names of factors, and the type of post-hoc tests. The top panel presents the proportion of all papers that included ANOVA (n = 225). 'Sometimes' indicates that the information was reported for some ANOVAs but not others. The bottom row examines the proportion of papers that specified whether each factor was between vs. within-subjects. Papers are subdivided into those that reported using repeated measures ANOVA (n = 41), and those that did not report using repeated measures ANOVA (n = 184). RM: repeated measures.
The number of factors included in the ANOVA and the names and levels of each factor
16.9% of papers (38/225) failed to specify how many factors were included for any ANOVA performed in the paper. 54% of papers did not specify which factors were included in any ANOVA, whereas fewer than half of papers specified which factors were included for some (n = 13, 5.8%) or all (n = 90, 40%) ANOVAs reported in the manuscript.
Our data suggest that reporting the number, names and levels of factors may be particularly important to determine whether the statistical test is appropriate for the study design. Among papers that used one-way ANOVAs, 60.9% (67/110) used a one-way ANOVA for an analysis where the study design included two or more factors. (Note: Two papers that reported using a maximum of one factor in the ANOVA were excluded, as these papers also included a repeated measures ANOVA with an unknown number of factors.) For example, investigators might have used a one-way ANOVA to compare four independent groups: wild-type mice that received vehicle (placebo), wild-type mice that received a treatment, knockout mice that received vehicle (placebo), and knockout mice that received a treatment. This approach may be appropriate for extremely small sample sizes, as these datasets may not have enough power for an ANOVA with two or more factors. In most cases, however, a two-way ANOVA with mouse strain (wild-type vs. knockout) and treatment (placebo vs. treatment) as factors may provide more information. Figure 3 and Figure 4 show the difference between these two approaches and illustrate how the two-way ANOVA may offer additional insight. The two-way ANOVA allows investigators to examine the effects of both factors simultaneously and may help investigators to avoid unnecessary post-hoc tests. If the sample size is large enough, the two-way ANOVA can test for an interaction between the two factors (i.e., whether the effect of mouse strain depends on treatment).
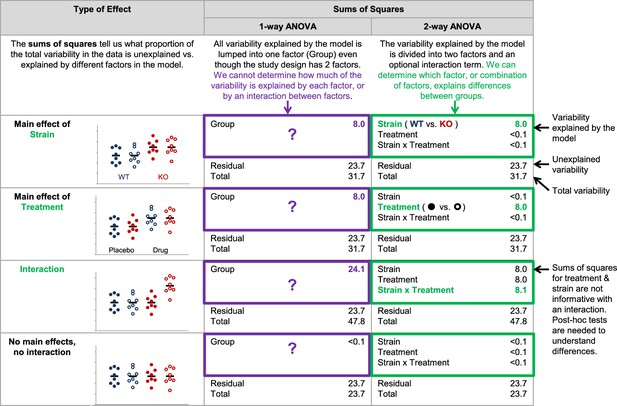
Why it matters whether investigators use a one-way vs two-way ANOVA for a study design with two factors.
The two-way ANOVA allows investigators to determine how much of the variability explained by the model is attributed to the first factor, the second factor, and the interaction between the two factors. When a one-way ANOVA is used for a study with two factors, this information is missed because all variability explained by the model is assigned to a single factor. We cannot determine how much variability is explained by each of the two factors, or test for an interaction. The simulated dataset includes four groups – wild-type mice receiving placebo (closed blue circles), wild-type mice receiving an experimental drug (open blue circles), knockout mice receiving placebo (closed red circles) and knockout mice receiving an experimental drug (open red circles). The same dataset was used for all four examples, except that means for particular groups were shifted to show a main effect of strain, a main effect of treatment, and interaction between strain and treatment or no main effects and no interaction. One- and two-way (strain x treatment) ANOVAs were applied to illustrate differences between how these two tests interpret the variability explained by the model.
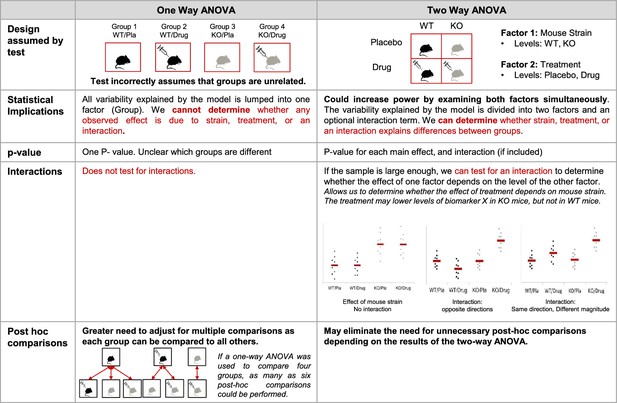
Additional implications of using a one-way vs two-way ANOVA.
This figure compares key features of one- and two-way ANOVAs to illustrate potential problems with using a one-way ANOVA for a design with two or more factors. When used for a study with two factors, the one-way ANOVA incorrectly assumes that the groups are unrelated, generates a single p-value that does not provide information about which groups are different, and does not test for interactions. The two-way ANOVA correctly interprets the study design, which can increase power. The two-way ANOVA also allows for the generation of a set of p-values that provide more information about which groups may be different, can test for interactions, and may eliminate the need for unnecessary post-hoc comparisons. This figure uses an experimental design with four groups (wild-type mice receiving placebo, wild-type mice receiving an experimental drug, knockout mice receiving placebo and knockout mice receiving an experimental drug). See Figure 2 for a detailed explanation of the material in the statistical implications section. KO: knockout; WT: wild-type; Pla: placebo.
Whether each factor was entered as a between (independent) or within (non-independent) subjects factor
Among the 18.2% of papers (41/225) that reported using repeated measures ANOVA, 63.4% (n = 26) did not specify whether each factor was entered as a between or within-subjects factor. Many of the 15 papers that provided adequate information reported using one-way repeated measures ANOVA. When the ANOVA only includes one factor, stating that repeated measures were used demonstrates that this factor was treated as a within-subjects or non-independent factor. When a repeated measures ANOVA includes two or more factors, however, authors need to clearly report which factors were treated as between vs. within-subjects factors. A two-way repeated measures ANOVA could refer to two different tests – an ANOVA with two within-subjects factors, or an ANOVA with one within-subjects factor and one between-subjects factor (Box 1).
The remaining 81.8% of papers that included ANOVA did not indicate whether repeated measures were used. Only one of these papers stated that all factors were entered as between-subjects factors (1/184, 0.5%). If repeated measures or within-subjects factors are not mentioned, one would typically assume that all factors were independent or between-subjects. Our data suggest that scientists should be cautious about this assumption, as 28.3% of papers that did not indicate that repeated measures were used (52/184) included at least one ANOVA that appeared to require repeated measures. There is no way to distinguish between papers that used the wrong test and papers that failed to clearly specify which test was used. Figure 5 illustrates the differences between these two tests. Failing to account for repeated measures in an ANOVA makes it less likely that investigators will detect an effect, as the variability that can be attributed to individual subjects remains unexplained. To avoid confusion, we recommend that reviewers, editors and journal guidelines encourage authors to specify whether each factor was entered as between or within-subjects factor, even if the paper does not include a repeated measures ANOVA.
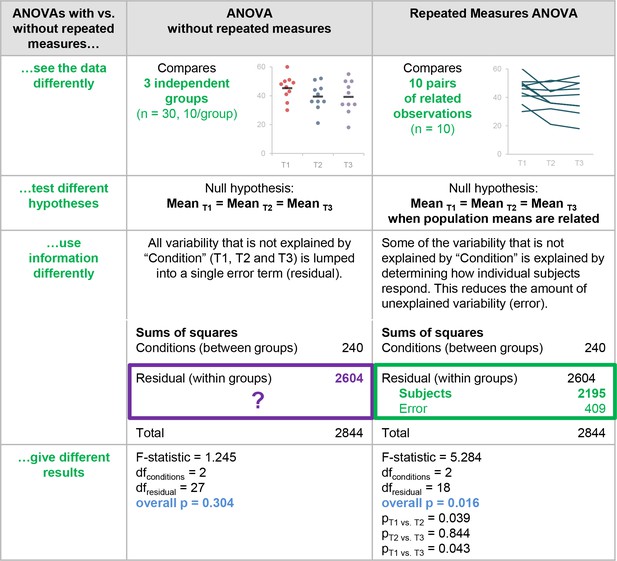
Why it matters whether investigators used an ANOVA with vs. without repeated measures.
This figure highlights the differences between ANOVA with vs. without repeated measures and illustrates the problems with using an ANOVA without repeated measures when the study design includes longitudinal or non-independent measurements. These two tests interpret the data differently, test different hypotheses, use information differently when calculating the test statistic, and give different results.
The type of post-hoc test that was performed
Clear reporting of post-hoc testing procedures allows readers to determine how the authors decided whether to use post-hoc tests, what type of post-hoc tests were performed and whether the tests results were adjusted for multiple comparisons. 72.8% of papers (164/225) stated what test was used to examine pairwise differences after performing an ANOVA (such as Tukey and Bonferroni). The remaining 27.1% of papers (61/225) did not specify what type of post-hoc tests were performed.
Can we determine what type of t-test was performed?
Many of the 179 papers that included a t-test were missing information that was needed to determine what type of t-test was performed, including whether the tests were paired or unpaired, or assumed equal or unequal variance.
Unpaired vs. paired t-tests
Over half of the papers (53%; 95/179) did not specify whether any t-tests were paired or unpaired; a small proportion (2.2%; 4/179) provided this information for some but not all of the t-tests in the paper. 69 of the 95 papers without any information on paired vs. unpaired t-tests reported that the Student’s t-test was used. While the term Student’s t-test traditionally refers to the unpaired t-test for equal variances, we identified numerous instances where authors referred to a paired t-test as a Student’s t-test. Due to this confusion, we did not assume that the Student’s t-test was unpaired unless the authors included additional terms like unpaired t-test or independent samples t-test. Figure 6 illustrates why clear reporting that allows readers to confirm that the correct test was used is essential. Unpaired and paired t-tests interpret the data differently, test different hypotheses, use different information to calculate the test statistic and usually give different results. If the incorrect test is used, the analysis tests the wrong hypothesis and the results may be misleading. Without the original data, it is difficult to determine how the test results would have been different had the appropriate tests been used.For example, differencesbetween the results of the paired and unpaired t-tests depend on the strength of the correlation between paired data points (Figure 7), which is difficult or impossible to determine from line graphs that only show summary statistics.
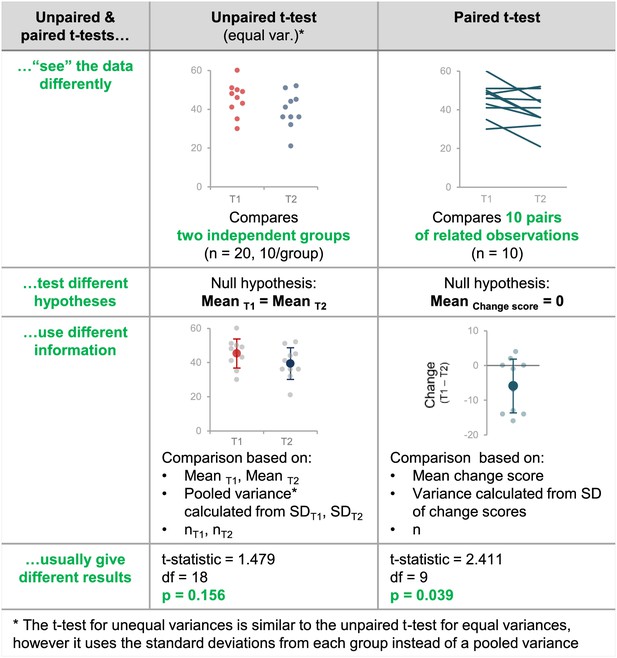
Why papers need to contain sufficient detail to confirm that the appropriate t-test was used.
This figure highlights the differences between unpaired and paired t-tests by illustrating how these tests interpret the data differently, test different hypotheses, use information differently when calculating the test statistic, and give different results. If the wrong t-test is used, the result may be misleading because the test will make incorrect assumptions about the experimental design and may test the wrong hypothesis. Without the original data, it is very difficult to determine what the result should have been (see Figure 6).
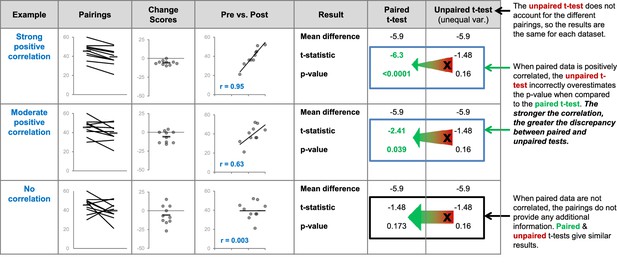
Differences between the results of statistical tests depend on the data.
The three datasets use different pairings of the values shown in the dot plot on the left. The comments on the right side of the figure illustrate what happens when an unpaired t-test is inappropriately used to compare paired, or related, measurements. We expect paired data to be positively correlated – two paired observations are usually more similar than two unrelated observations. The strength of this correlation will vary. We expect observations from the same participant to be more similar (strongly correlated) than observations from pairs of participants matched for age and sex. Stronger correlations result in greater discrepancies between the results of the paired and unpaired t-tests. Very strong correlations between paired data are unusual but are presented here to illustrate this relationship. We do not expect paired data to be negatively correlated – if this happens it is important to review the experimental design and data to ensure that everything is correct.
Equal vs. unequal variance
When using unpaired t-tests, it is important to specify whether the test assumes that the variance is equal in both groups. The unpaired Student’s t-test (also called the t-test for equal variances) assumes that the variance is similar in both groups, whereas the Welch’s t-test (the t-test for unequal variances) assumes that variance differs between the two groups. If the variance is not estimated appropriately, the type I error is actually higher than advertised; this means that the null hypothesis is falsely rejected more often (Ruxton, 2006). Among the 155 papers that included unpaired t-tests, 64.5% (100/155) reported whether the test assumed equal variance for all unpaired t-tests and 6.5% (10/155) provided this information for some unpaired tests.
Papers rarely contain information needed to verify the test result
Reporting the test statistic (ANOVA: F-statistic, t-tests: t-statistic), degrees of freedom and exact p-values are important for several reasons. First, these values allow authors, reviewers and editors to confirm that the correct test was used. This is particularly important when the statistical methods do not provide enough information to determine which type of ANOVA or t-test was performed, which was common in our dataset. Second, reporting the degrees of freedom allows readers to confirm that no participants, animals or samples were excluded without explanation. A recent study found that more than two thirds of papers using animal models to study stroke or cancer did not contain sufficient information to determine whether animals were excluded, while 7-8% of papers excluded animals without explanation (Holman et al., 2016). Biased exclusion of animals or observations can substantially increase the probability of false positive results in small sample size studies. Third, this information allows authors and readers to verify the test result. In an analysis of psychology papers, over half reported at least one p-value that did not match the test statistic and degrees of freedom: this error was sufficient to alter the study conclusions in one out of eight papers (Nuijten et al., 2016). Authors and journal editors can eliminate these errors by double checking their results, or using software programs such as statcheck (Eskamp and Nuijten, 2016) to confirm that p-values match the reported test statistic and degrees of freedom. Unfortunately, the information needed to verify the test result is not reported in many papers.
Among the studies in our sample that included ANOVA (Figure 8), more than 95% failed to report the F-statistic or degrees of freedom. Moreover, 77.8% of these papers reported ranges of p-values (i.e., p>0.05, p<0.05, p<0.01), with just 50 papers reporting exact p-values (41 of 225 papers reported exact p-values for some ANOVAs, and 9 papers reported exact p-values for all ANOVAs). Among studies that included t-tests, 16 papers (8.9%) were excluded because abstractors were unable to determine what data were analyzed by t-tests or to identify a two-group comparison. While most papers reported the sample size or degrees of freedom for some (16.6%) or all (76.7%) t-tests, t-statistics were missing from 95.7% of papers (Table 1). Moreover, 79.7% of the papers that included t-tests reported ranges of p-values instead of exact p-values.
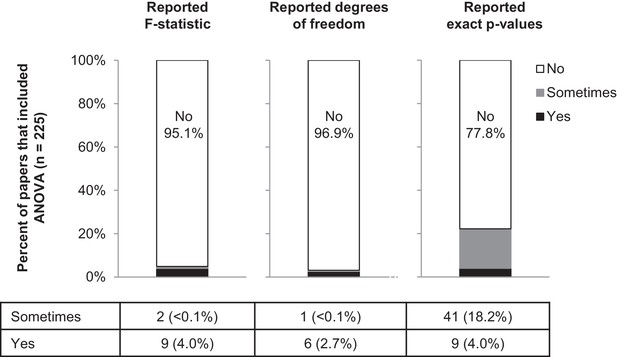
Few papers report the details needed to confirm that the result of the ANOVA was correct.
This figure reports the proportion of papers with ANOVAs (n = 225) that reported the F-statistic, degrees of freedom and exact p-values. Sometimes indicates that the information was reported for some ANOVAs contained in the paper but not for others.
Reporting of details needed to verify the results of a t-test.
https://doi.org/10.7554/eLife.36163.013| Reported t-statistic | Reported exact sample size or degrees of freedom | Reported exact p-values | |
|---|---|---|---|
| No | 156 (95.7%) | 11 (6.7%) | 113 (69.3%) |
| Sometimes | 0 | 27 (16.6%) | 17 (10.4%) |
| Yes | 7 (4.3%) | 125 (76.7%) | 33 (20.2%) |
-
We analyzed the 179 papers in our sample that included t-tests to check if they reported the details that are needed to verify the results of these tests: we had to exclude 16 papers from this analysis because we were unable to determine what data were analyzed by t-tests or to identify a two-group comparison. Most of the papers (95.7%; 156/163) did not report the t-statistic (column 2) and over two-thirds (69.3%; 113/163) did not report exact p-values (column 4), but over three-quarters (76.7%; 125/163) reported the exact sample size or degree of freedom for all of the t-tests in the paper (column 3).
Moving towards a more transparent and reproducible future
This systematic review demonstrates that t-tests and ANOVA may not be so simple after all, as many papers do not contain sufficient information to determine why a particular test was selected, what type of test was used or to verify the test result. Selecting statistical tests that are not appropriate for the study design may be surprisingly common. Often, it is not possible to determine why statistical tests were selected, or whether other analyses may have provided more insight. Investigators frequently present data using bar or line graphs that only show summary statistics (Weissgerber et al., 2015) and raw data are rarely available. Many journals have recently introduced policies to encourage more informative graphics, such as dot plots, box plots or violin plots, that show the data distribution (Nature, 2017; Fosang and Colbran, 2015; Kidney International, 2017; PLOS Biology, 2016; Teare, 2016) and may provide insight into whether other tests are needed. Non-parametric tests, such as the Mann-Whitney U test, Wilcoxon sign rank test and Kruskal Wallis test, may sometimes be preferable as sample sizes in basic biomedical science research are often too small to determine the data distribution. However, these tests are not commonly used. A systematic review of physiology studies showed that 3.8% used only non-parametric tests to compare continuous data, 13.6% used a combination of parametric and non-parametric tests, and 78.1% of studies used only parametric tests (Weissgerber et al., 2015). A recent primer Hardin and Kloke, 2017 provides a brief overview of common statistical techniques, including non-parametric alternatives to t-tests and ANOVAs.
Recently, fields such as psychology have been moving away from a reliance on t-tests and ANOVAs towards more informative techniques, including effect sizes, confidence intervals and meta-analyses (Cumming, 2014). While p-values focus on whether the difference is statistically significant, effect sizes answer the question: "how big is the difference?" A published tutorial provides more details on how to calculate effect sizes for t-tests and ANOVA (Lakens, 2013). Presenting confidence intervals provides more information about the uncertainty of the estimated statistic (i.e., mean, effect size, correlation coefficient). A guide to robust statistical methods in neuroscience examines a variety of newer methods to address the problems with hypothesis tests, and includes information on techniques that are suitable for studies with small sample sizes (Wilcox and Rousselet, 2018). Small, underpowered studies frequently produce inconclusive results that may appear to be contradictory. Meta-analyses combine these divergent results to provide a comprehensive assessment of the size and direction of the true effect (Cumming, 2014).
The findings of the present study highlight the need for investigators, journal editors and reviewers to work together to improve the quality of statistical reporting in submitted manuscripts. While journal policy changes are a common solution, the effectiveness of policy changes is unclear. In a study of life sciences articles published in Nature journals, the percentage of animal studies reporting the Landis 4 criteria (blinding, randomization, sample size calculation, exclusions) increased from 0% to 16.4% after new guidelines were released (Macleod and The NPQIP Collaborative group, 2017). In contrast, a randomized controlled trial of animal studies submitted to PLoS One demonstrated that asking authors to complete the ARRIVE checklist at the time of submission had no effect (Hair et al., 2018). Some improvements in reporting of confidence intervals, sample size justification and inclusion and exclusion criteria were noted after Psychological Science introduced new policies, although this may have been partially due to widespread changes in the field (Giofrè et al., 2017). A joint editorial series published in the Journal of Physiology and British Journal of Pharmacology did not improve the quality of data presentation or statistical reporting (Diong et al., 2018). Statistical reporting requirements are not standard practice for many fields and journals in basic biomedical science, thus limiting the ability of readers to critically evaluate published research.
Other possible solutions to improve reporting include strengthening and implementing reporting guidelines, and training editors, reviewers and investigators to recognize common problems. Box 2 lists statistical information that should be reported when presenting data that were analyzed by t-tests and ANOVA. Some journals have already begun offering unlimited word counts for methods sections to improve reporting (Nature, 2013), while others suggest putting additional information in supplemental methods. Creating open-source software programs that calculate word counts for the results section after excluding statistical information may also facilitate transparent reporting of statistical results. Encouraging public data archiving or interactive graphics that include all data (Ellis and Merdian, 2015; Weissgerber et al., 2016b; Weissgerber et al., 2017) may also strengthen reporting and reproducibility while facilitating data re-use.
Materials and methods
Systematic review of literature
Methodology for the systematic review was similar to the approach outlined in our previous paper (Weissgerber et al., 2015). Physiologists perform a wide range of studies involving humans, animals and in vitro laboratory experiments; therefore we examined original research articles that were published in June 2017 in the top 25% of journals (n = 21) in the Physiology category in Journal Citation Reports as determined by 2016 journal impact factor; six journals that only publish review articles and one journal that did not publish a June issue were excluded. Each phase of screening and data abstraction was performed by two independent reviewers (TLW, OGV). Disagreements were resolved by consensus. Both reviewers screened all articles published in each journal between June 1 and June 30, 2017 to identify full length, original research articles (Figure 1 and Supplementary file 1). Full text articles were then reviewed and papers were excluded if they did not include new data, did not have a continuous outcome variable, or did not include an analysis of variance (ANOVA) or t-test. Eligible manuscripts and supplements were reviewed in detail to evaluate the following questions according to a predefined protocol (Supplementary file 2). This systematic review was conducted in accordance with those elements of the PRISMA guideline (Liberati et al., 2009) that are relevant to literature surveys.
Questions asked for papers that included ANOVAs
Request a detailed protocolWhat was the maximum number of factors included in any ANOVA performed in the paper?
Could the names of factors that were included in each ANOVA be determined from the text, tables or figures?
Did the paper report using a repeated measures ANOVA?
Did the authors specify whether each factor was included in the ANOVA as a between–subjects (independent) or within-subjects (non-independent) factor?
Did the paper specify which post-hoc tests were performed?
If ANOVA was performed but the paper did not mention including repeated measures, within-subjects factors, or non-independent factors, did the paper include any analyses that appeared to require a repeated measures ANOVA (i.e., longitudinal data or other non-independent data)?
If the paper reported using a maximum of one factor in ANOVAs, was ANOVA used to compare groups that could be divided into two or more factors?
Did the paper report F-statistics, degrees of freedom and exact p-values when describing ANOVA results?
Questions asked for papers that included t-tests
Request a detailed protocolDid the paper specify whether paired or unpaired t-tests were used for each analysis?
Did the paper specify whether unpaired t-tests assumed equal or unequal variance for each analysis?
Did the paper report t-statistics, sample size or degrees of freedom, and exact p-value for data analyzed by t-test?
Statistical analysis
Request a detailed protocolData are presented as n (%). The objective of this observational study was to assess standard practices for reporting statistical methods and results when data are analyzed by ANOVA; therefore no statistical comparisons were performed. Summary statistics were calculated using JMP (10.0.0, SAS Institute Inc., Cary, NC). Ethical approval was not required.
Data availability
All data from the systematic review has been uploaded with the manuscript, along with the abstraction protocol.
References
-
The new statistics: why and howPsychological Science 25:7–29.https://doi.org/10.1177/0956797613504966
-
statcheck: Extract statistics from articles and recompute p valuesstatcheck: Extract statistics from articles and recompute p values, 1.2.2, http://CRAN.R-project.org/package=statcheck.
-
Transparency is the key to qualityJournal of Biological Chemistry 290:29692–29694.https://doi.org/10.1074/jbc.E115.000002
-
Reporting on statistical methods to adjust for confounding: a cross-sectional surveyAnnals of Internal Medicine 136:122–126.https://doi.org/10.7326/0003-4819-136-2-200201150-00009
-
Erroneous analyses of interactions in neuroscience: a problem of significanceNature Neuroscience 14:1105–1107.https://doi.org/10.1038/nn.2886
-
The prevalence of statistical reporting errors in psychology (1985-2013)Behavior Research Methods 48:1205–1226.https://doi.org/10.3758/s13428-015-0664-2
-
WebsiteSubmission guidelines: data presentation in graphsPLoS Biology. Accessed December 15, 2018.
-
The use of statistics in medical research: A comparison of the New England Journal of Medicine and Nature MedicineThe American Statistician 61:47–55.
-
Data visualization, bar naked: A free tool for creating interactive graphicsJournal of Biological Chemistry 292:20592–20598.https://doi.org/10.1074/jbc.RA117.000147
-
A guide to robust statistical methods in neuroscienceCurrent Protocols in Neuroscience 82:8.42.1–8.42.8.https://doi.org/10.1002/cpns.41
Decision letter
-
M Dawn TeareReviewing Editor; University of Sheffield, United Kingdom
-
Peter A RodgersSenior Editor; eLife, United Kingdom
In the interests of transparency, eLife includes the editorial decision letter and accompanying author responses. A lightly edited version of the letter sent to the authors after peer review is shown, indicating the most substantive concerns; minor comments are not usually included.
Thank you for submitting your article 'Why We Need to Report More Than "Data were Analyzed by t-tests or ANOVA"' to eLife for consideration as a Feature Article. Your article has been reviewed by three peer reviewers, including Dawn Teare as the Reviewing Editor and Reviewer #1, and the evaluation has been overseen by Peter Rodgers, the eLife Features Editor. The following individuals involved in review of your submission have agreed to reveal their identity: Andrew Althouse (Reviewer #2); Glenn Begley (Reviewer #3).
The reviewers have discussed the reviews with one another and the Reviewing Editor and Features Editor have drafted this decision to help you prepare a revised submission.
Summary:
This paper is a systematic review of 328 papers published in June 2017 in 21 physiology journals. The authors focused on the use of t-tests and ANOVA. They conclude that key information was routinely absent. Similar studies have been published in the past that describe the problems with statistical analysis of scientific papers. However, with the change in Guidelines to Authors instituted by many journals over recent years, it might have been hoped that the situation had improved. Sadly, that does not appear to be the case. The paper includes several figures that demonstrate the challenges that arise when data is inappropriately analysed: these are very useful. The authors are to be congratulated on a clear, well-written, compelling study.
Essential revisions:
Reviewer #1:
a) Given the authors are stating that reporting initiatives are urgently needed, it is a shame that they did not use the PRISMA guidelines to draft the manuscript. There are many reporting initiatives out there, we don't need new ones but rather we need to know how the existing ones can be improved. This paper has been written without much reference to those other initiatives.
b) The manuscript selects instances where a t-test or an ANOVA have been performed. There is no mention of the use of non-parametric tests. Although there is some discussion of how to optimally use an ANOVA to examine interactions, the work tends to focus on being able to replicate exactly what has been done by providing more details. The article would benefit from some discussion of how to select the optimal analysis strategy given a research hypothesis.
c) The checklist provided in box 2 does not have prompts for effect sizes and confidence intervals to be reported. Many of the new reporting guidelines that have been proposed recently directly encourage these to be reported rather than the F-test values and degrees of freedom. This is also missing from the ANOVA section. Again the article would benefit from some discussion of comparative statistics and confidence intervals.
d) The final section ('Transparency: Where should we draw the line?') is missing the idea of reproducibility. Transparency is important for reproducibility. I would suggest including the following recommendation: There should be sufficient detail in a paper so that: i) a reader can understand why the author has selected the analysis methods they have; ii) a reader can repeat the analysis and get the same answer (if they have the raw data).
e) Please expand the figure captions to better explain what is shown in each figure.
https://doi.org/10.7554/eLife.36163.020Author response
Essential revisions:
Reviewer #1:
a) Given the authors are stating that reporting initiatives are urgently needed, it is a shame that they did not use the PRISMA guidelines to draft the manuscript. There are many reporting initiatives out there, we don't need new ones but rather we need to know how the existing ones can be improved. This paper has been written without much reference to those other initiatives.
We have added a statement to the Materials and methods that the systematic review was conducted in accordance with all relevant aspects of the PRISMA guidelines and included a PRISMA checklist. We have also integrated the SAMPL guidelines for statistical reporting in the Introduction. The SAMPL guidelines are very general and may not include adequate information for scientists with little or no statistical training to determine what details should be reported. This paper is designed to provide basic biomedical scientists with more information about why it is important to include additional information so that readers can determine whether an appropriate type of ANOVA or t-test was performed. While we focus on t-tests and ANOVA because they are the most common, the same principles apply to other types of tests.
We always follow all relevant aspects of the PRISMA guidelines as part of our standard protocol for conducting systematic reviews. However, it is important to note that large portions of the guidelines do not apply to literature surveys or to systematic reviews without a meta-analysis. For example, search terms are not included because no selective electronic search was performed. Journals were identified by selecting the top 25% of journals, according to 2016 impact factor, in the physiology category of the Journal Citation Reports database. Articles were then identified by examining journal websites to identify all articles in issues published in June 2017. This process was completed by two independent reviewers. The PRISMA guidelines recommend a structured Abstract, however this contradicts this journal’s requirements for features articles. Elements such as PICO, risk of bias assessments, and reporting of elements relevant to meta-analyses are not relevant to this literature survey.
b) The manuscript selects instances where a t-test or an ANOVA have been performed. There is no mention of the use of non-parametric tests. Although there is some discussion of how to optimally use an ANOVA to examine interactions, the work tends to focus on being able to replicate exactly what has been done by providing more details. The article would benefit from some discussion of how to select the optimal analysis strategy given a research hypothesis.
We chose to focus on t-tests and ANOVA for two reasons. First, while t-tests and ANOVA are very common, our previous work has shown that non-parametric tests are not. We examined articles published in the top 25% of physiology journals during a three-month period in 2014 (Weissgerber et al., 2015). We found that 78.1% of studies used only parametric tests to compare continuous data (i.e. t-tests and ANOVA), 13.6% used a combination of parametric and non-parametric tests, and 3.8% used only non-parametric tests. We have now described this data in the manuscript. Second, there are many different types of ANOVAs and t-tests; therefore additional detail is needed to determine which test was performed. In contrast, the name of the non-parametric test (i.e. Kruskal-Wallis, Mann Whitney, Wilcoxon Rank Sum, Wilcoxon Signed Rank) is sufficient because these tests do not have variations.
We understand the reviewers’ desire for a single paper that outlines the problems with the reporting of existing analyses, addresses the misconceptions that lead to these reporting errors and shows how to correct them, and also describes how to select more informative or optimal tests. However, it is important to be realistic about what can be accomplished in a single paper designed for basic biomedical scientists, many of whom have limited or no statistical training. There are several papers that address the problems with t-tests and ANOVA and describe how to select more informative alternatives. Although these papers tend to be quite long, the authors frequently note that they are intended to supplement existing statistical knowledge and are not a substitute for statistical training. We have rewritten the last section of the paper to briefly address other approaches and referred readers to existing resources for additional information. A shift away from hypothesis testing in basic biomedical science will require retraining the scientific workforce, which will take time. It is likely that most investigators will continue to perform t-tests and ANOVA in the near future; hence, efforts to improve reporting for these techniques are needed.
c) The checklist provided in box 2 does not have prompts for effect sizes and confidence intervals to be reported. Many of the new reporting guidelines that have been proposed recently directly encourage these to be reported rather than the F-test values and degrees of freedom. This is also missing from the ANOVA section. Again the article would benefit from some discussion of comparative statistics and confidence intervals.
We have updated Box 2 to include effect sizes and confidence intervals and added a section at the end of the manuscript that addresses other statistical approaches and provides links to papers that examine these resources in detail. This includes a citation on how to calculate effect sizes for t-tests and ANOVA.
d) The final section ('Transparency: Where should we draw the line?') is missing the idea of reproducibility. Transparency is important for reproducibility. I would suggest including the following recommendation: There should be sufficient detail in a paper so that: i) a reader can understand why the author has selected the analysis methods they have; ii) a reader can repeat the analysis and get the same answer (if they have the raw data).
These are both included in the SAMPL guidelines, which we have now mentioned in the Introduction. Additionally, these points are also both mentioned in the first sentence of the final section of the paper, which has been extensively revised and is now entitled “Moving towards a more transparent and reproducible future”. This section also includes a brief discussion on more informative analysis techniques and links to resources and integrates the concept of reproducibility.
e) Please expand the figure captions to better explain what is shown in each figure.
We have added additional descriptors to figure legends.
https://doi.org/10.7554/eLife.36163.021Article and author information
Author details
Funding
American Heart Association (16GRNT30950002)
- Tracey L Weissgerber
National Center for Advancing Translational Sciences (UL1 TR000135)
- Tracey L Weissgerber
Mayo Clinic (Robert W Fulk Career Development Award)
- Tracey L Weissgerber
National Cancer Institute (R03-CA212127)
- Stacey J Winham
Walter and Evelyn Simmers Career Development Award for Ovarian Cancer Research
- Stacey J Winham
The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Publication history
- Received:
- Accepted:
- Accepted Manuscript published:
- Version of Record published:
Copyright
© 2018, Weissgerber et al.
This article is distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use and redistribution provided that the original author and source are credited.
Metrics
-
- 24,007
- views
-
- 2,363
- downloads
-
- 69
- citations
Views, downloads and citations are aggregated across all versions of this paper published by eLife.
Citations by DOI
-
- 69
- citations for umbrella DOI https://doi.org/10.7554/eLife.36163







